Many anomalies, pathological conditions and processes in the orbital region are accompanied by insufficient hydration of the conjunctiva (the thin mucous membrane of the eye and the inner surfaces of the eyelids) and, what is even more dangerous, drying out of the cornea (the transparent area of the outer dense sclera, which acts as a “viewing hatch” in front of the pupil) . Symptom complexes caused by such drying out are known under the names “kerato-conjunctival xerosis”, “keratomalacia” or simply “dry eye syndrome” (DES). Epidemiological statistics regarding this syndrome covers, according to various estimates, from 9% to 18% of the world's population, reveals a predominance of women (up to 70% of all diagnosed cases) and is in direct correlation with age: persons under 50 years old account for no more than 12 % of the total number of cases.
The normal natural hydrodynamics of the eye are quite complex. Constant contact of open areas of the eyeball with oxidizing (and drying) air oxygen requires special protection. This problem in the course of evolution was solved, firstly, at the biochemical, and secondly, at the biomechanical levels. Thus, the composition of the tear film, which normally should be constantly present on the surface of the eye in the form of a lubricant layer 10 microns thick, includes:
- mucous-oily hydrophobic secretion of the meibomian glands (minimizes friction during blinking, prevents the evaporation of the underlying molecular layers of the tear film);
- a hydrophilic liquid layer, saturated with ions and organic mediators (acts as a local immune barrier and disinfectant when removing small foreign particles, transports nutritional compounds and oxygenation, i.e. saturates the corneal tissue with bound oxygen);
- mucin layer produced by epithelial and goblet cells (directly adjacent to the cornea, it provides additional “polishing”, fills and smoothes microscopic gaps, bubbles and protrusions; the refractive power of the mucin layer is normally such that the image transmitted by the cornea is as clear and saturated as possible).
This biochemical solution would be useless or too wasteful for the body (in other words, all the glands would work in an enhanced mode and tears would flow down the eye in a continuous stream), if nature had not found an amazing mechanism for mechanical interruption. Millions of years later, it was reproduced by the automotive industry in windshield wiper systems, the intensity of which depends on external conditions: during drizzling rain, the operation interval is much longer than during rain. Similarly (or rather, being a prototype of this), the eyelids are “triggered” by a blink reflex with a frequency of about 0.1 hertz (once every 10 seconds), renewing the tear film and applying the next uniform three-component layer to the surface of the eyeball. Considering the above-mentioned most important functions of the tear lubricant, it is easy to imagine the danger posed by the heterogeneity, insufficiency or absence of the protective layer. With dry eye syndrome, this danger becomes a clinical reality.
Reasons for the development of dry eye syndrome
Dry eye syndrome is most often based on a deficiency of tear fluid and/or disturbances in its composition (which leads, for example, to increased or accelerated evaporation) due to insufficient or improper secretory activity of the corresponding glands. In turn, this may be a consequence of a number of autoimmune and endocrine disorders (for example, Sjögren’s and Felty’s syndromes, lymphoma, etc.), renal failure, infectious and inflammatory processes, dermatological diseases, general asthenia of the body, as well as hormonal changes, in particular during pregnancy or menopause.
Provoking factors-conditions for dry eye syndrome in the organ of vision include chronic inflammation (for example, conjunctivitis, keratitis or combinations thereof), lagophthalmos (non-closure of the eyelids), neuroparalysis, cicatricial deformities, previous ophthalmic surgical operations (kerato- or conjunctival plastic surgery, elimination of ptosis, keratotomy etc.), as well as diseases of the lacrimal glands themselves.
Risk factors, which are a constant tough “strength test” for the tear film, can be: indoor air overdried by air conditioners or thermoradiators, continuous concentration of attention for many hours on a computer monitor or television screen, incorrect selection of glasses or contact lenses, numerous environmental hazards (dust , arid climate, chemical or mechanical aggressive suspensions in the air, radiation, intense ultraviolet in the lighting spectrum, etc.). Inhibition (suppression) of the production of tear fluid or its individual components can be caused by prolonged use of drugs belonging to certain pharmacological groups: adrenergic blockers, analgesics, anesthetics, anticholinergics, hormone-containing drugs (especially contraceptives), anhistamines and antihypertensive medications.
