Signs of aphakia and diagnosis
Aphakia deprives the eye of all functions associated with the lens. There is no accommodation, refraction is impaired. Points of clear vision near and far merge. The iris constantly trembles due to the inability of the eye to focus and the lack of support, the role of which is normally performed by the lens. A characteristic sign determined visually is an excessively deep anterior chamber.
Monocular (one-sided) aphakia causes disturbances in binocular perception. To preserve and restore it, correction, treatment and exercises should be prescribed as soon as possible after lens loss.
Symptoms
When examining an aphakic eye, you can see iridodonesis (tremor of the iris) and a fairly deep anterior chamber. In cases where the posterior capsule of the lens remains preserved, iris trembling is less noticeable, because it reduces the shocks of the vitreous body that occur when moving the eyes.
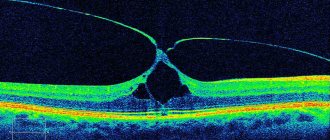
In the complete absence of the lens bag, the vitreous body is retained solely by the anterior limiting membrane, as a result of which it begins to protrude in the pupillary region. This pathological condition is called a vitreous hernia. If the membrane ruptures, the vitreous fibers exit into the anterior chamber of the eye. In this case, they speak of a complicated vitreous hernia.
Vision correction for aphakia
Unilateral aphakia is always accompanied by aniseikonia (difference in retinal images in both eyes). This makes it difficult to select glasses for correction. If the second eye retains high visual acuity, it is advisable to immediately resort to surgical implantation of an intraocular lens before the ability of binocular perception decreases.
In other cases, spectacle correction may be quite sufficient. First, distance lenses are prescribed. After getting used to them, glasses are selected for close vision. Two pairs of glasses for aphakia are a necessity that cannot be avoided. Sometimes the absence of only one lens can be successfully corrected with contact lenses. Glasses and lenses can simultaneously eliminate astigmatism, which often accompanies aphakia.
Of course, the complete absence of a lens does not allow for a 100% correction. At the periphery of the visual field, a ring scotoma (prolapse zone) remains, in which, under certain conditions, unclear outlines of objects and distorted figures can flicker. Such phenomena complicate life where visual strain and attention are required (for example, when crossing streets with heavy traffic, working on an assembly line). If correction is accompanied by significant discomfort, you should consider surgical treatment.
Afakia
Aphakia is corrected using glasses, contact and intraocular lenses. The indication for spectacle vision correction is a bilateral form of the disease. For unilateral aphakia, glasses are recommended only if contact methods of correction are intolerant. The choice of glass for an emmetropic eye is difficult, because even glass of +10 diopters is not comparable to the refractive power of the lens, which is 19 diopters. This is due to the fact that the refractive index of the liquid that surrounds the lens is higher than that of the air surrounding the glass.
The optical power of a glass lens depends on the patient's refraction. For hyperopia, it is necessary to choose glasses with stronger optics than for myopia. There is no need to prescribe vision correction methods to patients with high degrees of myopia before lens removal. Due to the lack of accommodation ability, the patient should be prescribed glasses for near vision that are 3.0 diopters stronger than for distance vision.
Contact or intraocular vision correction is indicated for patients with monocular aphakia. Prescribing glasses to patients with this form of the disease will worsen aniseikonia. During surgery (intraocular correction), an artificial lens with individually selected optical power is implanted. The most preferred treatment option is the use of posterior chamber lenses, since localized at the location of the natural lens, they provide high quality vision. Congenital aphakia can be corrected using this technique only after the child reaches two years of age.
Forecast and prevention of aphakia
The prognosis for life and ability to work with proper correction of aphakia is favorable. In the absence of timely treatment, there is a high risk of complete loss of vision, which subsequently leads to disability.
In ophthalmological practice, there are no specific measures to prevent congenital aphakia. To prevent the development of acquired forms of the disease, it is necessary to undergo an annual examination by an ophthalmologist. This will help to timely diagnose those diseases that can lead to surgical removal of the lens. Persons at risk of eye injury due to the nature of their profession must use protective glasses or masks during working hours.
