With the advent of numerous gadgets that require considerable strain from human eyes, the development of eye pathologies has become more frequent.
According to statistics, conjunctivitis is the most common among all eye diseases. Such pathologies are an inflammatory process affecting the area of the eye called the “conjunctiva”. With proper and timely treatment, getting rid of conjunctivitis is not so difficult, but for this it is important to know the peculiarities of the course of the disease.
More details about them and the general essence of conjunctival pathologies will be discussed in today’s article, as well as on the pages of the section of the same name on our resource. Want to know more about conjunctivitis? Then be sure to read all the information provided.
Causes
There are several factors that contribute to the development of inflammation in the mucous membrane of the eyes. The most common causes of conjunctivitis in adults are:
- Bacteria. Bacterial lesions of the conjunctiva occur due to infection through contact and household contact. The causative agents of the disease are staphylococci, pneumococci, streptococci, Escherichia coli and Pseudomonas aeruginosa, and Mycobacterium tuberculosis. The organs of vision may be damaged by pathogens of gonorrhea, syphilis, and diphtheria.
- Viruses. Viral conjunctivitis is highly contagious and is transmitted by airborne droplets, less commonly by household contact. The disease is caused by adenoviruses, herpes viruses, chickenpox, measles, and enteroviruses.
- Allergy. Allergic conjunctivitis develops due to the body's high sensitivity to any allergen, and is often a local manifestation of a general allergic reaction. The causes of allergic inflammation of the conjunctiva are medications, food, household chemicals, and pollen.
- Chlamydia. Chlamydial damage to the organs of vision in adults is rare, as a rule, it is combined with diseases of the genitourinary system: urethritis (inflammation of the urethra) and prostatitis (inflammation of the prostate gland) in men, vaginitis (inflammation of the vaginal mucosa) and cervicitis (inflammation of the cervical tissue) - among women.
- Fungi. Fungal inflammation of the conjunctiva is caused by mold, yeast and other types of fungi. The development of fungal infections is facilitated by poor hygiene when wearing contact lenses, microtrauma, diabetes mellitus, and decreased immunity.
- Injuries. Non-infectious conjunctivitis occurs when the organs of vision are damaged by chemical and physical factors, smoke, dust, and ultraviolet rays.
Note! Conjunctivitis in adults is the most common inflammatory disease of the organs of vision. The frequency of damage to the conjunctiva is associated with its high sensitivity to infections, as well as the accessibility of the conjunctival cavity to the adverse effects of external factors.
Pathogenesis
The mucous membrane of the eyes performs a protective function, and due to its anatomical position, it is constantly in contact with many external irritants - dust particles, air, microbes, ultraviolet radiation. Normally, the conjunctiva is transparent and has a smooth, moist surface.
Under the influence of irritating factors, a pronounced inflammatory reaction occurs: the conjunctiva turns red, the eyelids and transitional folds swell, and a mucous or purulent secretion begins to be released from the conjunctival sac. The inflammatory process is accompanied by pain, pain, photophobia, and blepharospasm (involuntary closure of the eyelids).
The structure of the conjunctiva of the eye
The conjunctiva is located on the inside of the eyelids and the front of the eyes, ending at the cornea. The area is represented by a mucous membrane penetrated by nerves and blood vessels. She is very sensitive and susceptible to irritation from negative factors.
The conjunctiva performs the following functions:
- protection of the internal structures of the eyes from the effects of damaging environmental factors;
- interaction with the lacrimal fluid, which helps moisturize the mucous membrane;
- nutrition of eye tissues through blood;
- transmission of light rays into the lens and retina.
In the corner of the eye, the conjunctiva forms a cavity that contains microcirculation vessels and tear fluid. This formation is called the conjunctival sac.
This shell consists of two layers:
- superficial, consisting of epithelial cells;
- deep, which contains lymphoid tissue and glands that secrete secretions from tear fluid, mucin, and lipids.
Under the influence of negative environmental factors, both superficial and deep layers can become inflamed. The symptoms of the disease depend on this.