Finally, some congenital idiopathic features (for example, an increased interval of the blink reflex), vitamin deficiency in the body, a hereditary factor, as well as the old age and female gender mentioned at the beginning of the article, can contribute to the development of dry eye syndrome. Sometimes DES is caused by disruptions in the reflex circuit: for example, due to some functional disorder or organic changes, the self-protective sensitivity of the cornea is reduced, and the neural command to blink is given less frequently than is objectively necessary.
Natural eye hydration
In normal condition, the eyeball is covered with a thin tear film, which consists of three layers:
- Lipid (external). Consists of an oily secretion secreted by the meibomian glands. It ensures the sliding of the eyelid, prevents the evaporation of moisture, as well as heat transfer from the surface of the epithelium of the cornea and conjunctiva.
- Aqueous (medium), forms the basis of the tear film. Responsible for supplying the eye tissue with oxygen and nourishing it. Removes dead cells and metabolic products from the surface of the eyeball.
- Mucinous (internal). Responsible for giving the hydrophobic epithelium of the cornea hydrophilic properties, allowing it to retain the tear film on the cornea.
Normally, the tear film, which is less than 10 micrometers thick, is renewed every 10 seconds. But against the background of disruption of the processes of physiological renewal of the tear film and its stability, dry eye syndrome may develop.
Classification of the disease
There are three variants of dry eye syndrome, caused, respectively, by a) hyposecretion of tear fluid, b) abnormally high volatility, and c) a combination of the first two factors. According to the etiological criterion, syndromic (as an independent disease), symptomatic (as a consequence of other pathologies) and artificial (artificial, provoked by external influences) types are distinguished. The clinical picture, type of course, prognosis and consequences can also vary widely: most often these are all kinds, including ulcerating or eroding inflammatory processes in the conjunctiva and cornea. Finally, dry eye syndrome is classified according to severity, from mild to severe.
Symptoms
Dry eye syndrome can present with a wide variety of individual symptoms. Classic clinical manifestations include dry burning and gritty pain in the affected eye, foreign body sensation, increased (and useless) lacrimation, painfully heightened reaction to bright light, blurred vision, asthenopia (eye fatigue), redness, a variety of discomfort and pain on palpation , washing, instillation, etc. As a rule, there is a worsening of the existing symptom complex in the evening, in the cold or in strong winds, with more or less prolonged visual concentration, as well as in dry, smoky or dusty rooms.
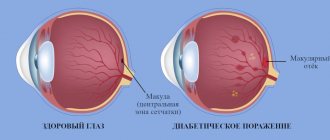
When examining, the ophthalmologist pays attention to organic changes in the conjunctiva and cornea specific to xerosis (the presence and nature of the so-called tear menisci), a tendency to “stick” during the act of blinking, displacement of the swollen edematous conjunctiva, erosions, signs of filamentous keratitis, etc. In some severe forms, signs of not only inflammation, but also degeneration are observed: a decrease in the transparency, smoothness, and uniformity of the corneal layer, its excavation (“pitting”), a decrease in the natural shine of the eyes, and hyperemia. The recurrent erosive variant is manifested by periodic microscopic ulcers on the cornea, which heal within a few days, but leave behind long-lasting discomfort.
A particularly severe degree of keratoconjunctival xerosis can develop as a result of chronic complete or partial non-closure of the eyelids. A profound deficiency of vitamins A results in scaly metaplasia of the corneal epithelium and keratin degeneration of the conjunctiva. In many cases, dry eye syndrome is accompanied by inflammation of the eyelids (blepharitis). In the absence of timely and adequate treatment, the outcome of dry eye syndrome can be irreversible destructive changes in the cornea, including perforation.
