Doctor Vadim Berezhnoy
Founder of the MediGlobus platform. Medical expert, Head of the department of coordinating doctors.
Ocular melanomas account for approximately 5-7% of the total number of melanoma cases. A tumor of melanocytes that affects the eye progresses very quickly, grows into neighboring tissues and metastasizes early. From the article you will learn about the types of tumors, as well as the methods and prognosis of treating ocular melanoma.
What types of eye melanomas are there?
Melanoma of the eye can have different localizations. The degree of malignancy depends on which part of the eye is affected by the tumor:
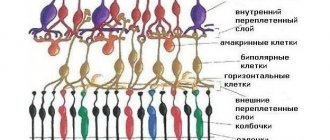
- malignant neoplasm of the eyelid - a rare and most malignant type of tumor; tumor of the conjunctiva of the eye - a rare tumor with high malignancy; melanoma of the choroid (tumor of the choroid of the eye - 85% of cases; melanoma of the iris - 6%; cancer of the ciliary body of the eye - 9%) - it is a tumor with this localization that is often mistakenly called retinal melanoma. These are less malignant tumors, but still have a high mortality rate.
Causes of disease development
Pathological processes of the choroid are associated with factors such as:
- general infectious diseases (tuberculosis, toxoplasmosis, influenza);
- the presence of foci of chronic inflammation in the body (caries, inflammation of the tonsils, sinusitis);
- heredity;
- allergic reactions;
- injury to the tissues of the organs of vision (mechanical factor, burn);
- hypothermia and associated weakening of the immune system;
- endocrine pathologies (diabetes mellitus).
Prolonged contact with ultraviolet rays is a predisposing factor that can provoke the development of choroidal pathologies, including tumor processes.
What types of eye melanomas are there?
Let's look at the stages of the most common eye tumors that form in the choroid of the organ:
Tumor of the choroid of the eye:
T1A – early stage ocular melanoma, the tumor has a size of up to 7x3 mm;
T1B – neoplasm reaches 10x3 mm;
T2 – tumor size is 15x5 mm, it extends beyond the boundaries of the outer capsule of the eye;
T3 – malignant neoplasm reaches 15x5 mm;
T4 – metastases in distant organs are diagnosed.
Tumor of the ciliary body:
T1 – early stage eye melanoma, the tumor is located within the ciliary body;
T2 – oncological process extends to the iris/anterior chamber of the eye;
T3 – tumor grows into the choroid;
T4 – metastases in other organs are diagnosed.
Tumor of the iris:
T1 – the tumor is localized within the boundaries of the iris;
T2 – the oncological process reaches the 1st quadrant and the angle of the anterior chamber of the eye;
T3 - tumor affects a pair of quadrants, anterior chamber angle, choroid or ciliary body;
T4 – the oncological process extends beyond the boundaries of the eye, the process of metastasis is in progress.
↑ Results and discussion
In the main group, 2 patients after independent BT successfully underwent repeated courses of BT (including triple irradiation in one case) due to partial regression of MX and signs of continued growth. The terms of re-treatment are 31 and 43 months. Visual acuity in patients after organ-preserving treatment ranged from 0 to 1.0 (average 0.12 + 0.24).
Detailed characteristics of MX and patients in whom metastases were detected after organ-sparing treatment and after primary enucleation are presented in Table. 1 and 2.
According to the Kaplan-Meier analysis (log-rank test), the 5-year rate of metastasis (specific survival) after organ-sparing treatment was 16%, after enucleation - 13% with no significant differences between groups (p> 0.96; see figure ).
Treatment methods for eye melanoma
The treatment program for melanoma of the retina, or more correctly the choroid, depends on the location of the tumor, the stage of the oncological process, concomitant diseases and the general health of the patient. The main treatment for ocular melanoma is surgery.
Excision of the tumor can be complemented by radiation therapy, chemotherapy, and treatment with targeted drugs. These methods can be prescribed both before and after surgery.
Surgery for choroidal melanoma of the eye involves excision of the tissue affected by the tumor and a small amount of surrounding healthy tissue, or enucleation (total removal) of the eyeball at advanced stages. Treatment of choroidal melanoma also involves radiation therapy.