Symptoms and classification
Clinical manifestations of the inflammatory process in the mucous membrane of the eyes depend on the etiological form of the disease. However, the course of conjunctivitis of various origins is characterized by a number of common symptoms. These include:
- swelling, redness of the mucous membrane of the eyelids and transitional folds;
- discharge of mucous or purulent secretion;
- itching, burning, lacrimation;
- sensation of “sand” or foreign body in the eyes;
- photophobia;
- blepharospasm.
As a rule, with conjunctivitis in adults, body temperature remains normal, in some cases it can rise to subfebrile values (37.5-38 ºC).
Inflammatory diseases of the conjunctiva in adults are classified according to the following criteria: source of infection, course, nature, cause of inflammation. Depending on the source of infection, endogenous and exogenous conjunctivitis are distinguished:
- endogenous - secondary lesions of the conjunctiva that occur against the background of other diseases (natural and chickenpox, ARVI, hemorrhagic fever, tuberculosis);
- exogenous - develop as an independent pathology due to direct contact of the mucous membrane with an infectious agent or allergen.
Based on the nature of inflammation, the following types of conjunctivitis are distinguished:
- purulent - develop when affected by bacteria, characterized by a severe, protracted course;
- fibrinous (membranous) - manifested by the formation of fibrinous films that partially or completely cover the mucous membrane of the eye;
- catarrhal - occurs with severe redness of the conjunctiva and swelling of the eyelids, severe lacrimation, burning, pain in the eyes;
- follicular - occurs due to viral lesions, the distinctive feature is the formation of follicles (small nodules) on the conjunctiva and eyelids.
According to the course, conjunctivitis in adults is divided into:
- acute – begins suddenly, lasts on average from 7 to 14 days;
- subacute – characterized by less pronounced symptoms, prolonged course (longer than three weeks);
- chronic - develop gradually, are characterized by a persistent long-term course, are difficult to treat, and often lead to serious complications.
Due to inflammation, conjunctivitis is classified into:
- bacterial;
- viral;
- allergic;
- chlamydial;
- fungal;
- traumatic.
The most common types of conjunctivitis found in adults are allergic, bacterial, viral, purulent and acute conjunctivitis, which differ in clinical manifestations, nature of inflammation, and course.
Allergic
Symptoms of allergic inflammation usually appear immediately after contact with the allergen, sometimes several hours may pass before the first signs of illness appear. Typically, allergic conjunctivitis affects both eyes. The main symptoms of the disease are:
- severe itching;
- swelling of the eyelids;
- redness of the conjunctiva;
- lacrimation;
- photophobia.
Often, allergic inflammation of the organs of vision tends to have a protracted, chronic course with periods of remissions and exacerbations, and is also combined with other manifestations of allergies: skin rashes, itching, sneezing, runny nose, cough.
Bacterial
A bacterial infection usually develops in one eye and moves to the other after 1-3 days. Specific manifestations of bacterial inflammation are:
- viscous purulent discharge from the eyes of a yellowish or greenish color;
- severe pain syndrome;
- dryness of the mucous membrane and skin of the periorbital region;
- formation of crusts on eyelashes.
Note! Purulent discharge from the eyes can be a sign of fungal or chlamydial conjunctivitis. To establish the exact cause of the disease and receive adequate treatment, you must consult an ophthalmologist.
Viral
Viral conjunctivitis usually occurs against the background of upper respiratory tract infections and is accompanied by the following symptoms:
- moderate lacrimation;
- photophobia;
- blepharospasm;
- scanty mucous discharge;
- enlarged submandibular or parotid lymph nodes.
With some viral infections, follicles (follicular form) or films (fibrinous form) form on the conjunctiva.
Purulent
A characteristic symptom of a purulent lesion is copious discharge of pus from the conjunctival sac. In this regard, patients complain of:
- sticking of eyelashes;
- difficulty opening your eyes, especially in the morning;
- pain and burning in the eyes;
- swelling of the eyelids.
A purulent inflammatory process develops with bacterial and fungal infections, chlamydia lesions. In the absence of timely treatment, it can occur due to eye injuries.