Diagnostics
The above and other known manifestations of dry eye syndrome serve as primary diagnostic criteria for the ophthalmologist. Of great importance for establishing a diagnosis is also the analysis of complaints, heredity, life history, and the dynamics of the disease. In general, a pathognomonic (inherent only to this disease and not typical for others) clinical picture is usually collected, which allows reliably diagnosing dry eye syndrome. Additional informative signs may include the dermatological and motor status of the eyelids (in particular, the frequency of blinking), the results of a biomicroscopic examination of the tear film, corneal and conjunctival surfaces, tear menisci, etc. A contrast fluorescent test may be prescribed to assess the homogeneity of the tear layer, tests of secretory productivity and volatility of the tear fluid (Schirmer, Norn tests, etc.).
Measurements of the various layers in the “lubricating coating” at the micron level are made in polarized light (thiascopy). If a more in-depth diagnostic examination is necessary, laboratory tests of osmolarity, crystallography, and cytological examination are prescribed. In the presence of background endocrine or autoimmune disorders, the current clinical status of the relevant systems is diagnosed.
Treatment of dry eye syndrome
As with any other painful condition, etiopathogenetic therapy is focused on eliminating its root causes as much as possible. In this case, these may be measures aimed, depending on the etiology, at the biochemical correction of the composition of the tear fluid or at stimulating its secretion, at relieving neurological pathology or compensating for organic changes in the corneal and/or conjunctival tissue. Prevention of complications and relapses is mandatory.
Eye drops
The therapeutic standard for almost any type of dry eye syndrome is the systematic instillation of tear substitutes (artificial tears, as well as in the dosage forms “Vidisik”, “Korneregel”, their analogues and generics) in order to ensure sufficient hydration of the eye membranes and stability of the tear film. The most common eye drops:
- Systane (including “Ultra”, “Balance”, etc.)
- Visine (only “Pure Tear”, but not “Classic”!)
- Artelak ("Splash", "Balance")
- Vizomitin (“Skulachev Drops”) and others
Depending on the severity of the syndrome, eye ointments and gels are selected with the optimal viscosity for a given specific case and with the most effective composition of active substances. Modulating, stimulating and correcting immunity agents, anti-inflammatory drugs are widely used; in case of degenerative tendencies, stimulants and metabolic correctors are used. According to indications, antihistamines (antiallergic) drugs can be prescribed.
Surgical methods
If it is determined that the triggering factor for the development of dry eye syndrome is impaired lacrimal drainage (discharge of waste tear fluid) or obstacles to its flow to its destination, the question of surgical correction and restoration of normal ocular anatomy is raised. Damage to the corneal layer (ulceration, erosion, perforation) is also surgically eliminated; Depending on the specific clinical picture, plastic surgery, obturation (artificial blockage with microscopic silicone plugs), diathermo- or laser coagulation of lacrimal openings, drainage canaliculi on the conjunctiva of the eyelid, or their surgical suturing are used. The obturation technique is considered preferable as it is minimally invasive, quite effective and does not leave irreversible consequences.
For indoor use
A tincture of blue cornflower fish oil will improve the moisture content of the mucous membrane and at the same time enrich it with the necessary vitamins. These ingredients are taken in equal proportions and heated for twenty minutes in a water bath. After this, the resulting mixture is infused for ten days in the dark. It is recommended to take the drug three times a day, one tbsp. l. Fish oil in this recipe can be replaced with flaxseed oil.
If the causes of dry eyes are clear, treatment with folk remedies can be carried out using a decoction of St. John's wort in milk. To do this, take 7 tbsp. prepared medicinal herb. This volume is mixed with a glass of milk and boiled for ten minutes. The decoction is taken twice a day in the mornings and evenings in a volume of 0.5 cups half an hour before meals.
An excellent source of vitamin A, which is very beneficial for the eyes, is carrot juice. It is recommended to take it freshly squeezed in a volume of 150 to 200 ml. To enhance the effect, it is advisable to add a little finely chopped parsley to this juice.
