Who doesn’t know what conjunctivitis is? Perhaps this is one of the most common eye diseases that almost everyone has encountered in their lives. By what symptoms can it be diagnosed, what causes contribute to its occurrence, and most importantly, how to cure it? You can read detailed answers to these questions in this article.
In this article
- What functions does the conjunctiva of the eye perform?
- What can an examination of the conjunctiva show?
- What types of conjunctivitis are there?
- Causes of allergic conjunctivitis
- Diagnosis and treatment of allergic conjunctivitis
- Symptoms of bacterial conjunctivitis
- How to cure bacterial conjunctivitis?
- Main characteristics of the fungal species
- Diagnosis and therapy of fungal conjunctivitis
- What is a viral type of conjunctivitis?
- Therapy for viral conjunctivitis
- Traumatic form of conjunctivitis
- Prevention of conjunctivitis
What is conjunctivitis or “rabbit eye syndrome”, as this pathology is popularly called? In principle, the “folk” name contains the whole essence of this disease. In medical terms, conjunctivitis affecting the eyes is an inflammation of the conjunctival mucosa, which covers the inner surface of the eyelids and the scleral part of the eyeball, that is, its protein region. Pathology is included in the group of polyetiological diseases. The name polyetiological itself comes from the Greek word “poly”, which translates as many, and “etiology”, that is, cause, origin. Consequently, it becomes clear that conjunctivitis can have very different etymologies, as a result of which it is divided into different types.
What functions does the conjunctiva of the eye perform?
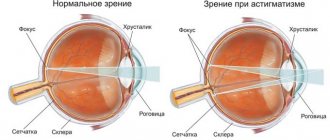
In order for you to have a complete understanding of the pathology we describe, you need to clearly understand what the conjunctiva of the eye is and what its role is in the functioning of the visual organs. Quite often from ophthalmologists you can hear such a formulation as “connective membrane”. This is the conjunctiva - a thin transparent tissue that covers the outside of the cornea and the inner surface of the eyelids. In some way, it protects the eyeball and performs a very important function in the functioning of our visual organs.
For example, the connective membrane guarantees the necessary level of lacrimation and direct distribution of tear fluid over the entire surface of the eye. Thanks to its work, the visual organs are equally moistened, which contributes to clear and precise vision. The conjunctiva ensures the receptivity of the visual organs to light sources and also prevents them from drying out. In addition, the connective membrane reliably protects the eyes from the penetration of microorganisms of various natures, which, in turn, connecting with the cornea, which is sensitive by nature, can become symptoms of many ophthalmological diseases, such as keratitis, blepharitis and conjunctivitis.
The latter disease is considered the most common today. According to rough estimates by experts, various forms of eye conjunctivitis, the treatment of which is carried out under the supervision of ophthalmologists, today affects about 30% of the population, including both children and adults.
What can an examination of the conjunctiva show?
The condition of the conjunctiva is always carefully examined during a visit to the doctor. At best - as part of annual vision prevention, at worst - if symptoms of various ophthalmological diseases are suspected. As the inflammatory pathology progresses, the connective membrane changes noticeably, becoming duller and rougher on the surface. Due to the fact that the conjunctiva is quite thin in structure, it is well supplied with blood and has no pigmentation. In many situations, it is by its appearance that specialists can identify various diseases, including:
- coagulation disorder;
- anemia;
- jaundice;
- pterygium;
- state of shock.
However, the most common pathology of the conjunctiva is a disease with a similar name, namely conjunctivitis - inflammation of the eye as a result of a foreign body or harmful microorganism. It can also be a side effect of some diseases that have nothing to do with the eyes, for example: acute respiratory viral infections, acute respiratory infections, influenza, measles, pneumonia. In the most severe and advanced cases, follicles—small “bags” with ectosomatic secretions—can be damaged. Because of this, they can increase in size, injuring the cornea. What types of conjunctivitis exist and how do they differ from each other in terms of symptoms, causes and methods of treatment?
