Doctor Vadim Berezhnoy
Founder of the MediGlobus platform. Medical expert, Head of the department of coordinating doctors.
Ocular melanomas account for approximately 5-7% of the total number of melanoma cases. A tumor of melanocytes that affects the eye progresses very quickly, grows into neighboring tissues and metastasizes early. From the article you will learn about the types of tumors, as well as the methods and prognosis of treating ocular melanoma.
Forms of damage to the ocular choroid
The nodular form of ocular melanoma is most often diagnosed. It looks like a spongy mass with a bumpy surface. The outbreak grows slowly (more than a year). As the tumor grows, it can affect most of the iris and the entire area of the anterior eye chamber. In addition, spread to the ciliary body is likely. The entire iris may be affected; the formation of daughter pathological nodules is possible. A common point of localization is the iris; metastases are rare.
The anular form of cancer of the iris has a specific course. Progresses in the border area between the iris and the ciliary body. The tumor is characterized by circular growth, simultaneously affecting the iris, the entire angle of the anterior eye chamber and the ciliary body. At first, the iris pattern looks compressed, and its shade may change. As the tumor progresses, it extends beyond the eyeball.
Forecast
The cellular composition of melanoma does not affect the clinical course of the tumor process, however, such signs as the mitotic index, the level of invasion into the dermis, ulceration and some others have prognostic significance. The depth of melanoma invasion remains the best prognostic indicator. This is the basis for the calculation of the five-year survival rate of patients with this tumor (Five Year Survival FYS). An important role is also played by the age and gender of the patient (women have a better prognosis), tumor location, lymph node involvement, as well as the presence of tumor suppressor genes (CDKN2A, CDK4) and proliferative markers (PCNA, Ki-67).
| 0.00 - 0.75 mm | 96% — 98% | |
| IB (localized) | 0.76 - 1.5 mm | 87% |
| IIA (localized) | 1.5 - 2.49 mm | 75% |
| IIB (localized) | 2.5 - 3.99 mm | 66% |
| III (metastases to regional l.u.) | > 4.00 mm | 20% — 45% (**) |
| IV (distant metastases) | 8 — 10% |
| 100% — 98% | |
| Level II | 96% — 72% |
| Level III | 90% — 46% |
| Level IV | 67% — 31% |
| Level V | 48% — 12% |
| . | . |
(*) - AJCC - American Joint Committee on Cancer (**) - 45% if 1 lymph node and 20% if 2 lymph nodes.
Prognosis of five-year survival depending on ulceration, depth and metastases to lymph nodes. According to the AJCC
| Depth of invasion (mm)* | With ulceration | No ulceration |
| less than or equal to 1.0 | 91% | 95% |
| 1,01 – 2,0 | 77% | 89% |
| 2,01 – 4,0 | 63% | 79% |
| more than 4.0 | 45% | 67% |
| Number of lymph nodes involved | ||
| 1 | 52% | 69% |
| 2 — 3 | 50% | 63% |
| 4 or more** | 37% | 27% |
(*) Without involvement of lymph nodes. (**) With or without ulceration.
Melanoma of the iris
Typically found at the bottom of the eye. Progresses in one of three forms: nodular, diffuse or planar. The pathogenic formation has pigment, its color is uneven, and progression is slow. As the lesion develops, it affects a large area of the iris; The ciliary body may be affected. A flat tumor lesion grows deep into the choroid. The shape of melanoma is similar to a cup. The lesion progresses slowly, without affecting visual functions. In later stages, retinal detachment occurs; inflammation rapidly spreads beyond the boundaries of the eyeball.
Options
Melanoma, tumor cells in the reticular layer of the dermis
Skin melanoma
Clinical forms:
- Superficial spreading melanoma
, 70% of cases: usually develops in women, is characterized by horizontal growth and generally has a favorable prognosis. - Nodular melanoma (nodular)
, 15%: more often in men, characterized by growth in the thickness of the skin, is considered the most unfavorable type in terms of prognosis. - Acrolentiginous melanoma
(lat. Acral Lentigo Maligna) 10%: also known as subungual melanoma. It also grows on the tips of the fingers and palms. It occurs most often in dark-skinned individuals. - Lentiginous melanoma
, (lat. Lentigo Maligna, Hutchinson's malignant freckle, Dubreuil's melanosis) 5%: develops against the background of a pigment spot (mole), usually on the face, mainly in women. It is characterized by horizontal, slow growth and has the most favorable prognosis. - Achromatic melanoma (non-pigmented)
is very rare.