Spicy
Acute conjunctivitis begins suddenly with pain and stinging in the eyes. Against the background of redness of the conjunctiva, pinpoint hemorrhages are often observed. Other symptoms of acute inflammation include:
- swelling of the eyelids;
- copious mucous, mucopurulent or purulent discharge;
- general malaise;
- headache;
- sometimes – a slight increase in body temperature.
The duration of the disease varies from one to three weeks, with an average of 10-14 days.
Conjunctiva. Conjunctival membrane.
The conjunctiva is an interesting anatomical formation. Its function of tear production allows you to see, and in addition, it reliably protects the eyeball.
Conjunctiva is a word that comes from Latin and means the connective membrane of the eye. It is a thin and transparent shell that is designed to cover the back surface of the eyelids. It forms the fornix of the conjunctival sac, making the transition to the anterior surface of the eyeball. It ends at the limbo. The conjunctival epithelium will clearly transition to the cornea. The tarsal part, tightly fused with the tissue and mobile - orbital, like a transitional fold, are located in the conjunctiva.
Double-layered columnar epithelium represents the surface of the conjunctiva of cartilage. At the edge of the eyelids it contains goblet cells, and the crypts of Henle at the distal end of the cartilage, they secrete mucin. Reticular tissue is located under the epithelium, it is fused to the cartilage very firmly. The submucosa is almost completely absent, which does not allow the conjunctiva to move, which leads to the formation of a distance above its surface.
Meibomian glands are visible through it normally. From them a transparent pattern emerges, reminiscent of a vertical picket fence. On the lower eyelid you can count up to thirty of them, and on the upper eyelid more. The fatty secretion is produced by the meibomian glands, which prevents tears from overflowing over the edge of the eyelid. An internal stye or chalazion develops when the outer eyelid is blocked. Stye and chalazion are treated with different methods and you need to know this. Complete removal of the contents requires removal of the chalazion. Sanitation of the capsule must be strict, using 5% iodine, otherwise there is a risk of chalazion recurrence.
The free edge of the conjunctiva is smooth, but moving a few mm away from it, roughness is felt. A 5-6-layer columnar epithelium with numerous goblet mucous cells that secrete mucin covers the conjunctiva of the transitional fold. Loose subepithelial connective tissue, which consists of elastic fibers, includes lymphocytes and plasma cells that form clusters in the form of lymphomas or follicles. This part remains mobile due to the pronounced subconjunctival tissue. Foreign bodies may not be noticed when they are in swollen folds of the arches, so you need to keep this quality in mind. You should look for a foreign body using different lighting options and different colors. The task becomes more complicated if the foreign body is transparent.
A wet bath is used to remove such a body. Additional lacrimal glands are located on the border between the orbital and tarsal parts. Three of them are located at the top in the edge of the upper cartilage, and one is lower than the lower cartilage, in the area of the arches. On the upper eyelid there are from 15 to 40 the last named glands, and on the lower eyelid there are 6-8. Their structure is identical to the main lacrimal gland; its excretory ducts open in the upper fornix, or more precisely in its temporal part.
The tear-producing glands of the eyeball can produce no more than three ml of tears in 24 hours. The upper as well as the lower bays of the conjunctival sac, at the point where the conjunctiva of the eyelids pass into the conjunctiva of the eyeball, look like blind pockets, and they are called the conjunctival fornix.
The upper conjunctival fornix has a depth of 10 mm, and if the eyelids are closed, then 20-25 mm. The lower conjunctival fornix is 8 mm, when the eyelids are closed - 11-13 mm. Eyelid lifters are used to inspect the arches. Double eyelid inversion is necessary for chemical burns.
The posterior leg of the levator approaches the conjunctival fornix. The fascial layers and Tenon's capsule are connected to the conjunctiva of the fornix. They extend from the outside with the help of layers of muscles. When the muscle tendons are exposed, the conjunctiva is separated first, followed by Tenon's capsule.
Squamous epithelium covers the conjunctiva of the eyeball. It easily moves along the surface of the sclera, since it is loosely connected to it. Particles of columnar epithelium, which include secreting Becher cells, are included in the limbal part. Manz cells, which produce mucin, are located radially to the limbus; they have the shape of a belt 1 - 1.5 mm wide.