Conjunctivitis due to viral infections
Very often, eye inflammation occurs against the background of current infectious diseases: ARVI, influenza. Thus, acute respiratory diseases of the upper and lower respiratory tract caused by adenoviruses are often accompanied by various conjunctivitis. They progress especially quickly in children's groups: coughs and runny noses contribute to the rapid spread of the virus and cause an epidemic. When conjunctivitis develops against the background of a cold or infectious disease, medications are prescribed to eliminate the underlying disease, as well as drops and ointments intended to relieve eye inflammation.
What types of conjunctivitis are there?
The types of conjunctiva can be very diverse; conditionally, all of them can be divided into two large groups: endogenous and exogenous. Which form the doctor will determine will directly depend on the main cause that led to damage to the visual organs. For example, the endogenous type of inflammation usually manifests itself in conjunction with various other diseases. In fact, it is a secondary sign of a particular disease, for example:
- chicken pox;
- rubella;
- tuberculosis;
- hemorrhagic fever;
- Zika virus.
As for the exogenous subgroup of conjunctivitis, they usually occur independently, due to the entry of a provoking component into the body. Their further classification and method of treatment are selected based on what exactly caused the disease.
The causes of exogenous conjunctivitis are not as few as it might seem at first glance. These could also be:
- Leffler's wand.
- Neisser's gonococcus;
- diplobacillus Morax-Axenfeld;
- adenovirus;
- allergic components.
The causes of conjunctivitis can be completely different: from the banal contact of any allergen in the eyes, for example, household dust and particles of animal hair, to more serious ones, to which ophthalmologists include the Zika virus, which is widespread in South Africa and Southeast Asia.
Today, ophthalmologists distinguish the following types of inflammation of the connective membrane:
- allergic, also associated with disturbances in the functioning of the immune system of the human body;
- bacterial, which include pneumococcal, diphtheria, diplobacillary, gonococcal and others;
- fungal, the causative agents of which are various types of pathogenic fungi;
- viral, usually arising as a result of various viral infections and the entry of their smallest particles into the eyes;
- traumatic, the cause of which may be thermal or chemical burns.
Remember that only a qualified specialist can determine the true cause of the pathology, based on the results of the examination. That is why we strongly do not recommend that you neglect consulting an ophthalmologist: if you notice the first symptoms, immediately make an appointment for the next appointment.
What rules should be followed during the treatment process?
contact lenses, as eye discharge will accumulate on their surface, increasing inflammation. It is also better to exclude decorative cosmetics and face creams from everyday use at this time, as they can cause an allergic reaction and increase irritation. Almost any infection is a consequence of a weak immune system, and it needs to be strengthened. It would be a good idea to take a vitamin complex for the eyes, and also include in your diet foods that contain elements that are beneficial for the organs of vision: selenium, zinc, magnesium, etc. You should avoid spending long periods of time at the computer to prevent dryness and overstrain of the visual organs. A large percentage of success in treatment depends on following these simple rules.
Causes of allergic conjunctivitis
So, we figured out what types of inflammation of the connective membrane of the eye are. But why does the doctor diagnose one patient with an allergic form, and another, for example, with a fungal one? Let’s try to understand exactly what reasons are characteristic of this or that type of pathology. Let's start with the allergic type, since, firstly, it is considered the most common, and, secondly, it is the easiest to cure. Allergic conjunctivitis occurs due to the body's increased sensitivity to a particular allergen, which may include:
- house dust;
- plant pollen;
- animal hair;
- paints and varnishes;
- Perfumes and cosmetics.
Diagnosing allergic conjunctivitis is quite simple, and it will not take much time from a professional. Many symptoms characteristic of this pathology “lie on the surface”: this is hyperemia - overflow of blood in the vessels of the cornea, swelling of the mucous membrane, itching, and many other sensations that cause discomfort to the patient.
