Indications The essence of the procedure Price Our capabilities
Selective laser trabeculoplasty is currently the most highly effective and reliable method of laser treatment for glaucoma. The operation allows you to normalize intraocular pressure, including in patients for whom drug treatment (using antiglaucomatous drops) does not bring the expected effect or is contraindicated.
The procedure prevents the development of severe complications of glaucoma, avoids surgery and returns the patient with glaucoma to a full life.
The essence of laser trabeculoplasty for glaucoma
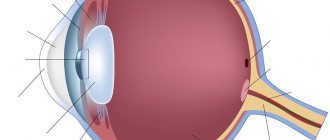
The purpose of laser trabeculoplasty is to eliminate the blockage of fluid outflow from the eye. Dosed cauterizations are performed with a laser beam on the elements of the ocular drainage system—the trabecular meshwork channels narrowed due to disease—with a laser beam. In this way, the lumens are expanded for normal outflow of intraocular fluid. The intervention is painless and bloodless and is performed on an outpatient basis in a few minutes.
Efficiency
In 8 out of 10 patients with early-stage open-angle glaucoma, the procedure eliminates the problem and allows you to stop using antihypertensive eye drops. In patients with advanced glaucoma, it helps reduce eye pressure and reduce the dosage of medications.
Possible complications
Even with such a low-traumatic procedure as selective laser trabeculoplasty, there is a risk of complications. These include:
- Allergic reactions, which are manifested by swelling, thinness and redness of the conjunctiva and eyelids. They occur in response to drops that are used during surgery. In this regard, it is necessary to warn your doctor if you have had similar reactions in the past.
- Inflammation that occurs in the postoperative period. In this case, keratitis, conjunctivitis, and corneal erosion develop. The risk of developing such negative phenomena is about 3-5%.
- A temporary increase in intraocular pressure that occurs in the postoperative period (usually on days 1-7).
- In approximately 12% of cases, selective laser trabeculoplasty fails to achieve a stable result. In this case, the doctor usually prescribes a full-fledged microsurgical intervention.
Types of laser trabeculoplasty
Operation argon laser trabeculoplasty ALT
ALT is a method of exposure to laser pulses with uniform parameters:
- wavelength – 488-512 nm;
- spot diameter – 50 µm;
- power – 400-1,200 mW;
- exposure time – 0.1 s;
- number of applications – 100 per eye or 50 per half of it.
Limitations and disadvantages of the method
The method is not effective for all patients with glaucoma, but only for those with severe pigmentation of Schlemm’s canal. A reactive rise in IOP is possible 1-4 hours after the procedure in approximately every third patient and after 1-2 weeks in approximately every fifth patient.
Over time, the achieved effect decreases - after 2 years the effectiveness of the method is 66%, after 4 years - 50%, after 10 years - 30%. When repeated, ALT is effective in only 3 out of 10 patients, and the risk of side effects is higher.
Surgery selective trabeculoplasty SLT for glaucoma
With SLT, a sharp, pointed beam of a 532 nm neodymium laser damages only the target cells and uses 5 times less energy. The frequency is 3 flashes per second, while the impact area is 8 times larger than with ALT.
Pointed extremely short pulses do not have a thermal effect on surrounding tissues, and therefore do not cause scarring. At the same time, they stimulate the body’s natural response - they activate the trabecular meshwork. Due to this, the intervention provides a sustainable effect, and if necessary, it can be repeated many times. There are practically no complications after the procedure and it has an ultra-short recovery period.
Methodology
In selective laser trabeculoplasty, the laser beam is directed directly at the pigment cells in the trabecular zone (the angle of the anterior chamber of the eye). In this case, there is no thermal effect or coagulating effect on surrounding cells, including underlying collagen fibers. The mechanism of laser damage to pigment is based on the activation of macrophages, which destroy trabecular tissue debris by phagocytosis.
The technique proposed by M. Latina, in its original form, is used as an independent treatment for glaucoma (primary open-angle type) in the initial and advanced stages of the disease against the background of moderate and severe pigmentation of the trabecular zone. At the same time, the appointment of selective laser trabeculoplasty can reduce the level of intraocular pressure by 6-8 mm Hg.