Other melanomas
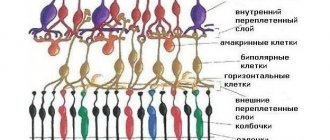
Melanoma of the retina Melanoma of the retina Lentiginous melanoma of the mucous membranes
- 1% of the total number of melanomas.
It is found in the nasal, oral, perianal and vulvovaginal areas. Characterized by pronounced, uneven pigmentation. Malignant melanoma
of soft parts or clear cell sarcoma - grows on ligaments and aponeuroses. It occurs in all age groups, including children and adolescents.
Conjunctival damage
Formed from moles. This type of cancer progresses slowly. Metastasis occurs gradually through hematogenous and lymphogenous routes. Rarely, this type of melanoma grows into the eye. There is also a specific group of ocular cancer pathologies called uveal tumors. Uveal melanoma of the eye is a tumor formation that involves the ocular choroid, iris, and ciliary body. Quite often, specialists find it difficult to determine the specific type of melanoma without proper microexamination of the samples.
Notes
- Turkington R.W.
FAmilial factor in malignant melanoma // JAMA. — 1965-04-12. - T. 192, issue. 2. - pp. 77–82. — ISSN 0098-7484. — DOI:10.1001/jama.1965.03080150007001. - WHO, Fact Sheet No. 305 December 2009 “Ultraviolet Radiation and Child Health”
- ↑ 1 2 3 4 Chissov V.I., Starinsky V.V., Petrova G.V. (editorial board).
Malignant neoplasms in Russia in 2008 (morbidity and mortality), 256 p. — M.: FGU “MNIOI im. P. A. Herzen Rosmedtekhnologii", 2010. - ISBN 5-85502-024-X. - Bale, SJ, Dracopoli, NC, Greene, MH, Gerhard, DS, Housman, DE Linkage analysis of melanoma and dysplastic nevus syndrome with polymorphic loci on human chromosome 1p. (Abstract) Cytogenet. Cell Genet. 46:575, 1987.
- Bale SJ, Dracopoli NC, Tucker MA, Clark WH Jr., Fraser MC, Stanger BZ, Green P., Donis-Keller H., Housman DE, Greene MH
Mapping the gene for hereditary cutaneous malignant melanoma-dysplastic nevus to chromosome 1p. (English) // The New England journal of medicine. - 1989. - Vol. 320, no. 21. - P. 1367-1372. — DOI:10.1056/NEJM198905253202102. - PMID 2716782. - Hussussian CJ, Struewing JP, Goldstein AM, Higgins PA, Ally DS, Sheahan MD, Clark WH Jr., Tucker MA, Dracopoli NC
Germline p16 mutations in familial melanoma. (English) // Nature genetics. - 1994. - Vol. 8, no. 1. - P. 15-21. — DOI:10.1038/ng0994-15. - PMID 7987387. - Oncologists from Tel Aviv University are on the verge of a revolutionary discovery in the treatment of melanoma. Tel Aviv's first medical center
. telaviv-clinic.ru (January 27, 2017). - Israeli scientists are closer to creating a cure for melanoma (August 23, 2016).
- Viruses show new promise in treating cancer Medical Xpress. September 13, 2018
- IMMUNOTHERAPY IS THE BEGINNING OF A “NEW ERA” IN CANCER TREATMENT. euroonco.ru. Retrieved June 16, 2015.
- Scientists uncover new pharmaceutical strategy for treating melanoma (English) (May 6, 2015). Retrieved May 13, 2015.
- "Keydruda" - now also for the treatment of lung cancer. www.isramedportal.ru. Retrieved February 3, 2021.
