Retinal hemorrhage develops due to the influence of several causative factors. It may not cause subjective sensations in a person and remain unnoticed for a long time. In the case of retinal detachment or the development of hemorrhage in the area of the macula, visual impairment, even complete loss, cannot be ruled out. Any signs of a violation of the functional state of the eye are grounds for contacting an ophthalmologist, who will prescribe timely appropriate treatment.
Clinical symptoms
With a small volume of blood outside the macula, clinical symptoms practically do not appear. When pathological changes are localized in the area of the macula (macula), in the case of retinal detachment, the following signs of the pathological process appear:
- Discomfort with an unpleasant sensation of “pressure” in the eye.
- Decreased visual acuity, which can have varying severity.
- The appearance of a “mesh” before the eyes.
- Blurred image, double vision.
- The appearance of “floaters” before the eyes, which leads to deterioration of vision.
As the pathological condition progresses, the cloudy spot before the eyes expands, which gradually increases over time. When there is a retinal detachment or hemorrhage in the macula, visual fields are lost.
Regardless of the severity and localization of the changes, a consultation with an ophthalmologist is required, since the development of complications in the future, which may negatively affect visual acuity, cannot be ruled out.
Complications after hemorrhage
Regardless of which area of the eyeball the bleeding occurs, the pathology has a visual defect. Many patients delay visiting a doctor. Due to untimely treatment, the disease progresses rapidly, so the following complications appear:
- glaucoma;
- retinal detachment;
- disturbance of image perception;
- loss of vision (partially or completely);
- traumatic cataract;
- formation of a cataract.
These consequences are due to the toxic effects of elements formed as a result of the destruction of blood cells. To eliminate complications, radical measures are often resorted to.
Causes
Retinal hemorrhage is a polyetiological pathological condition. This means that its development is provoked by a large number of provoking factors. The reasons for the development of the pathological condition include:
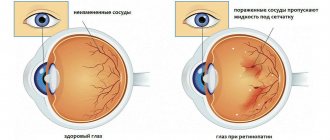
Arterial hypertension with increased systemic blood pressure. In this case, damage occurs to small arteries or structures of the microvasculature of the retina with hemorrhage.
Systemic pathology of the blood, affecting the functional state of the formed elements and coagulation - leukemia, thrombocytopenia of various origins, hemophilia.
- Increased intraocular pressure, including with open-angle or closed-angle glaucoma.
- Diabetes mellitus - a prolonged increase in blood sugar levels leads to a decrease in the strength of the walls of microvasculature vessels, resulting in an increased likelihood of hemorrhage.
- Inflammatory diseases that directly affect the retina of the eye or the vessels in it.
- Intraocular benign or malignant neoplasms.
- Systemic pathology of connective tissue, which usually has an autoimmune origin - systemic vasculitis, scleroderma, in which the immune system “erroneously” produces antibodies against its own tissues.
- Progressive myopia in the later stages of progression of the pathological process.
- Atherosclerosis of the vessels of the retina is the deposition of cholesterol in the walls of blood vessels in the form of atherosclerotic plaques, as a result of which their strength decreases.
In children under the age of one year, the pathological condition can provoke a strong cry or cough, which increases the pressure in the venous vessels of the head. In isolated cases, the pathological process was diagnosed in women during childbirth.
Knowledge of the reasons due to which the pathological condition develops helps to select effective treatment and preventive measures.
Causes of hemorrhages in the retina
The most common cause of such hemorrhage is blunt trauma (contusion) of the eye. In this case, an external mechanical force can act both directly on the eye and through the surrounding tissues (a blow to the face, head, or even the diaphragm).
Based on gravity, there are three degrees of concussion:
- Mild, when there are almost no visible manifestations, the structures of the eye are not damaged, slight swelling of the cornea and retina is observed, vision can be restored in full;
- Moderate, which is characterized by damage to eye tissue (hemorrhage under the conjunctiva and its ruptures, corneal erosion) and deterioration of vision to light perception;
- Severe, accompanied by irreversible structural changes in the tissues of the eye (ruptures of the choroid and retina, dislocation of the lens) and complete loss of visual functions.
Even mild bruises can lead to serious changes in the structure of the eyeball. Likewise, the symptoms and external manifestations of concussion do not always correspond to the actual severity of the injury. Often, hemorrhages in the visual organs accompany closed brain injuries.
The second, fairly numerous group of causes consists of common diseases:
- Atherosclerosis - the walls of blood vessels, covered with sclerotic plaques, lose their elasticity and become more susceptible to influences;
- Arterial hypertension - with increased pressure, the risk of rupture of the walls of blood vessels increases;
- Diabetes mellitus – high glucose levels lead to aneurysms (protrusion) and weakening of the vascular walls;
- Systemic connective tissue diseases (scleroderma, vasculitis, lupus erythematosus) – increase the permeability and fragility of blood vessels;
- Blood diseases (anemia, leukemia, coagulopathy) - coagulation disorders and pathological changes in blood composition have a negative effect on the walls of blood vessels.
The third group includes eye diseases directly:
- Intraocular tumors compressing blood vessels;
- Myopia (myopia) of moderate and high degree;
- Developmental anomalies and inflammatory processes of the choroid (angiopathy or retinal vein thrombosis, uveitis, iritis).
Intense physical activity can be divided into a separate group:
- Sports, cardio training;
- Attempts during childbirth;
- severe coughing or screaming;
- Shaking (especially in babies).