Rehabilitation period
After surgery, the doctor measures intraocular pressure and prescribes anti-inflammatory drops. Normally, the patient may experience increased sensitivity to light and complain of fog before the eyes for up to several days. You can return home immediately after the procedure. You can return to your usual daily activities the next day.
Within 1-2 weeks after surgery:
- drink no more than 1.5 liters of liquid per day;
- exclude alcohol, coffee and strong tea, salty and spicy foods;
- alternate visual stress (30 minutes) with rest (15 minutes);
- avoid hypothermia and intense physical activity;
- do not swim in pools and ponds, do not take baths (replace with showers).
To clarify current prices, contact SM-Clinic by phone in St. Petersburg.
Find out more information by phone or fill out the online form - the administrator will contact you to confirm your appointment.
SM-Clinic guarantees complete confidentiality of your request.
Laser treatment of glaucoma
Most often, the most common type of glaucoma is primary, but there are actually at least three other types:
- Congenital glaucoma, which can be determined both genetically and by infectious processes in the mother during pregnancy. This disease is quite rare and, as a rule, is diagnosed during the neonatal period or in early childhood.
- Juvenile glaucoma, which has an age range of approximately 3-35 years.
- Primary glaucoma of adults associated with age-related changes in visual structures.
- Secondary glaucoma is a consequence of diseases that somehow affect the circulation of intraocular fluid.
Depending on the stage at which the pathology was diagnosed, in each case you can turn to any of the three methods of treating glaucoma, and yet the majority of cases of successful therapy involve laser treatment of glaucoma.
When it comes to such important matters as intervention during a serious illness, there is no doubt that the patient has the right to the most competent specialists that can be found in the field of treatment of each specific disease.
Each ophthalmologist working at the Fedorov Eye Clinic in Moscow is a master of his craft, guided by currently accepted treatment protocols and has all the necessary equipment for the highest quality treatment.
This is precisely the reason why this clinic is so successful in removing glaucoma with a laser, prolonging the visual health of hundreds and thousands of patients.
Laser treatment of glaucoma can be either an independent treatment method or combined with microsurgical interventions on the eye.
The essence of the treatment is to restore the outflow of intraocular fluid through natural pathways, and this manipulation is performed without directly compromising the integrity of the eyeball.
The laser beam simply penetrates the optical structures, acting only in the required place with a given intensity.
There is a laser-coagulator - the principle of its operation is a local burn of tissue, which stimulates the formation of scars and tissue atrophy, as well as a laser-destructor, which works by applying a shock wave and subsequent rupture of tissue.
Both principles formed the basis of the most common laser eye surgeries in world practice, and both types of operations are performed at a high level by the Medical Center named after. S. Fedorov.
Advantages of laser glaucoma removal:
- restoration of normal circulation of intraocular fluid along the paths of the natural drainage system of the eye;
- no need to use an intravenous method of pain relief - when performing glaucoma laser surgery, local anesthesia is sufficient, which significantly reduces the load on the circulatory system and expands the indications for surgery even in the presence of concomitant pathology;
- no need for hospitalization of the patient for the operation and the ability to leave the clinic on the day of the intervention;
- the minimum period of time required to restore the patient to full working capacity;
- absence of complications common during surgical interventions involving violation of the integrity of the eyeball;
- reasonable cost of the operation.