Conjunctivitis due to adenovirus infection
Almost any infection caused by an adenovirus causes inflammation of the eyes, and these symptoms appear on the first or second day. What happens when this happens? Here are some manifestations that may indicate the presence of adenoviruses in the body:
- swelling and hyperemia (redness) of the conjunctiva;
- severe itching and burning in the eyes;
- foreign body sensation;
- profuse lacrimation and nasal discharge;
- painful reaction to bright light;
- enlarged lymph nodes near the ears;
- a thin grayish film on the cornea (with membranous conjunctivitis);
- follicles and ulcers on the edge of the eyelid (follicular form).
If such signs appear, you should not delay your visit to the ophthalmologist, since viral conjunctivitis can also be accompanied by a bacterial infection. Its course is accompanied by purulent discharge from the eyes and other unpleasant symptoms that will be difficult to cure if the disease is advanced.
Diagnosis and treatment of allergic conjunctivitis
Direct diagnosis carried out by a specialist is based, first of all, on collecting an allergy history. The doctor may ask whether you are “allergic”, to what extent this condition is typical for you, etc. Next, the ophthalmologist will refer you to an allergist, who will have to conduct special tests or take blood from a vein. This is necessary in order to accurately determine the nature of inflammation of the connective membrane.
If the ophthalmologist’s suspicions of allergic conjunctivitis are proven, treatment, first of all, should include complete isolation of the allergen. If it is a food product, then you urgently need to exclude it from the diet; if it is pet hair, then most likely you will have to part with your pet, at least for the duration of therapy. Antihistamines are prescribed as conservative treatment methods, used by doctors for many years, including:
- "Claritin";
- "Cetrin";
- "Erius";
- "Ketotifen";
- "Lomilan."
In parallel with them, when diagnosed with conjunctivitis, treatment must necessarily include the use of eye drops. Their role in the treatment of pathology is very important, since they have a direct effect on the affected area and, in combination with taking antiallergic medications, are very effective. These are drugs such as:
- "Cromegexal";
- "Allergodil";
- "Azelastine";
- "Levocabastine";
- "Olopatadine."
Often, ophthalmologists prescribe cromoglycic acid derivatives, which are stabilizers of mast cell membranes, to their patients. Their operating principle is quite simple. When they come into contact with an allergen, they release chemicals into the blood, the main one of which is histamine. Mast cell membrane stabilizers block the association of allergic components, thereby reducing allergy symptoms. They are produced in the form of drops, for example:
- "Intal";
- "Cromogen";
- "Opotanol";
- "Lomuzol";
- "Allergo-Chest of drawers".
If allergic conjunctivitis is accompanied by “dry eye syndrome,” then the specialist may recommend the use of drugs that increase the level of hydration of the cornea. One of the most famous among them is Visin Pure Tear. Today you can buy drops not only in an optician or a specialized online store, but also in a regular pharmacy.
General principles of treatment
The treatment regimen for conjunctivitis can vary widely depending on the cause of the disease. Treatment of conjunctivitis has three main goals: • increase patient comfort; • completely stop or at least alleviate the course of the infectious process; • prevent the spread of infection in contagious forms of conjunctivitis.
Appropriate treatment for conjunctivitis is prescribed depending on its cause. Currently, there is no etiotropic (i.e., aimed at eliminating the cause of the disease) treatment for ordinary viral conjunctivitis; it usually goes away on its own within 1 to 6 weeks. Moisturizing eye drops (artificial tears) sometimes help relieve symptoms. Antibiotics have no effect on viral infections.
When treating allergic conjunctivitis, the first step should be to remove the irritant or avoid further contact with it, if possible. Cold compresses and artificial tear drops sometimes relieve discomfort in mild cases.
For more severe cases, nonsteroidal anti-inflammatory drugs and antihistamines may be prescribed. Cases of persistent allergic conjunctivitis may also require the use of topical steroid eye drops.
Bacterial conjunctivitis is usually treated with eye drops or ointments containing an antibiotic. Improvement may be observed after 3-4 days of treatment, but a full course of antibiotic therapy should be carried out to prevent relapse of the disease.