If the tumor is localized within the boundaries of the choroid and its small size, it is possible to destroy the tumor using a laser, low or high temperatures: laser and diathermocoagulation, cryodestruction, etc.
Radiation therapy, as well as radiosurgery and brachytherapy, are effective for ocular melanoma. Using the CyberKnife radiosurgical unit, it is possible to perform organ-saving surgery for non-surgical tumor removal. Brachytherapy for eye melanoma also allows you to destroy the tumor, preserving the organ and more than half of its functions. To do this, a radiation source is placed in the eye tissue, which destroys the tumor, and then removed.
Diagnostics
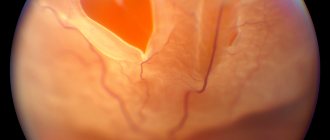
In the initial stages of the disease, diagnosis is very difficult. It is alleviated when the neoplasm is ophthalmoscoped, like a pigmented nodule protruding into the vitreous body. This provokes the occurrence of progressive hypermetropia. An increase in the size of the protrusion, a change in the contours of the affected area, an increase in the degree of pigmentation, as well as the appearance of implantation nodules in the choroid indicate the growth of melanoma. This is also evidenced by an increase in the size of the scotoma, progressive deterioration of vision, as well as the appearance of retinal detachment.
In order to recognize the disease, as a rule, biomicrophthalmoscopy, diaphanoscopy (regular and “bloody”), radioisotope and ultrasound examinations are prescribed.
Differential diagnosis of melanoma is carried out with choroidal nevus, hemangioma, proliferative senile degeneration, neurofibroma, and infectious granuloma.
Nevus is usually not accompanied by protrusion into the vitreous body, growth of the formation, and there is no scotoma. Proliferative senile degeneration of the macular region differs from melanoma in periodic hemorrhages and a bilateral process. Choroidal hemangioma is usually accompanied by similar tumors in other tissues and organs (skin, mucous membranes). Neurofibroma of the choroid is characterized by neurofibromatosis with its numerous clinical manifestations.
The difference between an infectious granuloma of the choroid is a small amount or absence of pigment, the rapid development of the process, the presence of inflammatory phenomena, and slight opacification in the vitreous body. To establish the correct diagnosis, a general examination of the patient and laboratory tests are prescribed.
Prognosis for eye melanoma
An important question for every person who has learned about his diagnosis: how long do people live with eye melanoma? The 5-year survival prognosis for early retinal (correctly choroidal) melanoma reaches approximately 80%. However, everything depends on the size of the tumor, the degree of invasiveness and location. For people with ocular melanoma that has spread to distant areas of the body, the 5-year relative survival rate is only 10-15%.
The highest survival rate is recorded for melanoma of the iris. However, it is more rare than other types of melanoma.
The chances of successfully treating melanoma largely depend on its size. Thus, with choroidal melanoma of the eye, the 5-year survival prognosis for people with small choroidal melanoma (stage 1) reaches 84%. The 5-year survival rate for people with medium choroidal melanoma (stage 1) is 68%, and the 5-year survival rate for people with large choroidal melanoma (stage 2) drops to 47%.
Regarding the occurrence of relapse in ocular melanoma, patients with a tumor less than 0.76 mm have the lowest risk of the disease returning. For tumors ranging in size from 0.76-1.5 mm or larger, the risk of relapse increases significantly.
Recurrence of iris melanoma with metastasis to distant organs is less common than with choroidal melanoma. Within 5 and 10 years after treatment, metastases from iris tumors are found in only 4.1% and 6.9%, respectively, compared with 15% and 25% for choroidal melanomas.
↑ Material and methods
A comparative analysis was carried out in 2 groups of patients. The main group consisted of patients who received organ-preserving treatment in the form of independent BT or BT with simultaneous TTT (BT + TTT). The BT and BT + TTT techniques were described previously [4, 10]. The control group consisted of patients with MX who underwent enucleation as primary treatment.
The criteria for inclusion in the analysis were MX height of more than 6.0 mm, follow-up period after treatment of at least 1 year, absence of signs of MX metastasis before treatment, confirmed metastases after treatment. Due to the fact that organ-preserving treatment was not carried out for tumors with a height of more than 10.5 mm, in cases of MX spread to the root of the iris, when the tumor covers the optic nerve head or involves the latter in the tumor process, in secondary glaucoma, extrascleral spread of MX, the corresponding patients did not were also included in the control group.