Diagnostics
The diagnosis is made by an ophthalmologist based on the patient’s complaints and clinical manifestations of the disease. History data (contact with sick people, allergies, injuries) help determine the cause of the disease. An external examination reveals redness, swelling of the conjunctiva, mucous or purulent discharge from the conjunctival sac. To determine the infectious agent or allergen, the following laboratory tests are performed:
- cytological and bacteriological examination of scrapings from the conjunctiva;
- determination of antibody titer (IgA and IgG) to the suspected pathogen in tear fluid or blood serum;
- examination for the presence of demodex mites;
- skin allergy tests.
Differential diagnosis of infectious or allergic lesions of the conjunctiva is carried out with other inflammatory diseases of the organs of vision, an attack of glaucoma, and a foreign body of the eye.
Diagnosis and treatment of conjunctivitis
Diseases of the conjunctiva cause discomfort
Conjunctivitis is the most common eye pathology, observed in approximately 30% of all visitors to the ophthalmologist's office.
The high prevalence of such pathologies makes them extremely easy to diagnose diseases. Surprisingly, a person is diagnosed with conjunctivitis immediately after a detailed examination.
Direct diagnostic procedures are used to identify the exact cause of the pathology, which is necessary for organizing the correct and most effective therapy.
Note that in terms of diagnosing conjunctivitis, two types of examinations are mainly used:
- Scraping - that is, taking the affected part of the conjunctiva from the surface of the eye.
- Analysis of biomaterial - as a rule, its subject is ordinary blood.
Based on the results of such studies, the treating specialist is able to find out the causative agent or factor provoking the disease. With this information, the ophthalmologist can already prescribe one or another course of therapy.
As for the treatment of conjunctivitis, in the vast majority of cases it is medicinal in nature. Surgical intervention takes place in three main situations:
- with severe inflammation, which requires removal of part of the connective tissue;
- in the presence of neoplasms in the conjunctiva;
- with the development of tissue dystrophy.
In all other cases, drug therapy is prescribed and is aimed at relieving inflammation. Also, the organized course is necessary to completely eliminate the cause of the development of pathology.
Treatment
Treatment is selected individually by an ophthalmologist depending on the pathogen, the nature of the inflammation, and existing complications.
If a bacterial infection is detected, patients are prescribed antibacterial ointments and eye drops. To treat viral lesions, antiviral agents are used topically. In order to prevent the addition of a bacterial infection, antimicrobial drugs may be additionally prescribed.
If a chlamydial lesion is detected, in addition to local treatment, a course of oral antimicrobial agents is indicated. Therapy for allergic conjunctivitis includes the prescription of vasoconstrictors, antihistamine drops, and hormonal drugs. For conjunctival lesions of fungal origin, antimycotic ointments and instillations (eye drops) are prescribed.
Regular eye care plays a big role in a speedy recovery. Before each application of ointment or instillation, it is necessary to thoroughly rinse the eyes, use disposable towels and napkins, separate pipettes and eye sticks. In case of inflammatory diseases of the conjunctiva, it is forbidden to apply bandages, as they prevent the discharge of secretions and can cause the spread of infection.
Complications
Correct timely treatment of conjunctivitis avoids the spread of inflammation and prevents the development of complications. In the absence of therapy or late initiation of treatment, the disease leads to the following complications:
- keratitis – inflammation of the cornea of the eye, which causes clouding, formation of ulcers, and decreased visual acuity;
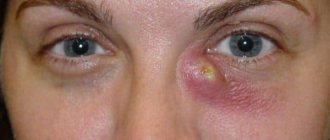
- dacryocystitis (inflammation), abscess or phlegmon (purulent lesions) of the lacrimal sac;
- blepharitis - an inflammatory process in the ciliary edge of the eyelids;
- orbital cellulitis - inflammation of the tissues located behind the orbital septum.
Note! Advanced acute conjunctivitis becomes a chronic form, which is difficult to treat, often causes a sharp deterioration in vision, and in severe cases leads to blindness.