Treatment of aphakia in children
Young patients need to undergo especially careful vision correction in order to bring it to the highest possible acuity values. As the child grows, the size of the eyes also increases, which necessitates regular visits to the doctor and new prescriptions for optical products.
The main method of correction in children is contact lenses. Most experts recommend soft samples for wearing at a young age, with excellent moisturizing properties and excellent gas permeability, allowing the eye to breathe. To treat aphakia in infants, only silicone contact lenses are used.
| The main negative point is the high cost of correction products, children grow quickly, and periodically there is a need to replace them, and thanks to an active lifestyle, a child may simply lose lenses. |
It is possible to use glasses. Their cost is lower, but it is quite problematic for small children to hold a frame with very heavy lenses on a small nose.
It is considered inappropriate to implant an IOL in the first years of life, because during this time the body grows, as they say, by leaps and bounds, which makes it much more difficult to calculate the required strength of an artificial lens. Ophthalmological specialists believe that surgical intervention should be resorted to when the little patient reaches two years of age.
Types of cataracts
There are two forms of the disease: congenital and acquired. The first ranks first among the causes of childhood blindness, the second is a consequence of age-related changes, previous injuries or illnesses, and can also be caused by adverse environmental influences.
If a congenital pathology is not recognized in time, the child is likely to face serious vision problems, including complete blindness. It is this fact that explains the inclusion of a pediatric ophthalmologist in the list of specialists whose visits are included in the mandatory medical examination program for one-month-old infants. Under no circumstances should you neglect a professional examination for fear of catching an infection at the clinic or for any other reason. Remember that such carelessness can cost the child too much. Also, do not refuse surgical intervention if the ophthalmologist insists on it. Timely treatment will save you from many problems in the future.
Important! If you start congenital ocular cataracts, the process will very quickly become irreversible due to the fact that the baby’s vision has just begun to form, and the affected eye ceases to perceive the image. Delay on the part of parents can lead to the fact that even surgery will not help restore the necessary functions. Experts insist that it is necessary to operate on a diseased organ at a very early age - before the age of two months.
As the name suggests, acquired cataracts do not occur in humans at birth, but appear over time under the influence of certain factors and are constantly progressing.
Why do cataracts occur?
The causes of eye cataracts have been described quite a bit, but, in general, they can be divided into internal (aging of the body, various diseases and general health) and external (trauma, burns, toxicological effects).
Ultraviolet radiation occupies a special place among the external causes of cataracts. Every reasonable person knows and understands perfectly well that it is forbidden, for example, to poke someone in the eye with a fork or spray mosquito repellent in the face, so such injuries are absolutely obvious and, as a rule, are accidental. The same cannot be said about the sun's rays: if only the lazy did not talk about the increased risk of skin cancer, then people tend to underestimate their destructive effect on the lens of the eye.
Surkova told the Federal News Agency about the phenomenon of so-called “snow blindness,” when ultraviolet light, reflected from the surface of a snowdrift somewhere on the top of a mountain or from gentle-looking sea waves, can cause a real burn of the conjunctiva. However, you should not think that such troubles are entirely the lot of vacationers. Insidious UV radiation can harm the eyes even under normal conditions.
One of the most important missions of the lens is to protect the retina from harmful radiation by absorbing it. Of course, once you look at the sun, you can hardly go blind, as grandmothers loved to scare in childhood. However, the damage caused tends to accumulate, which is why it is so important to take timely precautions and protect your eyes from direct sunlight.
Ekaterina Surkova recommends that everyone, regardless of age, wear good sunglasses and hats with wide brims or visors every time they go out into the open sun. At the same time, the ophthalmic surgeon emphasizes that not all glasses are equally useful. Be sure to pay attention to the mark on nanometers on the lenses - the number must be at least 400, then the material will reliably block ultraviolet radiation. If you cannot do without optics with diopters, then a special coating can be applied to your usual glasses. In addition, try to purchase glasses in trusted salons and specialized stores, and not in a subway crossing.
