Causes of microphthalmos
The main causes of microphthalmia are associated with intrauterine developmental disorders of the fetus.
The main provocateurs of the disease are infectious pathologies of the reproductive organs in women. In addition, hereditary pathologies are an increased risk factor. The causes of the isolated nature of the pathology include intrauterine infections:
- toxoplasmosis;
- rubella;
- herpes.
The cause of microphthalmia can be isolated or genetic pathologies.
The main etiological provocateurs are:
- TORCH infections.
The four most dangerous intrauterine diseases (toxoplasmosis, rubella, herpes). Infectious agents of these pathologies penetrate the fetal bloodstream, thereby provoking the development of many defects; - Teratogenic effects.
Microphthalmos is caused by the influence of ionized rays, smoking, alcohol consumption, and specific medications on the fetus; - Amniotic fusions.
These are constrictions in the form of dense threads that are localized in the amniotic sac. Such threads compress the fruit. Such an effect entails a reduction in the eyeball or a complete absence of development of the fetal organ at various stages of pregnancy; - Genetic pathologies.
Pathologies associated with genetic mutations (Temple Al-Ghazali, Delleman, Peters, Rieger syndromes). These diseases lead to the development of many abnormalities, including microphthalmia.
Nevertheless, the main cause of microphthalmia is teratogenic factors. The high-risk group includes women whose work involves interaction with toxic substances. Also, the consumption of narcotic substances significantly contributes to the development of underdevelopment of the visual organs of the fetus.
The stage of disruption of the embryogenesis process depends on the time of influence of pathogenic factors on the fetus.
Treatment options
In most cases, treatment is not aimed at eliminating the problem, but at stopping the development of pathology .
For this, older patients are prescribed to wear telescopic glasses .
But in cases of development against the background of microphthalmos, cataracts, glaucoma or retinal detachment, such measures will be ineffective, and only surgical intervention is indicated for patients.
In such cases, it is also impossible to get rid of the pathology as such, and the goal of doctors in this case is to exclude the development of secondary disorders and diseases.
There are several types of operations for microphthalmia:
- Implantation of a skin-fat or synthetic implant . It is performed in the most severe cases, when it makes no sense to preserve the affected organ.
- Cosmetic ophthalmic prosthetics. Partial implantation is performed using thin-walled prostheses. In such cases, the quality of vision does not improve, but the eye can be given a normal size and shape, while maintaining the mobility of the organ.
- Posterior scleral band. This type of surgery is indicated for minor development of microphthalmos. The essence of the operation is to install strips of allograft (donor tissue) under the rectus muscles of the eye. Such strips are attached to the episclera.
Remember! Surgical intervention does not guarantee complete elimination of the consequences of microphthalmos, and in each case the need for repeated intervention by surgeons cannot be ruled out.
Also, in case of the disease, drug treatment is used to exclude secondary complications. But it comes down only to regular injections of antiseptic solutions into the under-eye area.
Symptoms of microphthalmos
The most common symptom of microphthalmos is a unilateral reduction of the eyeball.
Basically, similar symptoms are observed in infants immediately after removal from the mother’s womb, since the etiology of the disease is congenital. In addition to deformation of the eyeball, microphthalmos is characterized by the following painful effects:
- decreased visual acuity;
- frequent tearing;
- facial asymmetry;
- discomfort;
- pain in the eye, with cysts formed between the membranes of the visual-sensory organ.
In the presence of microphthalmos, a defect may develop in which part of the eye shell is missing (coloboma).
This pathology provokes damage in various areas of the eye organ, including:
- iris;
- retina;
- vision receptors that transmit visual information to the brain.
The presence of coloboma occurs in both one and both eyes. Pathology of direct images contributes to impaired visual perception.
Symptoms
Most often, with microphthalmia, a unilateral decrease in the size of the eye is observed, but bilateral processes can also be diagnosed. A visible defect in appearance is associated with a significant decrease in the size of the eyeball and often it does not exceed 1 cm. The organ of vision becomes irregular in shape, the transparency of the cornea decreases, and it noticeably thickens. Only in rare cases does the corneal diameter exceed 6 mm.
Sometimes microphthalmia is diagnosed with correct formation of the eye, but more often additional malformations of the organ are detected. With microphthalmia, the following symptoms may develop:
- increased intraocular pressure;
- glaucoma;
- decreased vision;
- ectasia of the sclera of the posterior wall;
- Lenticonus.
