An accumulation of blood (a blood clot of varying sizes) in the white of the eye, or in its anterior chamber - hyphema. This is not just an aesthetic cosmetic defect. This pathological condition is extremely painful and can cause many vision-threatening complications.
The most common cause of the appearance of hyphema in the fibrous membrane of the eye is traumatic, from impact with a blunt object, without ruptures or penetrating wounds. But this does not mean that such injuries are less dangerous than penetrating injuries. Contusion can even cause complete blindness, as happens with grade 4 hyphema, when a blood clot fills the entire visible part of the sclera.
Definition of disease
The space bounded in front by the cornea and behind by the iris is called the anterior chamber of the eye, and in normal condition it is filled with intraocular moisture. However, if the vessels are damaged, blood penetrates the anterior chamber and fills it.
Since blood is heavier than the intraocular fluid, it always falls down, and if the hyphema is minor, it is observed in the form of a strip of blood along the lower edge of the iris. Sometimes the damage is so weak that it is not visible to the naked eye, and only an ophthalmologist, when examined using special instruments, can detect them.
This condition is called microhyphema, but it is no less dangerous than visible damage, since it is also fraught with its own complications.
What is hyphema
Hyphema is a dangerous condition in which hemorrhage occurs in the anterior chamber of the eye. It can be almost invisible to humans. In severe cases, blood fills most of the chamber (see photo). The red liquid gradually settles below and a clearly visible level of filling the space with blood is formed. Using this line, the ophthalmologist can judge the complexity of the patient’s condition and the stage of development of the hyphema:
- Microhyphema is detected only with the help of ophthalmological equipment, and the reason for examination is a person’s complaints of poor vision. In most cases, formations resolve on their own over time and do not require treatment.
- In the event that the chamber is 1/3 full, we are talking about the first degree, which responds well to treatment
- If the chamber space is filled to half, grade 2 is diagnosed, in which the treatment prognosis is favorable
- The third degree occurs when blood fills more than half of the chamber space, in this case there may be complications
- Grade 4 is characterized by a complex course in which the entire chamber is filled (“black eye”)
| If at the first and second stages the pathology can be treated with medications, then at the third stage surgical intervention may be necessary, and with total hyphema, only surgery solves the problem |
Hyphema is diagnosed more often in cats than in dogs. The main reason why this disease develops in animals is trauma (bruise, contusion, penetrating wound) of the eye. Especially in young active dogs and cats, due to fights, after being wounded by a claw, blood vessels inside the eye rupture and blood enters the anterior chamber.
In adult animals, hyphema can develop against the background of high blood pressure due to renal failure. In addition, uveitis (inflammation of the middle membrane of the eye, rich in blood vessels) or retinitis (inflammation of the iris) can provoke the disease.
Hyphema in an animal can be detected by careful examination - bloody clots will be observed in the intraocular fluid. However, only a veterinarian can make a correct diagnosis based on a set of studies (ophthalmoscopy, ultrasound, biomicroscopy, tonometry). In addition, to check the somatic condition of the pet, blood is given for analysis.
Since hyphema is a consequence of the underlying disease, therapy is aimed at treating a specific pathology. Therefore, in each individual case, a different set of drugs is used.
Types and classifications
There are several degrees of damage to blood vessels, determined by the amount of blood flowing into the anterior chamber:
- 1st degree – filling less than 1/3 of the volume;
- 2nd degree – filling from 1/3 to ½ of the anterior chamber;
- 3rd degree – more than half filled;
- Grade 4 – total hyphema (complete filling) or “black pupil”.
Degrees of hyphemas
As a rule, 3-5 days after the initial hemorrhage, a second hemorrhage may occur, which is often more abundant. Therefore, a distinction is made between primary and secondary hyphema.
Causes
There are several causes of the painful condition, however, undoubtedly, the primacy belongs to traumatic injuries:
- Injuries. Depending on the degree of damage, a distinction is made between penetrating injuries (complete damage to the eye membranes) and blunt injuries (non-penetrating). In penetrating trauma, rupture of blood vessels is the direct cause of hemorrhage. If the injury is blunt, then vascular rupture results from damage to the iris, ciliary body (the muscle that regulates the size and curvature of the lens) or the choroid (the choroid that provides nutrition to the retina);
- Eye surgeries. Hyphema can occur as a complication after abdominal or laser surgical interventions on the eyeball. The cause in this case may be damage to the vessels of the ciliary body or the iris. In most cases, the doctor will deal with this bleeding during surgery. However, up to several months after surgery, hyphemas may appear: with repeated bleeding of the same vessel or as a result of the growth of newly formed vessels at the site of the surgical incision;
- Eye diseases in which new blood vessels grow in the area of the iris. This phenomenon may be due to uncompensated diabetes mellitus, intraocular tumors, thrombosis of the central vein (in the retina), etc. Newly formed vessels are characterized by fragile walls that collapse at the slightest fluctuations in pressure (intraocular or arterial);
- Systemic diseases can cause bleeding disorders, resulting in bleeding for no apparent reason. These diseases include hemophilia, blood cancer, and anemia. Often, alcohol abuse has the same effect.