Allergic conjunctivitis is an inflammation of the conjunctiva caused by the body's reaction to an allergen. The conjunctiva contains a large number of immune cells (mast cells) that release chemicals (transmitters) in response to various antigens (such as pollen or dust mites). These mediators cause an inflammatory response in the eye, which can be short-lived or long-lasting. About 20% of people have some degree of allergic conjunctivitis.
Seasonal and year-round allergic conjunctivitis
are the most common types of allergic reactions in the eye. The first is often caused by tree or grass pollen, and as a result usually appears in the spring and early summer. Weed pollen causes the development of symptoms of allergic conjunctivitis in the summer and early autumn. Perennial allergic conjunctivitis lasts throughout the year and is most often caused by dust mites, animal dander, and bird feathers.
Spring conjunctivitis
is a more severe form of allergic conjunctivitis, in which the causative agent (allergen) is unknown. This disease is most common among boys, especially between the ages of 5 and 20 years, who have concomitant diagnoses such as eczema, bronchial asthma, or suffer from seasonal allergies. Spring conjunctivitis usually worsens every spring, and in the fall and winter it is in a state of regression. Many children outgrow this condition by the time they reach puberty.
Giant papillary conjunctivitis
is a type of allergic conjunctivitis that occurs as a result of the constant presence of a foreign body in the eye. It occurs mainly in those who wear hard or soft contact lenses for a long time without removing them, as well as in those who have sutures protruding to the surface of the conjunctiva after surgical interventions.
Symptoms of bacterial conjunctivitis
The bacterial form of conjunctivitis in most cases occurs due to infection through contact and household contact. It is quite simple for a doctor to identify such a disease, since various types of bacteria that are not part of the natural microflora begin to multiply very actively on the mucous membrane. It is they who provoke a pronounced inflammatory reaction. Most often, the causative agents of this pathology are:
- staphylococci;
- pneumococci;
- streptococci;
- gonococci;
- Klebsiella
Among other things, the cause of inflammation can be Pseudomonas aeruginosa or Escherichia coli, tuberculosis microbacteria, Proteus - a pathogenic “inhabitant” of the intestines that can exist for a certain time in both soil and water. The greatest difficulties in treatment are the so-called “mixed infections”, when, for example, not only an allergen appears on the connective tissue, but also a certain bacterium, possibly one of the ones listed above.
Quite often, the bacterial species takes on an acute form even before the patient has time to see a specialist. This is facilitated by general weakness of the immune system, traumatic eye injuries, as well as relatively recent viral diseases, for example, some forms of hepatitis, measles, polio, parainfluenza and others. An important role in the development of pathology is played by stress, as well as long-term use of glucocorticoids, for example, Prednisone or Dexamethosone.
It is very important to know that the bacterial form of conjunctivitis is transmitted through household contact, which means that during treatment you should not wipe yourself with someone else’s towel, use handkerchiefs from relatives or friends, or drink or eat from the same container with them. If we are talking about a child who, while still a newborn, was diagnosed with “bacterial conjunctivitis,” then it is likely that this pathology was transmitted to him from his mother. This happens when during pregnancy a woman suffers from inflammatory diseases of the genital organs and does not use the necessary medications.
Treatment of conjunctivitis with antiviral drops
To instill medicines, you need to use individual pipettes if the bottle does not have a spout, and to put in the ointment, you need to use special spatulas. The doctor prescribes the medicine after determining the type of conjunctivitis.
Allergic, bacterial and viral types of this disease require different remedies. Here is a brief overview of the most popular drugs that are used in modern ophthalmology to treat conjunctivitis in adults and children. Many of them contain interferons. This is the name of protein molecules that provide antiviral immunity - they begin to be actively produced in our body during the invasion of viruses, bacteria, and the proliferation of tumor cells. Interferon can be called a universal defender, which begins to act first, even before the rest of the immune system comes into play. Interferon drugs are used to treat many diseases. Eye drops containing these proteins are good at eliminating inflammation, fighting viruses, relieving symptoms of the disease and improving general condition.
- "Poludan" - drops that induce the synthesis of interferon, which significantly speeds up the healing process. The active ingredients are polyadenylic and polyuridylic acids.