Leading doctors
- Karpova Margarita Yurievna
Operating ophthalmologist
st. Marshala Zakharova, 20
- Borisova Maria Leonidovna
Operating ophthalmologist
Udarnikov Ave., 19
- Radjabova Ashura Radjabovna
Operating ophthalmologist
Udarnikov Ave., 19
- Shablovsky Dmitry Yurievich
Ophthalmologist
Danube Ave., 47, st. Marshala Zakharova, 20
- Ageev Vladimir Sergeevich
Operating ophthalmologist. Candidate of Medical Sciences
Danube Ave., 47
- Manzyuk Natalya Sergeevna
Ophthalmologist
st. Marshala Zakharova, 20
- Gadzhieva Zaira Ilyasovna
Ophthalmologist
st. Marshala Zakharova, 20
- Meshcheryakov Evgeniy Vladimirovich
Operating ophthalmologist
Vyborg highway, 17-1
- Pryalukhina Maria Alexandrovna
Ophthalmologist
Vyborg highway, 17-1
View all
- Yakimova Maria Alekseevna
Dunaysky Ave., 47 - Salomov Manuchehr Abdukodirovich
Udarnikov Ave., 19
- Toporkov Igor Anatolievich
Danube Ave., 47
Hide
Advantages
- Selective laser trabeculoplasty is performed on an outpatient basis; local drip anesthesia is used for pain relief. This avoids the additional stress on the cardiovascular system associated with the use of general anesthesia.
- Thanks to the use of the most modern equipment, selective laser trabeculoplasty is low-traumatic, painless, takes minimal time, and has a low risk of intra- and postoperative complications.
- If there are indications, the operation can be repeated.
- During the operation, the laser does not damage the surrounding tissue, acting exclusively on the selected area.
- The technique is a worthy alternative to medical and surgical treatments for glaucoma, as well as other laser treatment methods (such as argon laser trabeculoplasty).
Contraindications
The operation does not bring the desired result in the inflammatory nature of glaucoma. It is also ineffective for congenital eye pathologies and associated increased IOP in young patients.
Laser surgery for glaucoma cannot be performed for the following pathologies:
- closed-angle form of pathology;
- clouding or swelling of the cornea;
- inflammatory processes of the eyes;
- paralytic mydriasis;
- slit-like shallow anterior chamber.
There are also general contraindications to the operation:
- severe diseases of the heart, kidneys, liver;
- diabetes mellitus in the stage of decompensation;
- ARVI, febrile condition;
- high blood pressure;
- HIV, syphilis.
The patient's condition is assessed by a doctor; it is possible to postpone the surgical intervention to a later date or completely refuse the operation.
Trabeculectomy – surgical treatment of glaucoma at an advanced stage
Trabeculectomy
is an operation that is performed to reduce intraocular pressure in stage 3 and 4 glaucoma. It is one of the most common surgical methods to combat this pathology in adults. The intervention is used for open-angle and chronic angle-closure glaucoma. It is also used to treat pathologies of inflammatory and traumatic nature.
APPOINTMENT FOR TRABECULECTOMY
Foreign medical centers adhere to modern protocols for the treatment of glaucoma. Operations to combat this pathology are performed by ophthalmologists with 20 years of experience. Contact MediGlobus. We will help you choose the best glaucoma surgery specialist and arrange an appointment with him.
Contraindications for trabeculectomy surgery for glaucoma
- previous failed trabeculectomy; damaged conjunctiva; Stevens-Johnson syndrome;
- neovascular form of glaucoma; uveitic glaucoma; complete blindness.
How is trabeculectomy performed for glaucoma?
During surgery, the eye surgeon creates a tiny flap in the sclera
. He then makes a small hole in the eye to release the fluid. Fluid from the eye may leak through the flap into the bleb, where it is absorbed by the intraocular tissues. This helps reduce blood pressure and slow down the progression of the disease.
Trabeculectomy is performed under general or local anesthesia. It lasts from 45 minutes to 1 hour. After the intervention, a patch is applied to the eye, which is removed after 1-2 days.
After surgery, patients stop taking any glaucoma medications. They are prescribed a course of antibiotics and steroid drugs to prevent the risk of infection.
Prognosis of trabeculectomy in the treatment of glaucoma
Trabeculectomy is the “gold standard” in the fight against advanced disease. According to the World Glaucoma Association, after it is carried out, 80% of patients manage to maintain normal intraocular pressure for 5 years or longer.
Complications of trabeculectomy
Although trabeculectomy is considered a safe procedure, it does have some side effects. These include:
- infection of the wound surface; drooping eyelid; swelling around the eye and bleeding;
- scarring; excessive decrease in intraocular pressure; retinal disinsertion.