Since the main cause of hyphema is injury, the high-risk group includes young people 10-20 years old, when the threat of eye damage as a result of injury is highest.
Symptoms
Symptoms depend entirely on the degree of damage:
- With microhyphema, the manifestations of discomfort are insignificant, there is no decrease in vision, there is no hyperemia;
- At grade 1, “fog” appears in the eyes, and patients can independently diagnose a narrow strip of blood in the anterior chamber. If the hyphema is of traumatic origin, then pain and photophobia (photophobia) may appear;
- With grades 2 and 3, the symptoms increase: the blood level is clearly visible, a veil appears before the eyes, and vision is slightly reduced. Neurological symptoms are observed: headache and dizziness, “spots” before the eyes;
- With “black” hyphema, vision is, of course, absent, since the pupil is completely closed. Some patients retain light perception. Even after treatment, formed elements are detected in the cornea in microscopic quantities. They affect its color, which can reduce visual function.
“Black” hyphema
conclusions
Hyphema is, in most cases, a consequence of ocular trauma and should be treated as soon as possible after the injury. In this case, an inspection by a specialist must be carried out.
Non-traumatic hyphemas can occur in patients with severe blood diseases or cancer. The main symptom of eye damage is hemorrhage in the anterior chamber, but additional symptoms may be present. Often only they can help detect hyphema.
In any case, the disease is a dangerous pathology that threatens reduction and even loss of vision and should be treated only under the supervision of an ophthalmologist.
Read more about strabismus in newborns and whether conjunctivitis is transmitted.
Hyphema or hemorrhage in the eye, or more precisely in the anterior chamber, can be either completely harmless or lead to serious complications. Therefore, in case of injury (or bruise), you should visit an ophthalmologist.
Possible complications
The frequency and degree of complications are directly proportional to the degree of filling of the anterior chamber with blood, i.e., the strength of the lesion. With microhyphema, the risk of developing severe consequences is minimal. And, conversely, with a “black” pupil such complications are maximum.
The development of the following complications of hyphema is most often diagnosed:
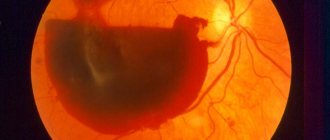
- Staining of the cornea with blood. Complete filling of the chamber invariably leads to the absorption of some amount of blood into the corneal layer, which causes a change in the color of the cornea and, consequently, a decrease in the quality of visual perception. Such a defect remains even after the blood is removed and disappears very slowly;
- Secondary glaucoma. It occurs due to an increase in IOP as a result of filling the anterior chamber with additional fluid. The greater the volume of bleeding, the higher the IOP and, therefore, the higher the risk of developing glaucoma and decreased vision.
Blood staining of the cornea is a complication of hyphema
Hyphema, even microscopic, must be treated adequately and promptly. Otherwise, decreased visual acuity is a guaranteed outcome.
Diagnostics
Even if there are no visible signs of eye damage after injury, the patient is recommended to undergo a preventive examination.
To determine the causes of hemorrhages in the anterior chamber and the nature of the damage, a number of studies are carried out:
- Visual examination and collection of medical history data allow us to draw a conclusion about possible etiological factors and determine the direction of further diagnosis;
- Visometry and tonometry are traditional methods that allow you to assess the functionality of the eyes and determine one of the main indicators of their health (IOP);
Testing visual acuity (visometry)
- Biomicroscopy is a method of examining internal structures using a slit lamp. Allows you to assess the extent and nature of damage;
- Computed tomography – examination is carried out in the most severe cases;
- Ultrasound of the eyeball - allows you to identify damage in areas that are inaccessible for examination by other methods;
- Blood test to determine the degree of clotting.
When identifying causes of non-traumatic origin, the diseases that served as the impetus for the development of hyphema are diagnosed.
How is the cause of hyphema diagnosed?
To determine exactly why the hemorrhage occurred, it is necessary to find out whether the patient has recently had an eye injury or eye surgery. If this does not happen, then doctors will conduct a series of studies to study the general condition of the body. So, it is necessary to donate blood for clotting. Using tonometry, the level of intraocular pressure is determined, and a coagulogram reveals the presence of hematological diseases. A general blood test provides information about the presence of common diseases.
Treatment
For minor injuries, outpatient treatment is performed. More extensive hemorrhages require constant medical supervision and hospital stay.
Indications for hospitalization may include:
- 3 or 4 degree hyphema;
- Presence of complicating factors (increased IOP);
- Age (young children);
- Patients with sickle cell anemia.
Despite the fact that the disease has been known for many centuries, treatment tactics remain the subject of debate. Therefore, all efforts of doctors are aimed at achieving the following goals:
- Ensuring patient comfort;
- Preventing re-bleeding;
- Prevention of complications.