- "Ophthalmoferon" is prescribed for the treatment of various types of conjunctivitis, including adenoviral and herpetic. The drops are well tolerated by the eye tissues and do not cause side effects. There were no complaints of toxic or allergic reactions when using this drug.
- "Aktipol" are antiviral drops that activate interferon in the body, thus helping it build its own immune defense. Their use allows you to quickly eliminate swelling of the conjunctiva and regenerate the damaged cornea.
- "Albucid" is the most famous and inexpensive remedy for the treatment of inflammatory eye pathologies. Its active ingredient - sulfacetamide 200 mg - suppresses many pathogenic microorganisms, preventing their reproduction. The medicine is very effective in the initial stages of the disease, as it is quickly absorbed into the systemic circulation through the conjunctiva.
How to cure bacterial conjunctivitis?
If you have been diagnosed with bacterial conjunctivitis, local treatment is usually prescribed. The type of pathogen must be identified - the bacterium that led to the development of inflammation. An important role in its therapy is played by strict adherence to the rules of hygiene, ideally - washing the conjunctival sac with a needle-free syringe with antiseptic solutions, suitable: "Furacilin";
- "Boric acid";
- "Miramistin";
- "Albucid";
- "Levomycetin".
After the mechanical cleansing of the eyelids and connective membrane is completed, it is necessary to instill eye drops. It is very important to follow the regime of their use and apply at least every two to three hours. These are medications such as:
- "Ofloxacin";
- "Neomtsin";
- "Lincomycin";
- "Tetracycline";
- "Ciprofloxacin."
Before going to bed, in order to relieve the symptoms of bacterial conjunctivitis as quickly as possible, ophthalmologists recommend lubricating the eyelids with a special antibacterial ointment. However, in no case should you put a blindfold on your eyes, so if you are afraid of staining your bed linen, try to sleep on your back so as not to touch the pillow with your eyes. Basically, doctors prescribe the following types of drops:
- "Zovirax";
- "Virolex";
- "Oxlolin";
- "Tebrofen";
- "Bonafton."
If the symptoms of bacterial conjunctivitis are too severe and the prescribed treatment does not help, then the ophthalmologist may also add antihistamine or anti-inflammatory drops to the prescription list. In general, therapy for this pathology usually lasts no more than two weeks.
How is viral conjunctivitis transmitted?
The main method of transmission of viral conjunctivitis is through the air, which explains the rapid spread of the disease in groups and places where large numbers of people gather. What other ways and means of transmission of the virus are there? There is also contact transmission of the virus - through household items, equipment, and common devices. If cases of a viral infection are confirmed in the premises where the patient was, surfaces should be sanitized, floors washed, and the room ventilated to prevent the emergence of new cases of the disease. How long does the virus stay active and spread to other people? The incubation period for viral conjunctivitis ranges from three days to two weeks. Viral conjunctivitis is especially dangerous in the first days of illness. Thus, during adenoviral infection, viruses are released into the environment in huge quantities along with secretions from the nasal mucosa and conjunctiva. Such viruses are extremely stable and survive at room temperature on a variety of surfaces. They can last up to 10 days on the patient’s bed linen, scarves, and napkins; on dishes, toys, and personal belongings – up to 20 days. The causative agent of the disease can be in water, food, on the hands of the patient with conjunctivitis and on the hands of medical personnel, so everyone who comes into contact with the sick person should carefully observe hand hygiene and regularly disinfect the room.
Main characteristics of the fungal species
The next form of pathology is called fungal, or ophthalmicosis, in medical terms. This pathology is characterized by inflammation of the connective membrane in a chronic form, which is provoked by pathogenic fungi. The danger, and therefore the difficulty in treating the disease, arises due to the fact that pathogenic fungi have a very high viability. For example, in nail plates, hair, and conjunctiva, they can live for about one year. Depending on which particular fungus became the cause and main causative agent of conjunctivitis, the inflammatory process itself may be accompanied by:
- purulent inflammations accumulating in the corners of the eyes;
- catarrhal inflammation of the mucous membrane, accompanied by increased lacrimation;
- the formation of mucin films mixed with protein or lipid deposits;
- the formation of nodular infiltrates mixed with blood and lymph.