When the pathology progresses to an advanced form, retinal detachment may be detected. With a significant decrease in the size of the eye, deformation of the facial bones is observed. A patient with microphthalmia may have drooping eyebrows, raised wings of the nose and corners of the mouth on the affected side. In the absence of timely treatment, facial asymmetry worsens as the child grows.
Classification of microphthalmos
The disease is classified into 2 categories: unilateral and bilateral microphthalmos. The most common form is the first option. The second occurs in 10% of the total number of sick children.
In addition, the types of pathology are divided into idiopathic and hereditary disorders. The first option means that doctors were unable to identify the etiological factors of the disease. Hereditary microphthalmos manifests itself in newborn infants when the development of pathology occurs in an autosomal dominant or autosomal recessive manner.
There are two degrees of severity of the pathology: ordinary and combined microphthalmia. Pathology of a simple type occurs without anomalies and third-party diseases. The complex form means the presence of other concomitant disorders affecting the anterior region of the eye. Consequently, the latter option is characterized by a more complex form.
Approximately up to 50% of patients have concomitant ophthalmological diseases. In most patients, along with microphthalmia, cryptophthalmia develops (complete, incomplete, abortive) proliferation of an orbital cyst.
Another form of microphthalmos is nanophthalmos. This form of pathology is characterized by a reduction in the eyeball with thickening of the scleral capsule, the manifestation of severe farsightedness and an increased risk of developing glaucoma.
Classification of the disease
Most often, patients are diagnosed with unilateral damage to the eyeball, and only in some cases - bilateral. Microphthalmos is considered a frequent manifestation of genetic pathologies occurring in the body. Isolated microphthalmia is divided into the following types:
- Idiopathic. A diagnosis such as “idiopathic microphthalmia” indicates that it was not possible to find out the cause of the disease. In addition, an idiopathic disease eliminates the impact of adverse factors on the fetus during its intrauterine development.
- Hereditary. Taking into account the type of inheritance, this type of disease is classified into autosomal recessive, autosomal dominant and X-linked. The variety of modes of disease transmission explains the high prevalence of microphthalmia.
Diagnosis of microphthalmos
Microphthalmos has a pronounced visual character. Consequently, the presence of the disease is noticed very easily.
The final diagnosis is established by an ophthalmologist or pediatrician during a postpartum external structural examination of the child’s eye. To record the disease, the pediatrician opens the baby’s eyelids and examines the outer tissue of the eyeball. If a unilateral type of lesion is detected, the other eye is extensively examined for the presence of additional defects and anomalies that may lead to deterioration of visual functions.
It is not always possible for a doctor to determine the cause of the development of pathology. Therefore, often an additional influencing factor is determined through diagnostic methods using hardware equipment - ultrasound, MRI.
Considering the fact that microphthalmia is often caused by genetic pathologies, a DNA analysis can be performed, in which a blood sample and buccal epithelium are examined.
To diagnose the disorder, the following medical and ophthalmological methods are used:
- Biomicroscopy.
To diagnose the disease, the condition of the palpebral and orbital conjunctiva is assessed, the anterior part of the eyeball is examined, and the level of opacification of the optical media is determined; - Visometry.
Allows you to evaluate visual acuity using special tables (for example, Sivtsev - Golovin); - Refractometry.
The procedure is aimed at an objective assessment of the optical functions of the eye and identification of refractory anomalies using special refractometer devices.
After confirmation of the diagnosis, consultative participation of a geneticist is indicated. Modern medicine has the capabilities of prenatal examination of the visual apparatus. Microphthalmos is diagnosed differentially with underdevelopment of the eyelids and eyeball (cryptophthalmos) and complete or partial absence of the eyeball (nanophthalmos).
Complications
If prosthetics are not performed in time for the congenital form of the disease, then later this may cause facial asymmetry. In this case, drooping of the eyebrows is observed. As the child ages, these symptoms only worsen. In the future, this can cause disruption of chewing functions and normal breathing.
If in the place where the eyeball should have been, its rudiment is observed, then this can cause the development of infection and other inflammatory processes. The risk of developing orbital phlegmon and abscess increases. There is only one way to avoid complications - consult a doctor in a timely manner. Otherwise, it will only worsen the patient's well-being.