- Clinical trials of the drug "Keytruda". www.isramedportal.ru. Retrieved February 3, 2021.
- Creams with a high sun protection factor reduce the risk of melanoma by 33% (Russian). purederma.ru. Retrieved May 29, 2021.
- Reza Ghiasvand, Elisabete Weiderpass, Adele C. Green, Eiliv Lund, Marit B. Veierød.
Sunscreen Use and Subsequent Melanoma Risk: A Population-Based Cohort Study // Journal of Clinical Oncology. — 2016-09-30. - T. 34, issue. 33. - pp. 3976–3983. - ISSN 0732-183X. — DOI:10.1200/JCO.2016.67.5934.
Symptoms of eye melanoma
It begins with the appearance of a colored formation, similar to a mushroom on a stalk. The lumpy surface of this “mushroom” often has cracks. In the early stages of progression, many types of melanoma are asymptomatic. This is their main danger - the lesion is detected even when treatment may be ineffective.
Sometimes the following symptoms may be present:
• a dark spot on the iris that gradually grows; • visual defects (spots, flashes may be visible); • change in pupil shape; • decreased visual functionality; • loss of peripheral vision.
All visual defects are a signal that you need to contact an ophthalmologist. Indicators of ocular melanoma can be classified based on the stages of pathology progression.
At the 1st stage, there are no strong deviations in the condition. Starting from the 2nd stage, the first significant complications may appear. Stage 3 of ocular melanoma is characterized by tumor formation extending beyond the eyeball. A forward displacement of the apple is developed. The walls of the orbit may collapse and intraocular pressure may decrease. Possibly a violation of the integrity of the sclera. At the 4th stage, metastasis begins, quickly affecting various organs. Indicators of metastasis are regional lymph glands, which quickly increase in size. The patient loses weight and begins to experience pain. Vitreous hemorrhage may be present. Certain types of melanoma lesions are discovered incidentally during routine eye examinations. Retinal detachment is possible (although rare).
Advantages of Top Assuta
- Oncologists and ophthalmologists with extensive clinical experience. Our specialists are experts in the field of treatment of malignant eye pathologies and are well known in scientific and medical circles.
- An examination within a few days using modern technology allows you to accurately determine the location of the tumor and plan the most appropriate type of treatment.
- Therapy using modern techniques such as various types of endoscopic operations, contact radiotherapy, radiosurgery, thermotherapy.
- Each patient in the clinic uses the help of a free translator-curator (coordination of doctors and medical personnel, translation of documents, resolution of organizational issues). Comfortable rooms and individual treatment for each guest of the clinic.
- 5
- 4
- 3
- 2
- 1
(6 votes, average: 3.5 out of 5)
Diagnosis of melanoma cancer
It is quite difficult to detect eye melanoma, because at first it is similar to other pathological processes. In many cases, people come to the ophthalmologist because of age-related vision deterioration or abnormal visual effects. A specialist with extensive experience can detect early melanoma, but this requires additional diagnostic measures.
The list of such events includes:
• Ophthalmoscopy is a fundamental diagnostic technique. With its help, you can detect suspicious formations in the visual organs. • Fluorescein angiography is a research technique that allows you to assess the condition of the vessels of the eyeball. This activity is carried out in the following way: a dye is injected into the human circulatory system. After a few seconds, this substance is distributed throughout the body. Then, using a special lamp, the specialist examines the eye vessels and finds out whether there are any defects in their structure. • Diaphanoscopy – examination of the iris, lens, and cornea using a light source. • Radioisotope diagnostics – a special isotope solution is injected into the circulatory system. Thanks to this solution, it is possible to detect the oncological focus, which accumulates the injected isotope much faster than other components. • Ultrasound examination – performed using a small probe that emits and receives sound waves. The resulting echo forms an image reproduced on the monitor screen. • Histological examination - usually performed after surgery, which can lead to the formation of metastases.