Folk remedies
Traditional medicine recipes recommend using such remedies as aloe juice, a solution of propolis and honey in the form of drops, applying cucumbers and bags of tea to the eyelids. Rinsing the eyes with infusions of chamomile, calendula and eyebright.
However, it is worth understanding that these traditional methods do not help solve the problem, but only lead to infection and allergic reactions, which only aggravates the situation.
Severe dry eye syndrome with a xerotic ulcer or severe keratomalacia may require, if other methods are ineffective (in particular, conservative therapy and/or obstruction of the lacrimal drainage tract), operative keratoplasty. Laser tarsorrhaphy (a high-tech radical technique for suturing the edges of the eyelids) is indicated for non-closure or inadequate closure of the eyelids, an abnormally widened palpebral fissure, or a pathologically rare blink reflex. The latest developments in this area are autotransplantation of salivary glands into the conjunctiva, implantation of special lacrimal reservoirs, etc.
Eyelashes and eyebrows
In addition to the skin around the eyes, the appearance of the eyelashes and eyebrows is also important. Every woman dreams of long fluffy eyelashes. Extensions and professional growth products cost a lot and are not suitable for everyone. Few people know that you can grow eyelashes at home and for a reasonable price. Caring for them will require the following ingredients:
- Castor oil;
- Apricot kernel oil;
- Vitamin Aevit in capsules;
- Clean wooden stick;
- Old mascara brush;
The recipe is extremely simple: you need to mix 50 ml of both oils, carefully pierce the gelatin shell of the Aevit capsule with a needle and squeeze the contents into the oil. Mix the resulting solution thoroughly with a wooden stick. The resulting solution should be placed in the refrigerator door and applied to eyelashes and eyebrows every evening before going to bed, after carefully removing makeup.
In addition to castor oil, eyelash care can be carried out using avocado oil, jojoba oil, burdock oil and wheat germ. It is also important to comb your eyelashes every evening with a special brush. The same applies to eyebrows. Usually, girls' eyebrows are regularly plucked, and in order for them to continue to grow, it is also important to nourish them.
As you understand, you can take care of your eyes at home; it’s easy and inexpensive. It is only important to know some secrets.
Forecast and prevention of dry eye syndrome
Any forms and variants of dry eye syndrome, even its earliest stages and minimally uncomfortable degrees of severity, require intervention, careful diagnosis and an intensive combined therapeutic response; otherwise, the risk of severe and often irreversible damage to the conjunctiva, cornea and adjacent structures is too high, which may result in complete loss of visual function.
Prevention is at least basic “visual hygiene” (including optimization of exercise and rest regimes, simple eye exercises and consciously rapid blinking with constant visual concentration; the use of personal protective equipment in hazardous industries or in unfavorable climatic conditions, proper organization and illumination of the workplace, etc. .).
Of course, in the presence of any chronic diseases and systemic disorders, their constant therapeutic monitoring with timely relief and prevention of exacerbations is necessary. An important preventive role in the prevention of dry eye syndrome is also played by the consumption of the naturally required daily amount of fluid (calculated and recommended by the doctor based on age, body weight and other factors), improving the diet with an emphasis on the variety of composition and sufficient content of vitamins in food.
Healing oils
Oils that need to be slightly warmed before use will help eliminate dry eyes to release their active ingredients. To eliminate the syndrome use:
- Sea buckthorn oil. A small amount of oil should be instilled regularly to eliminate the unpleasant feeling on the part of the visual organs.
- Mustard oil should be lubricated on the eyelids to increase lacrimation.
- Camphor oil should be applied to the eyes to eliminate dryness. First you need to pour it into a spoon and heat it on fire until a little powder remains in the container. It is this powder that is used to rub the eyes, mixed with olive oil;
- Any oil of plant origin should be taken orally to prevent dryness in the organs of vision.
Treatment
Before using oils, you can perform therapeutic exercises. To do this, you need to sit on a chair and blink frequently. After this, you need to rotate your eyeballs clockwise and counterclockwise.
When you feel very tired and a veil appears before your eyes, you should look at the farthest object, then sharply focus your vision in front of you.