Other systemic disorders may also appear. To prevent unwanted consequences, doctors can use surgery. Especially when suspicious signs develop. Drug treatment is used as an adjuvant therapy.
Improper treatment can cause the development of such complications: internal hemorrhages, swelling, damage to the optic nerve. Therefore, you should only contact qualified and experienced doctors.
Treatment of microphthalmos
The doctor thinks over the treatment tactics for microphthalmia, based on the degree of underdevelopment of the eye tissues and the duration of the pathology. The therapy paradigm is based on surgical correction of the structures of the eyeball.
Surgical correction
Surgical correction methods include:
- Scleroplasty.
The indication for this operation is due to slight hypoplasia of the eye organ, namely a decrease in the eye lumen to 3 mm. During surgery, strips of special scleroplastic tissue are implanted into the posterior wall of the sclera; - Cosmetic ocular prosthetics.
It is advisable when the size of the eyeball is reduced to 5 mm. During the operation, a thin-walled prosthesis is inserted to maintain normal lability of the eyeball. For patients with increased sensitivity of the cornea, de-epithelialization of the cornea is used. During the operative procedure, the cornea is lined with a rounded allograft; - Implantation technique.
The essence of the operation is the placement of a skin-fat graft in the retro-orbital space with delayed prosthetics. Surgery is indicated when the size of the anteroposterior vector of the eyeball does not exceed 10 mm.
Important!
Surgery is permitted for patients at least 7 years of age. Surgical intervention is necessary for diagnosed glaucoma, cataracts, and retinal detachment. In addition, the operation is performed to improve the appearance of the visual organ; prosthetics are used for this purpose.
Conservative therapy
Conservative methods of therapy are used for preventive purposes aimed at relieving residual complications with the installation of antiseptic solutions, such as:
- Miramistin;
- solutions for treating contact lenses;
- Chlorhexidine.
{banner_horizontalnyy3}
Microphthalmos
This is often a congenital pathology, usually caused by exposure to various unfavorable factors on the fetus during the period of intrauterine anlage and eyelid development. In some cases, anomalies are familial in nature and are inherited. Post-traumatic injuries and inflammatory diseases are classified as acquired pathologies.
Congenital microphthalmia is a reduction in the size of the eyeball (the rudiment of the eye or 1-2 mm less than normal), accompanied by abnormalities of the eyelids. Most often it is unilateral, in rare cases bilateral. There is a disturbance in the intrauterine anlage and development of the eyeball and eyelids, but with congenital microphthalmia, unlike anophthalmia, the rudiment of the eyeball is located in the orbital cavity.
The diagnosis of microphthalmos is made when the length of the anterior-posterior axis of the eyeball is less than normal and corresponds to 21 mm in an adult and 19 mm in a one-year-old child. The incidence of this disease (congenital anophthalmos and microphthalmos) in different countries varies from 1 to 2.1 per 10,000; it is registered in 0.4% of patients with pediatric ophthalmopathology.
Causes:
- hereditary-genetic; The type of transmission is predominantly dominant, less often recessive, sex-linked or not.
- intrauterine inflammatory processes (measles, rubella, herpes zoster, etc.);
- intrauterine degenerative processes (amniotic cords).
- manifestation of various syndromes.
Acquired microphthalmia develops secondarily in early childhood as a result of exposure to various external factors that inhibit the growth of the eyeball. These include: retrolental fibroplasia, toxoplasmosis, pseudoglioma, removal of congenital cataracts at a very early age, etc. Microphthalmos can be a consequence of X-ray irradiation of the orbital area and eyes in children.
Clinical picture
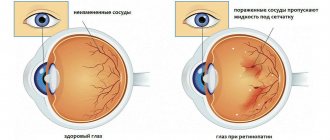
Congenital microphthalmos can be unilateral (more often) and bilateral (less often). The eyeball is sharply reduced in size - sometimes up to 1 cm in diameter, irregular in shape with a flattened, often translucent cornea, the diameter of which is 6 mm or less. The eyeball can be correctly formed and only reduced in size, or the reduction in size is combined with various malformations of the eye. In this case, the following are observed: colobomas of the vascular tract and optic nerve, aniridia, lenticonus, calcification of the lens, ectasia of the sclera in the posterior pole of the eye.