In connection with the above symptoms, this type of pathology can easily be confused with another ophthalmological disease - keratoconjunctivitis, which manifests itself not only in inflammation of the connective membrane, but also of the cornea. In any case, an ophthalmologist, after conducting the necessary examination, will be able to establish the correct diagnosis and prescribe qualified treatment.
Classification of conjunctivitis
All conjunctivitis is divided into infectious and non-infectious. Infectious conjunctivitis can be:
- bacterial (acute and chronic staphylococcal conjunctivitis, acute pseudomonas and gonorrheal conjunctivitis);
- viral (epidemic keratoconjunctivitis, adenoviral, herpetic, hemorrhagic);
- chlamydial (trachomas, paratrachomas, chlamydial conjunctivitis of adults and newborns);
- fungal;
- acanthomoeba (keratoconjunctivitis).
Diagnosis and therapy of fungal conjunctivitis
The main way to diagnose conjunctivitis, which has a fungal form, is to take a smear from the connective membrane or a scraping. All these procedures should be carried out only in a specialized institution and only under completely sterile conditions. If the results of the examination confirm that the patient suffers from a fungal type of inflammation, then the treatment is prescribed for quite a long time. In most cases, experts recommend the following medications:
- "Fluconazole";
- "Nystatin";
- "Miconazole";
- "Amphotericin";
- "Ketoconazole".
These products belong to the category of fungicidal. There is another group of drugs that are very effective in treating fungal inflammation of the connective membrane. They are called fungistatic and are available both in the form of tablets and in the form of ointments, sprays or aerosols. These include:
- "Lamisil";
- "Mikoket";
- "Zinocap";
- "Thermikon";
- "Loceril."
The question that arises immediately is what is the difference between fungicidal and fungistatic drugs? Why can't they replace each other? The fact is that fungal conjunctivitis, the treatment of which is a rather complex and lengthy process, requires quite a long and massive therapy. Antihistamines or drops alone will not be enough here.
Fungicidal agents are intended to directly destroy the fungal pathogen, and fungistatic agents are intended to suppress further proliferation of fungi. Taken together, these drugs have a fairly strong and, most importantly, stable effect. In general, the treatment process can take about a month and a half, but even after complete recovery, the doctor may recommend an additional visit to remove smears from the conjunctiva.
What provokes the development of viral conjunctivitis: ways of transmitting the disease
Viral conjunctivitis - what causes the disease and how to protect yourself from infection? Conjunctivitis can be caused by both bacteria and viruses. For its correct, successful treatment, it is necessary to know the type of pathogen. Among the bacterial pathogens: streptococcus, staphylococcus, Pseudomonas aeruginosa, pneumococcus.
The viral nature of the disease is often confirmed by laboratory testing of a smear from the conjunctiva and the identification of:
- Adenovirus - this type of conjunctivitis is transmitted without contact; adenovirus infections are common in preschool and school groups and have different forms of manifestation: conjunctivitis, pneumonia, fever, nasopharyngitis, etc.
- Herpes - with this viral conjunctivitis in adults and children, most often one eye is affected, the onset of symptoms is gradual, accompanied by a rash on the skin of the eyelids. The amount of mucous discharge, unless a bacterial infection is involved, is small.
- Enterovirus - acute viral conjunctivitis occurs with pronounced symptoms and is transmitted by contact through common household items and medical instruments. The virus, after accumulating on the mucous membrane, can penetrate the blood and spread throughout the body.
How is purulent conjunctivitis transmitted? Diseases caused by bacteria and viruses spread quickly in children's groups due to close contact between children. In groups, children share toys, which provokes contact transmission of the virus, but conjunctivitis is transmitted not only by contact, but also through the air. Viral conjunctivitis in hot, dry climates leads to an epidemic, so in such regions it is advisable to use preventive measures: in April-May, before the start of the dry, windy season, people at risk are instilled with antimicrobial drops. Conjunctivitis, like other eye infections, is extremely dangerous, so preventive measures cannot be ignored.