Cost of trabeculectomy surgery abroad
The cost of trabeculectomy in foreign hospitals is determined taking into account the severity of the pathology, as well as the qualifications of the ophthalmologist.
The initial price for this intervention on one eye is:
| A country | Price |
| Türkiye | from $2,100 |
| Germany | from €3,500 |
| South Korea | from $2,360 |
| Austria | from €3,100 |
Where is glaucoma surgically treated abroad?
Operations for this disease are successfully carried out in ophthalmological centers and departments of leading hospitals in Turkey, Korea or the Czech Republic. Medical tourists also travel to Israel and Germany for surgical treatment of glaucoma. The following clinics are in demand in these areas:
Spreebogen Ophthalmology Center
Read about the clinic →
Chaim Sheba Clinic
Read about the clinic →
Reviews about trabeculectomy
Where it was held:
Batygoz Clinic
What procedure:
Trabeculectomy
Patient age:
57 years old
Patient from:
Sevastopol
Nikolay:
“I would like to leave my feedback regarding glaucoma surgery. The intervention was carried out in the Turkish Batigöz hospital. To be honest, I was a little worried that it would get worse, but everything went well. In 40 minutes they were able to stop the progression of the disease. It's been 2 years now and my vision remains the same. Thank you!"
Where it was held:
Spreebogen Clinic
Which procedure:
Trabeculectomy
Patient age:
50 years old
Patient from:
Kharkov
Michael:
“I went to Germany for treatment of stage 4 glaucoma. I didn’t want to get treatment in my native country. I've already healed. So, I survived from stage 1 of glaucoma to the last. I chose the Spreebogen clinic. Here I had a trabeculectomy, which was able to slow down the disease. I hope the results last a long time.”
What do you need to know about the disease?
Glaucoma is a chronic disease in which the level of intraocular pressure increases and the optic nerve is affected. The disease provokes decreased vision up to blindness. One of the main visible signs is a change in the color of the pupil. It becomes greenish or azure, which is why people often call glaucoma “green water” or “green cataract.”
According to statistics, about 70 million people suffer from this disease, and a million of them are Russians. Experts predict that in a year the number of patients will increase to 80 million.
Causes
The main cause of glaucoma is the inability to maintain the correct balance between the amount of aqueous fluid produced and the amount of fluid drained inside the eye. This imbalance is usually associated with a form of glaucoma. Under normal conditions, fluid flows out of the eye socket through a special channel. If it becomes blocked, excessive accumulation of fluid occurs inside the organ of vision, and glaucoma develops.
Increased intraocular pressure may be due to the following reasons:
- Excessive formation of intraocular fluid.
- Impaired removal of fluid through the drainage system of the eye as a result of its changes.
Other reasons for blockage of the water channel are as follows:
- An imbalance between the outflow and inflow of aqueous humor in the eye cavity, which is accompanied by an increase in IOP.
- Myopia.
- Elderly age.
- Hereditary predisposition.
- Inflammatory diseases of the organs of vision.
- Taking medications to dilate the pupils.
- Bad habits.
- Diseases such as diabetes, hypotension, atherosclerosis, disorders of the thyroid gland.
- Eye tumors.
- Injuries and burns of the organs of vision.
Risk factors include old age, myopia and farsightedness, heredity, and dilated pupils. People with small eyes and of East Asian descent are also more susceptible to glaucoma. This is due to the fact that the anterior ocular chamber has smaller volumes.
Symptoms
Almost all types of glaucoma, especially in the early stages, are asymptomatic. For this reason, patients turn to a specialist late, when the disease is already quite advanced and has already provoked irreversible changes in the optic nerve.
The main symptoms by which glaucoma can be recognized are as follows:
- narrowing of the boundaries of the peripheral field of vision;
- disturbances in the visual field, rainbow circles may appear when looking at the light.
At the same time, visual acuity can remain high.
Glaucoma is dangerous because at first it may not manifest itself in any way. If the patient notices a narrowing of the field of vision, it is already at fairly advanced stages. Only an ophthalmologist can determine the disease in the initial stages, so it is important to undergo regular preventive examinations. This especially applies to people over 40 years of age.