Microphthalmos can be complete, anterior or posterior.
- With complete microophthalmia, the anterior-posterior axis (APA) of the eyeball and the diameter of the cornea are reduced by 1 mm or more.
- With anterior microphthalmos (microcornea), only the diameter of the cornea is reduced by 1 mm or more with a normal size of the eye's PZO.
- In posterior microphthalmia, the size of the PZ is reduced with normal corneal diameter (rare).
Depending on the size of the eye, there are 3 degrees of microphthalmos:
- I - reduction of one or two of the above dimensions by 1.0-1.5 mm compared to the age norm;
- II - decrease by 2.0-2.5 mm;
- III - decrease by 3 mm or more.
Microphthalmic eyes are predisposed to glaucoma, and in the presence of choroidal coloboma, to retinal detachment. The refraction of the eye is most often hypermetropic. Visual acuity due to underdevelopment of the macula is low, sometimes complete blindness is observed. There are frequent combinations with other developmental defects (cleft lip, cleft palate, anomalies of the ears, fingers and toes, etc.). The diagnosis is made based on an external examination of the eye.
Treatment
Treatment Goals
- Prevention of progressive facial asymmetry.
- Correction of orbital bone growth.
- Correct formation of the conjunctival cavity and eyelids.
- Correction of a cosmetic defect.
- Getting rid of psychological trauma and normal adaptation in a team.
Non-drug treatment is considered the main one in the first years of life. It is included in stepwise orbital prosthetics with prostheses of increasing size. Prosthetics should begin as early as possible - from the first month of the patient’s life.
For hygienic purposes, antiseptic solutions are used: miramistin (INN - benzyldimethyl - myristoylamino - propylammonium) 0.01%, chlorhexidine 0.05%, as well as solutions for treating and soaking contact lenses. Sulfacetamide should not be instilled onto the prosthesis.
In the presence of glaucoma, retinal detachment or cataracts, surgical treatment is indicated in some cases. With pronounced microphthalmia and the absence of visual functions, it is possible to cover such an eye with a single-walled cosmetic prosthesis.
The prognosis for vision is unfavorable; a significant decrease in visual functions up to blindness is possible.
Prosthetics for congenital microphthalmia
Congenital microphthalmos is an anomaly that requires the attention of an ophthalmoplasticist and ocular prosthetist. Without the help of specialists, the patient will experience progressive asymmetry of the facial skeleton, which in the future will lead to limitation of social adaptation and professional activity.
From the first weeks of a child’s life, stepwise prosthetics of the underdeveloped orbit begins. Already a month after birth, parents should contact a prosthetist.
At the first visit, the conjunctival cavity looks so small that non-specialists consider it impossible to select a prosthesis. Nevertheless, prosthetics must be started. A small plastic pea is placed into the cavity. If it is poorly held in place, apply a pressure bandage.
After 3-4 days, during the second visit, a larger pea can be placed into the cavity. After another week, a microprosthesis is selected. After 1-2 weeks, a larger prosthesis is selected. Stepped prosthetics continues continuously throughout the entire period of the child’s growth, with a frequency of 1-6 months in the first years of life, after 5 years - once a year.
It is recommended to use standard-shaped prostheses so that the cavity acquires a normal shape. This is not always possible. The fact is that orbital hypoplasia is accompanied not only by a change in its scale, but also in shape. The most unfavorable property of such an orbit is the absence of a retromarginal groove, which develops in the presence of a round formation in the orbit and into which the edges of the prosthesis are placed.
The orbit in congenital microphthalmia has the shape of a bell, because of this the prosthesis tends to turn around, shift and come forward. To maintain the correct and stable position of the prosthesis, its shape is changed to mushroom-shaped. The mushroom-shaped prosthesis is better retained in the cavity.
Particular attention should be paid to maintaining the length of the palpebral fissure. It may be insufficient for inserting a large prosthesis into the cavity, and the decision to perform an external canthotomy naturally suggests itself in order to facilitate this procedure and obtain a cosmetic effect by enlarging the eye. In fact, canthotomy is extremely dangerous. A short palpebral fissure is a good deterrent for the prosthesis to fall out. Elimination of this factor greatly complicates prosthetics and forces the use of smaller prostheses. Often it is simply impossible to keep the prosthesis in the cavity. This gives rise to attempts to reconstruct the conjunctival cavity, which often further aggravate the situation.