Content
- 1. History
- 2 Epidemiology
- 3 Risk factors and causes 3.1 Human skin phototypes (According to Fitzpatrick)
- 4.1 Skin melanoma
- 8.1 Microstages according to Clark 1967
- 9.1 Initial melanoma (without regional and distant metastases)
Treatment of eye melanoma
Any therapeutic measures can be taken only after a thorough examination and an accurate diagnosis. In current medical practice, various methods are used to eliminate melanoma, among which surgery is considered the most effective. During such an intervention, the cancer focus and nearby healthy tissue are removed. The tumor is excised along with the subcutaneous tissue. Also, the muscle fascia is often excised. The surgical team believes that removing the fascia is not necessary, so they leave it in place. Resection of nearby lymph nodes is almost always performed. Such operations are carried out using a microscope, which increases the accuracy of the manipulations performed.
Risk factors and causes
Graphic representation of the CDK4 gene
- Ultraviolet radiation: natural (solar) and from artificial sources (tanning equipment). Is the leading risk factor.
- Phenotype - white skin, light (blue) eyes, blond hair and pink freckles.
- A history of sunburn. Moreover, even those of them (burns) that were received in childhood, adolescence and young adulthood can play a fatal role in the development of the tumor in subsequent years.
- Melanoform nevus (synonyms: dysplastic melanocytic nevus, atypical nevus syndrome). Refers to benign skin tumors.
- Heredity - family history of melanoma. In 1987-1989[4][5], the first susceptibility locus for familial cutaneous melanoma (CMM1) was mapped to band 36 of human chromosome 1 (1p36), but in 1994 the association of the 1p36 locus with familial melanoma was confirmed doubtful[6]. Currently, the increased risk of melanoma is associated with dysfunction of tumor suppressors, one of which is CDKN2A, a locus of chromosome 9p21, encoding proteins p16 and p14ARF, and the second is the CDK4 gene (cyclin-dependent kinase 4) localized on chromosome 12q14.
Graphic representation of the CDKN2A gene
- Nevi - According to the Research Institute of Oncology named after. prof. N.N. Petrova, among patients with an established background for the development of melanoma, the following types of nevi were named: complex (45%), borderline (34%), intradermal (16%), blue nevus (3.2%). Moreover, 70% of nevi were regarded as congenital, and 30% as acquired.
- The factor of multiplicity of nevi (more than 50) increases the risk of developing melanoma.
- Xeroderma pigmentosum.
- Already previously suffered melanoma.
- Age over 50 years.
Phototypes of human skin (According to Fitzpatrick)
The relative risk of developing melanoma is associated with skin phototype. At the same time, those with phototypes I and II are most susceptible to developing a tumor, and those with phototypes V and VI are the least susceptible, which, however, does not completely exclude the possibility of the disease in them.
| Skin phototype | Reaction to radiation |
| I | Sunburn always occurs after a short (30 min.) exposure to the sun; a tan is never acquired. |
| II | Sunburn occurs easily; tanning is possible, although difficult. |
| III | Minor burns may occur; a good even tan develops. |
| IV | There is never a sunburn; Tanning occurs easily. |
| V | Naturally dark skin. |
| VI | Black skin of people from the African continent. |
Literature
- Shanin A.P.
Diagnosis and treatment of malignant skin tumors. — L.: Medgiz. Leningr. department, 1957. - 168 p. — (Library of a practical doctor). - Shanin A.P.
Pigmented tumors. — L.: Medgiz. Leningr. department, 1959. - 260 p. - Ganina K. P., Naleskina L. A.
Malignant melanoma and previous skin changes / Academy of Sciences of the Ukrainian SSR, Institute of Problems. oncology named after R. E. Kavetsky. - Kyiv: Naukova Dumka, 1991. - 168, [48] p. — 1160 copies. — ISBN 5-12-002070-4. - Fradkin S.Z., Zalutsky I.V.
Skin melanoma. - Minsk: Belarus, 2000. - 224 p. — 5000 copies. — ISBN 985-01-0323-X. - Romanova O. A.
Early diagnosis and prevention of skin melanoma: Guide-atlas. - M.: Medical Information Agency, 2012. - 96 p. — 1000 copies. — ISBN 978-5-8948-1910-5.