Kinds
Modern classification involves dividing a pathological condition into types according to several criteria. In relation to the retina of the eye, there are 3 types of hemorrhage:
- Preretinal – blood accumulates in front of the retina, a condition characterized by the appearance of a “cloudy spot” in front of the eyes.
- Intraretinal - hemorrhage occurs directly in the tissue of the retina.
- Subretinal - hemorrhage is localized behind the retina; it may not affect visual acuity if detachment has not occurred.
Read in a separate article: Eye asthenopia: what is it and how to treat
Separately, hemorrhages with retinal edema are distinguished, as well as accumulation of blood in the area of the macula, which are characterized by an unfavorable outcome.
Based on the modern classification, the doctor makes a diagnosis and selects the optimal treatment.
Diagnostics
To identify and localize hemorrhage, ophthalmoscopy is performed. First, medications are instilled into the eye in the form of drops that dilate the pupils. Then, using a special device, the doctor examines the retina.
To determine the cause of the development of the pathological process, an electrocardiogram, clinical analysis of blood and urine are additionally prescribed, blood pressure and blood glucose levels are measured. Based on all the results of diagnostic studies, the doctor selects the appropriate treatment.
Types and classification of eye hemorrhages
The classification of the disease depends on the location of blood clots in the organs of vision. In addition, the pathological phenomenon is divided based on the intensity of development:
| Severity | Main characteristics |
| Lightweight | There are no painful sensations. The structure of the organ does not change and is restored over time. |
| Average | Minor eye damage. Needs drug therapy. |
| Heavy | Serious and sometimes irreversible impairments, including loss of vision. Treatment is carried out through surgery. |
Treatment with medications
Treatment of retinal hemorrhage with medications includes the use of drugs from several pharmacological groups:
- vasoconstrictors;
- hemostatic drugs;
- vitamins K and C, which help normalize blood clotting;
- vitamin A to improve the functional state of retinal cells.
In addition to medications, a regimen must be prescribed that involves reducing eye strain. In case of pathology of the cardiovascular system, which is accompanied by an increase in the level of systemic blood pressure, antihypertensive drugs are prescribed. In the case of concomitant diabetes mellitus of the first or second type, glucose-lowering drugs or insulin are necessarily prescribed.
The duration, regimen of medication use and dosage are determined individually by the attending physician.
Treatment of the disease with medication
Hemorrhage in the eyeball can resolve on its own. This applies to cases where the disorder is not associated with chronic diseases. With minor bruising, the visual organs are not disturbed, and the ability to see does not change.
The principles of drug therapy for hemorrhage in the vitreous body or retina are aimed at eliminating inflammation. Vasoconstrictor drops help eliminate such symptoms. The most effective among them are:
- Visine.
- Taufon.
- Potassium iodide.
- Artificial tear.
In addition, vitamins are recommended that strengthen the walls of blood vessels in combination with hemostatic agents. The drugs are used in tablets or injections. Often prescribed:
- Dicynone;
- Vikasol;
- Aminocaproic acid;
- Ascorutin;
- Ascorbic acid.
These drugs help restore damaged vascular networks in the eye and reduce the permeability of the vascular walls. Thanks to this, oxygen supply and blood circulation improve, and hematomas formed in the eyeball quickly resolve.
Sometimes drug treatment is ineffective and surgery is required.
Surgery
Surgery is prescribed for massive hemorrhage in the retina, as well as for localized changes in the area of the macula. It is called vitrectomy and involves removing a blood clot that has formed that is preventing normal light perception. At the same time, altered, cloudy areas of the vitreous body are removed.
Despite radical surgical treatment for massive retinal hemorrhage, complete restoration of visual acuity cannot be achieved.
Features of hemorrhage into the main structures of the eye
In ophthalmology, hemorrhage is called damage to the eye vessels or capillaries. This is accompanied by the appearance of hemorrhagic spots in the eyeball. The intensity of redness is related to the location. This disorder has several varieties, which are distinguished depending on the area of the eye where the blood spreads.
Hemophthalmos
The process associated with the penetration of blood into the vitreous body is called hemophthalmos. The disease is manifested by the formation of a purple tubercle behind the lens. Patients experience flashes of light and dark spots in front of their eyes.
Depending on the severity of the pathology, hemophthalmos is divided into two types. These include:
- residual: vision deteriorates significantly, a complication appears - retinal detachment;
- total: blindness occurs.
Traditional methods of treatment
Traditional treatment methods involve the use of medicinal plants. It is recommended to take a lot of fruits containing sufficient amounts of vitamins. Among the medicinal plants, it is recommended to use chamomile and St. John's wort as an infusion internally.
Before using any folk remedies, you should consult your doctor.
Prevention
Retinal hemorrhage can be prevented. To do this, follow simple preventive recommendations, which include:
- exclusion of exposure to provoking factors;
- weight normalization;
- sufficient physical activity;
- rational nutrition with limitation of fatty, fried foods;
- giving up bad habits, including smoking and systematic drinking of alcohol;
- reducing the load on the organ of vision.
If a person knows that the strength of his vascular walls is reduced, then he needs to avoid sudden movements, turning his head, and bending. At the same time, for preventive purposes, it is recommended to take vitamin C and rutin, which strengthen the walls of blood vessels.
Hemorrhage in the retina can be dangerous for vision, so to prevent vision problems, you should consult a doctor at the first sign of changes.
Author of the article: Igor Mikhailovich Krivoguz, specialist for the website glazalik.ru Share your experience and opinion in the comments.