Among other external and internal causes of cataracts are: - aging; - blows, cuts, burns, punctures; - systemic use of hormones; - myopia; — diabetes mellitus (with this disease, vision is almost the first to suffer); - glaucoma and other ophthalmological pathologies.
If we talk about congenital cataracts, the main factors that provoke its appearance in children are: - the presence of damage in genes and chromosomes; - heredity; - taking certain types of antibiotics during pregnancy (this is why it is so important for women while expecting a child to consult an obstetrician-gynecologist before taking any medications); - infections dangerous to the fetus suffered by the expectant mother: rubella, measles, toxoplasmosis, etc. (it is advisable to undergo appropriate examinations at the stage of pregnancy planning to identify the presence or absence of antibodies, and, if necessary, undergo vaccination); — chronic illnesses of the mother; - alcohol, nicotine or drug addiction of the mother.
Diagnosis of aphakia
Detecting the disease at an early stage is the key to a likely successful outcome in the fight for your vision. As trivial as it sounds, an annual visit to the ophthalmologist’s office significantly reduces the risk of receiving an unpleasant diagnosis.
The doctor determines the disease based on his own examination, medical history, and based on the nature of the clinical picture. It should be understood that some of the symptoms inherent in aphakia may correspond to traumatic lens luxation. In these cases, a repeated, more thorough examination usually reveals its displacement.
To accurately diagnose aphakia, a number of studies are necessary:
- visometry – identifying the real level of visual acuity degradation;
- gonioscopy – to measure the angle of the anterior chamber and its depth;
- biomicroscopy - a detailed study of the internal structures of the visual organ;
- ophthalmoscopy – identification of possible concomitant pathologies, and development of a treatment plan, taking into account all detected factors;
- refractometry - determining the ability of the organ of vision to refract light;
- Ultrasound of the eyeball.
Having collected the test results and research data, the ophthalmologist determines the methodology, develops a plan to combat the disease, and begins to implement it.
Diagnostics
Since the absence of the lens is noticeable upon initial examination with the naked eye, diagnosing aphakia is not difficult. But in order to fully assess the condition of the patient’s visual organ, the ophthalmologist usually conducts the following studies:
- Ophthalmoscopy - checking the condition of the fundus, optic nerve head and retina, assessing the condition of the eye vessels using special lenses.
When diagnosing, an ophthalmologist uses special equipment
- Refractometry is the determination of the refractive index of light in the patient’s organ of vision. For this study there is a special device - a reflectometer.
- Biomicroscopy - checking the structure of all parts of the eye, which is carried out using a special slit lamp,
- Since aphakia can exist simultaneously with retinal detachment, the ophthalmologist may additionally prescribe an ultrasound of the eye, which will help identify this pathology.
- If correction of aphakia is intended through surgery, the patient should undergo all tests, as before any operation, in order to identify hidden foci of inflammation or other problems with general health.
Symptoms of cataracts
If the disease is localized not in the central, but in the peripheral zone of the lens, then it may not manifest itself sufficiently for a long time for the patient to decide to seek help from a specialist, which complicates subsequent treatment.
Ophthalmologists advise showing concern and coming to an appointment as soon as possible if a person notices the following alarming symptoms:
- blurred vision, blurred vision, blurred contours; - change in pupil color to white, yellow or gray; - double vision; — flies, dots, light flashes before the eyes; - deterioration in color perception; - painful reaction to bright light; - general deterioration in visual acuity, for example, when reading or manipulating small objects.
When the first signs of the disease appear, you must immediately consult an ophthalmologist, who will conduct a visual examination and a series of instrumental examinations that will help determine how far the process has progressed and determine treatment tactics.