The eye virus is transmitted without contact, and in order to reduce the risk of infection, it is necessary to constantly moisturize the conjunctiva with artificial tear preparations, which create a uniform protective layer on the surface of the eyes - the tear film. Knowing how dangerous conjunctivitis is, how the disease is transmitted, what the first symptoms are, you can take all the necessary measures to protect team members, relatives of the patient, etc. from the disease.
What is a viral type of conjunctivitis?
As the name of this type of inflammation makes clear, its main cause is viruses. Depending on which one of them caused the specified pathology, the ophthalmologist will be able to draw a conclusion about whether it is single or represents a complex set of viral infections. It is quite easy to determine this even without being a qualified specialist. So, for example, if you initially suffered from: influenza, measles, chicken pox, rubella or mumps, in other words, most of those diseases that are considered to be childhood diseases, then, most likely, conjunctivitis developed precisely against the background of these diseases and, accordingly, your the case falls into the second category. If the cause of inflammation is an adenovirus, enterovirus, herpes zoster or herpes simplex, then your case is in the first category. In most cases, the most characteristic symptoms of viral damage to the connective membrane begin to appear simultaneously with infection of the upper respiratory tract. This form of the disease affects two eyes at once. Even in situations where the infection initially concentrates on one of them, it quickly spreads to the other. Sometimes this happens within just a couple of days. The danger of viral conjunctivitis is that it is transmitted through household contact. You can become infected with it through any close contact, for example:
- shaking hands;
- use of shared household appliances;
- by airborne droplets.
The incubation period of viral inflammation of the connective membrane ranges from 5 to 14 days. As ophthalmologists say, already at the appointment, many patients remember that they had some kind of contact with one of their friends or acquaintances suffering from viral conjunctivitis. After the incubation period, the following symptoms begin to appear:
- in one of the eyes, the formation of serous fluid begins, released from the tissues of the blood vessels, and is quickly transmitted to the second eye;
- the lymph nodes in the ear area may become enlarged and painful when touched;
- irritation of the nerve endings occurs and the eye vessels enlarge, which is usually accompanied by increased lacrimation and redness;
- transparent follicles with redness along the edges begin to appear on the connective membrane;
- there is a feeling of the presence of a foreign body in the eyes, as well as itching and photophobia.
Doctors consider clouding of the cornea of the eye to be the most dangerous manifestation of this disease, which in most cases leads to a decrease in visual function.
The first symptoms and methods of transmission of viral conjunctivitis
How does ocular conjunctivitis begin, what are the signs of the disease? Profuse lacrimation, photophobia, redness of the eyes, scanty mucous, clear discharge - these are typical signs of both viral and bacterial conjunctivitis. Other symptoms are related to the type of pathogen. So, with adenoviral conjunctivitis, in addition to swelling of the mucous membrane, patients may have an elevated temperature, cough, runny nose, and fever. How is conjunctivitis caused by an adenovirus transmitted? Adenoviral conjunctivitis is transmitted by airborne droplets and contact, manifests itself in catarrhal, follicular or membranous form:
- in the catarrhal form, the disease passes quickly, with minor inflammation and lasts about 5-7 days;
- the filmy form of the disease is characterized by the formation of dense gray films and pinpoint infiltrates;
- If conjunctivitis has a follicular form, then painful small blisters are noticeable on the mucous membrane of the eye.
Among the distinctive symptoms of herpetic viral conjunctivitis in adults are mild redness of the eyes and a small amount of discharge. Ulcers and erosions may form on the edges of the eyelids. Is conjunctivitis transmitted by airborne droplets? Yes, viral diseases are contagious even at a distance and are dangerous due to their severe course and numerous complications. Thus, with epidemic conjunctivitis in adults, severe swelling of the mucous membrane is observed and the temperature rises. In this form of viral conjunctivitis, the infection can spread rapidly, leading to an epidemic of the disease. What are the methods of contact and non-contact transmission of the virus?