Drug therapy
With conservative treatment, the first thing the doctor prescribes is bed rest, and the patient’s head should be elevated at an angle of at least 30˚, and the body position should only be on the back.
Medicinal tactics consist of using the following drugs:
- Hemostatic agents: Gemaza, Purolaza. Prescribed for ongoing bleeding and to prevent recurrence;
Hemostatic agent “Gemaza”
- Corticosteroids: Prednisolone, Hydrocortisone. The drugs have a strong anti-inflammatory effect, relieving swelling and irritation;
- Absorbable: Mannitol, Glycerol. Eliminate the consequences of hemorrhage and help restore the transparency of the cornea;
- Vascular strengtheners: Actovegin, Emoxipin. Strengthen vascular walls, preventing the threat of repeated hemorrhage;
- Weak analgesics: Acetaminophen. Preparations containing aspirin are contraindicated because they reduce blood clotting;
- Drops for pupil dilation: Atropine, Thymol, Acetazolamide. A temporary measure to prevent an increase in IOP, which can cause re-bleeding.
Atropine - drops with a relaxing effect
A shielding, non-pressure bandage is applied to the affected eye. It is mandatory to monitor (in a hospital setting) IOP several times a day to take action if there is a threat of recurrent hemorrhage.
Surgically
Surgery is a last resort and is prescribed when conservative therapy is ineffective or inappropriate.
The following conditions may be indications for surgical intervention:
- Formation of clots;
- Staining of the cornea with blood;
- No improvement with drug treatment within 5-10 days;
- Complete filling of the anterior chamber with blood;
- Ineffectiveness of conservative methods of reducing IOP.
Carrying out a surgical operation to wash the cornea of the eye from hyphema
The essence of the surgical operation comes down to washing the anterior chamber through 2 paracentesis located opposite each other. In addition, during surgery, a trabeculectomy or basal iridectomy can be performed to reduce intraocular pressure - restoring drainage function.
Folk remedies
Microhyphemas in most cases do not require drug treatment and resolve on their own, and in case of severe damage, when there is a large amount of blood in the anterior chamber, it is best to resort to surgical intervention.
When treatment is carried out using conservative methods, it would be useful to use folk remedies in addition to medications:
- Pour 0.5 liters of water 3 tbsp. l. chicory powder, boil and leave. Take 100 ml of the filtered drink three times a day, and also rinse your eyes with the infusion;
- Make a 10% alcohol tincture from arnica flowers, leave in a place protected from sunlight for a week, filter and take 30 drops, first diluted in water or milk, shortly before meals three times a day;
- Make a water infusion from the same arnica in the proportion of 10 g per 200 ml of water. Pour boiling water over and leave for 15 minutes. Use the filtered infusion one tablespoon at a time, also diluted;
- Use strong black tea brew for rinsing and lotions;
- Boil a small amount of urine in a copper basin with an equal amount of honey. Use the resulting solution for instillation into the sore eye;
- Place a small piece of raw chilled meat on the sore eye. Change the compress as it warms up.
Treatment of even microhyphema must be carried out under the supervision of a doctor, and the use of folk remedies must be consistent with him.
Prevention, prognosis and risks of complete loss of vision
The anterior chamber is of great importance for the formation of the immune function of the eye, and any damage to it can provoke a decrease in resistance to the effects of adverse environmental factors, therefore it is important to ensure timely prevention of hyphema and other types of subconjunctival and intraconjunctival hemorrhages:
- When engaging in outdoor sports, it is necessary to follow safety rules to minimize the risk of damage to the eyes and other particularly sensitive organs.
- Children from an early age need to be explained the rules of playing together: you cannot wave your arms too much, push your comrades, touch their faces with foreign objects (pens, pencils) and throw sand. Sharp objects should only be handled under adult supervision.
- Patients with a history of diabetes mellitus, severe heart and vascular diseases (especially malignant hypertension) should visit an ophthalmologist at least 2 times a year.
- Patients with oncological diseases of the organs of vision should undergo a thorough examination with measurement of visual acuity and monitoring of hemodynamic parameters every 3-4 months.
When working with harmful substances and vapors (diamond dust, sawdust, paints and varnishes, etc.), it is necessary to use protective equipment, including special safety glasses.
Forecast
Complete loss of vision with grade 3-4 hyphema is possible with untimely or incomplete treatment, as well as non-compliance with the rules of postoperative care and rehabilitation. For grades 1 and 2 hemorrhage, treatment in most cases gives consistently positive results, and visual function is restored in full.
Hyphema is a fairly common ophthalmological disease that requires careful medical supervision due to the high risk of relapse in the acute period. Conservative methods are used to treat uncomplicated hyphemas: drug therapy and physiotherapy. In severe cases, surgery is indicated. The prognosis for timely seeking help is favorable: 75% of patients completely restore visual function and return to normal life.