For a correct comparative analysis and obtaining reliable results, the groups were standardized according to the following main indicators that have an impact on metastasis and survival rates: by age of patients, MX sizes - height and maximum base diameter, by the number of tumors with unfavorable localization - juxtapapillary and ciliochoroidal and follow-up periods .
As a result, the main group (organ-preserving treatment) consisted of 39 patients (21 men and 18 women) aged from 39 to 74 years (average 54.3 + 9.0 years); 17 (44%) patients were under 50 years of age. 20 patients were treated using BT as monotherapy, and 19 were treated using the combined method (BT + TTT).
In the main group, the tumor height ranged from 6.9 to 10.5 mm (average 8.4 ± 1.03 mm), the maximum base diameter ranged from 9.6 to 18.9 mm (average 13.7 ± 2. 3 mm). There were 3 juxtapapillary tumors, 6 ciliochoroidal tumors. The maximum follow-up period was 98 months, median 48 months. Conducting organ-preserving treatment in patients with an MX height of more than 10.0 mm and a base diameter of more than 16.0 mm (11 patients) was explained by their categorical refusal of enucleation.
The control group (enucleation) consisted of 28 patients (9 men and 19 women) aged from 32 to 75 years (average 58.6 ± 10.4 years); 6 (21%) patients were under 50 years of age. The MX prominence ranged from 6.7 to 10.5 mm (average 8.8 ± 1.1 mm), the maximum diameter of the tumor base ranged from 7.4 to 18.5 mm (average 13.6 + 3 ,2 mm). 6 patients had juxta-papillary tumors, 5 had ciliochoroidal tumors. The maximum follow-up period in this group was 156 months, the median was 47.5 months.
Thus, groups of patients were formed that were statistically homogeneous by age (p - 0.063), including the number of patients under 50 years of age (p > 0.1), average MX height (p > 0.149), average maximum base diameter (p > 0.85), number of tumors with unfavorable localization (juxtapapillary and ciliochoroidal; p = 0.246 by x2 criterion), follow-up period (p > 0.23).
Where can I get treatment for eye melanoma?
The most effective treatment for eye melanoma is in Israel.
The structure of the famous Israeli clinic Assuta includes the specialized center Melanoma Unit. All types of melanomas are treated here, including eye melanoma. The clinic uses modern therapy protocols, including TIL (tumor infiltrating lymphocytes) - a treatment tactic that involves the use of immune resources in the fight against a tumor. In addition, the center offers modern surgical removal of tumors, cryo- and laser surgery. They also use SIRT therapy, which involves introducing a radiation source directly into the tumor. Melanoma Unit is a specialized center that brings together the best doctors in Israel with the appropriate specialization: oncodermatologists, oncosurgeons, and radiation therapy specialists. Among them are such famous doctors as prof. Yakov Shekhter
and prof. Chaim Gutman.
You can learn more about new treatment methods by leaving a request on our website. The MediGlobus coordinator will contact you as soon as possible and provide free consultation on any questions regarding the treatment of ocular melanoma abroad.
OncologyOphthalmology
Doctor Vadim Berezhnoy
Founder of the MediGlobus platform. Medical expert, Head of the department of coordinating doctors.
Lydia Artemenko
Editor
She has been working in the field of copywriting for more than 5 years, and has been writing texts about medical tourism for the website for about 1 year. For her, the ideal day off is a family walk in the park with her favorite dachshund. In his free time he enjoys handmade crafts, loves to knit, crochet, and bead embroidery.
Classification
By the nature of education there are:
- benign;
- malignant.
The disease is diagnosed in two types:
- vascular.
- pigmented.
Pigmented types of tumors, in turn, can be of two types:
- progressive;
- stationary.
In addition, there is a general classification of this group of pathological processes, which implies their division into the following types:
- nevus of the choroid of the eye.
- choroidal hemangioma.
- uveal melanoma.
In turn, hemangioma is divided into two subtypes:
- diffuse;
- limited.
Each form has its own characteristic clinical course.