Any operations for congenital microphthalmia should be performed by a surgeon with special skills in working with this pathology.
The effectiveness of stepped prosthetics in terms of orbital development is quite high. After 10-15 years, its size approaches normal, although it should be noted that the ratio of horizontal to vertical size on the microphthalmos side remains smaller than on the healthy side.
But the orbital problems don't end there. Prosthetics for congenital microphthalmia leads to significant changes in soft tissues.
The expansion of the conjunctival cavity is accompanied by an expansion of the space between the eyelids and the rudiment of the eyeball. This space contains structures such as the levator of the upper eyelid and the retractor of the lower eyelid. Their anatomical structure is such that stretching is accompanied by the development of inversion of the eyelids and smoothing of the palpebral fold.
Typical eyelid deformities in this pathology include inversion and flattening of the posterior edges of the eyelids, absence of the palpebral fold, and the formation of an epicanthus.
Soft tissue deformation is the subject of plastic reconstruction. The methods used to correct the cavity and eyelids are the following: enucleation and reconstruction of the orbital stump using special technology, deepening of the vaults with free mucosal transplantation, elimination of volvulus, formation of the palpebral fold and epicanthoplasty. Sometimes a small canthotomy is performed if there is a good margin of stability in the position of the prosthesis.
Complications of microphthalmos
The consequences of microphthalmos are complicated by dangerous pathologies that lead to significant visual impairment. The prolonged course of the disease provokes the formation of cysts, inflammation of the horny and conjunctival membranes (keratitis, conjunctivitis). The outcome in severe cases is complete blindness.
Additionally, microphthalmos in children leads to eye damage in the form of cataracts (clouding of the lens). Other complications of microphthalmos are narrowing of the palpebral fissure (eye opening). Pathology increases the risk factor for the development of glaucoma. Doctors have proven that congenital eye pathologies can cause malignant neoplasms in the intraorbital segment.
Characteristics of the violation
With a congenital anomaly, one eyeball is usually affected, but it happens that both are of insufficient size. It happens that the diameter is only 10 mm, the cornea thickens significantly and becomes cloudy.
Microphthalmos is often accompanied by an infectious lesion and occurs in the form of inflammation.
Time-tested therapy for eye infections - instructions for use of Levofloxacin eye drops.
Cataracts may accompany the manifestation of the disease
The pathology is often combined with other lesions in the form of:
- coloboma of blood vessels and optic nerve;
- Lenticonus;
- scleral ectasia;
- calcareous cataract.
The organ sometimes does not change shape, but the size of the apple is not normal.
Violation of the optical system provokes the appearance of hyperopia and deterioration of vision. Left untreated, it can lead to blindness.
Find out how to choose continuous wear contact lenses from the article.
Wearing telescopic glasses will help reduce the risk of complications
In addition to reducing the diameter of the eyes, with microphthalmia:
- The shape of the ears changes.
- A cleft lip is formed.
- Eyebrows droop.
- Fingers are affected.
Over time, the corners of the eyes rise, the child’s face becomes disfigured, and its asymmetry increases. With such a pathology it is very difficult to adapt to a team.
Many cysts that are located in the orbit cause unbearable pain because they put pressure on the structures of the visual organ. With microphthalmia, an infection is often associated, which leads to permanent conjunctivitis and the development of keratitis. Bacteria that have penetrated the membrane serve as causative agents of endophthalmitis.
In children who have an abnormally sized eyeball, cancerous tumors can form on the visual organ.
A dangerous symptom or sign of banal fatigue is the cause of constantly bursting blood vessels in the eyes.
Visiometry can determine the degree of vision loss in a preschooler
When treatment with Luxfen eye drops is indicated, find out here.
Causes
Among the main causes of microphthalmos are pathological processes in the womb. They can be inflammatory and degenerative in nature and often occur against the background of the development of infectious diseases. Most often the disease is inherited in a dominant way.
The disease can also be acquired. Among the main reasons in this case:
- Toxoplasmosis;
- Surgeries on the visual organs in childhood;
- Retrolental fibroplasia;
- Exposure to X-rays in childhood.