Therapy for viral conjunctivitis
Treatment of viral conjunctivitis is carried out on an outpatient basis, that is, the patient is placed in a specialized department of the nearest hospital. It is recommended to use antiviral agents as therapy. Traditionally, the treatment plan looks like this:
- the patient is prescribed droppers with interferon or another antiviral agent;
- deoxyribonuclease is instilled into the eyes at least 6 times during the first week of treatment and at least 2 times a day during the second;
- the use of ointments has been successfully practiced, for example: adimalova, florenal, tebrofenov, bonaftone, riodoxol;
- antihistamines are prescribed, both in the form of drops and tablets.
If the main cause of the development of inflammation of the connective membrane was one of the viral diseases that we mentioned above, then therapy, first of all, should be aimed at combating this disease. As a rule, when the underlying disease is treated, the symptoms of viral conjunctivitis also disappear.
Useful video
Dr. Komarovsky about conjunctivitis in a child: causes of the disease, treatment methods and signals for urgent consultation with a specialist.
Author's rating
Author of the article
Alexandrova O.M.
Articles written
2029
about the author
Was the article helpful?
Rate the material on a five-point scale!
If you have any questions or want to share your opinion or experience, write a comment below.
Traumatic form of conjunctivitis
None of us, unfortunately, are immune from various foreign bodies getting into our eyes. The simplest thing is dust particles, because given the current state of the environment, perhaps few people manage to avoid this. However, our visual organs can be damaged not only from dust, but also from animal hair, various straws, and crumbs. The very first and obvious symptom of inflammation of the connective membrane is its redness. It may often be accompanied by an itching or burning sensation. Many people in such situations use folk remedies for treating conjunctivitis, but we strongly recommend that you visit an ophthalmologist. Treatment consists of thoroughly washing the visual organs with a special solution. Doctors also prescribe antiseptic eye drops, for example:
- "Maxitrol";
- "Vitabact";
- "Ofloxacin";
- "Tsiprolet";
- "Tobropt."
The organs of vision can be damaged not only by dust particles or animal fur. The eye can be injured by a nail, a spark from welding, etc. In such cases, you must immediately consult a doctor, and it is best to call an ambulance team, which will promptly take you to the nearest specialized department of one of the hospitals.
Prevention of conjunctivitis
Any person knows that it is much easier to prevent a disease than to cure it in the future. This directly applies to conjunctivitis, or inflammation of the connective membrane of the eye. What needs to be done in order to avoid this disease and continue to enjoy bright and contrasting vision under any conditions? According to ophthalmologists, the main way to prevent this pathology is to strictly adhere to the rules of hygiene. This means that a face towel, like decorative cosmetics, including various lotions and cleansers, must be strictly individual.
You should wash your hands not only before eating, but every time you come from the street and other public places. If you do not have such an opportunity, for example, you have a traveling nature of work, then we recommend carrying a bottle of water with you so that you can wash your hands at any time, or special antibacterial liquids or wipes. Otherwise, if both options are not possible, try not to touch your face with your hands, and especially your eyes. If, while on the street, you feel that a speck has gotten into your eye, then try to pull it out with the help of disposable handkerchiefs.
Prevention
Timely adequate therapy allows you to get rid of conjunctivitis in 1-2 weeks. But even with proper treatment, relapses are often observed. With each subsequent inflammation of the ocular mucosa, the pathological process becomes more severe and the quality of vision decreases. Therefore, it is important to prevent the disease. To do this, you should follow the following recommendations:
- observe the rules of personal hygiene;
- avoid contact with sick people;
- strengthen the immune system;
- observe safety measures at work;
- touch your eyes less;
- wear contact lenses correctly;
- use high-quality cosmetics;
- treat concomitant diseases.
When the first signs of inflammation of the organs of vision appear, you should immediately contact an ophthalmologist. You should not let the disease take its course or try to cure it on your own.
Author of the article: Kvasha Anastasia Pavlovna, specialist for the website glazalik.ru Share your experience and opinion in the comments.