Prevention
As you know, any disease is easier to prevent than to treat. To prevent cataracts, follow the advice of experts to maintain clear vision for many years:
1. Get examined by an ophthalmologist at least once a year and more often. 2. Eat right. Include in your diet foods and vitamin complexes (as recommended by your doctor) containing vitamins E and C, microelements and antioxidants that are beneficial for vision. 3. Give up bad habits 4. Spend time in the fresh air more often. 5. Protect your eyes from direct exposure to ultraviolet rays. 6. Monitor your blood sugar and cholesterol levels regularly. 7. Take good care of your hygiene. 8. Observe safety precautions and use personal protective equipment in places where eye injury may occur.
Definition of pathology
Aphakia is the absence of a lens in the visual system. In such patients, there is a disturbance in the refraction of light rays. This makes it impossible to examine objects located at different distances, which significantly reduces visual acuity.
The lens is one of the most important elements of the optical system of the eye. It is located in the posterior chamber and is shaped like a biconvex lens. Normally, it is completely transparent, this is ensured by special proteins - crystallins, which are part of it. Ligaments hold the lens in the correct position and, if necessary, change the curvature of the surface.
Main functions of the lens:
- passage of a ray of light from the cornea to the retina;
- refraction of rays so that a projection appears on the retina in the form of a thin beam;
- accommodation - a change in the shape of the lens from convex to stretched, which allows you to move your gaze from close to distant objects;
- barrier function - the lens does not allow the vitreous body to protrude forward, so it remains in its anatomical position;
- protective function - preventing the passage of bacteria and viruses into the vitreous body and retina.
Operating principle of the lens:
- The light beam is reflected from the object and passes through the pupil and cornea.
- Then it passes through the lens and transforms into a thin beam.
- The beam hits the retina, where it is perceived by nerve endings.
- Special receptors transmit information to the optic nerve.
- The signal is deciphered in the visual center, thanks to which a person sees surrounding objects.
Reference! The most important thing about the lens is its transparency and integrity. Otherwise, the light beam will not be able to project onto the retina in the form of a thin beam.
When the lens is absent in only one eyeball, they speak of unilateral aphakia, when in both, bilateral aphakia is diagnosed.
Aphakia in all cases requires therapy. Without timely correction, the risk of complete loss of vision and, accordingly, disability increases.
Stages of pathology:
- Monocular aphakia. Violations of mild or moderate severity are observed. In this case, visual acuity decreases in the range of 0.4–1.0 diopters, while vision correction is possible with the healthy eye.
- Unilateral or bilateral aphakia. Vision is significantly reduced, but correction is still possible. If the field of view narrows significantly, correction is no longer possible. The patient is assigned disability group 3.
- The pathology occurs in conjunction with other diseases of the visual system that affect both eyes. Vision becomes within 0.04–0.08 diopters. The patient is assigned disability group 2.
- Monocular and binocular form with severe changes in ophthalmic structures. The patient is assigned disability group 1.
ICD-10 code
In the International Classification of Aphakia, code H27.0 is assigned.
Causes of aphakia
Ophthalmologists distinguish two forms of aphakia: congenital and acquired type. Congenital anomalies are divided into two groups.
Primary aphakia.
It is caused by delays in the formation of eyeball structures during embryonic development. Normally, at a certain stage, the lens vesicle should separate from the outer ectoderm. If this does not happen, there will be no lens in the eyeball.
Secondary aphakia.
It is caused by spontaneous resorption of the lens during embryogenesis. The lens capsule is formed from the basement membrane. Spontaneous mutation during its formation leads to resorption of the lens.
Congenital defects are rare diseases.
In most cases, the deviation is acquired. The main causes of aphakia:
- contusions of the visual organs as a result of bruises with blunt objects;
- penetrating wounds causing loss of an anatomical element;
- surgical operations.
In some cases, the lens is removed surgically when it is subluxated, dislocated or clouded. The likelihood of the occurrence of pathology increases significantly after 40 years of age due to the hardening of the lens and other age-related changes.