Throughout life, a person may encounter a foreign object entering the eye.
This causes injury. If a speck or speck of dust gets in, there is no risk of complications.
These items are easily removed. More complex injuries damage the corneal epithelium. Severe injuries cause the development of erosion. This consequence can lead to retinal detachment. The patient faces the risk of vision loss. Therefore, timely consultation with a doctor is very important.
Structure of the cornea
The cornea protects the internal structures of the eye from all kinds of influences (chemical, mechanical and temperature) of the external environment. It is the main optical refractive lens.
The stratum corneum consists of 5 layers:
- Epithelial. The most superficial layer performs a protective function. Recovers quite well from damage. Consists of 5 – 6 cell layers.
- Bowman's shell. Consists of dense fabric. It is a supporting layer that supports the outer epithelial layer.
- Stroma. Has a special cellular composition. Consists of keratocytes. Occupies most of the thickness of the cornea. It is its thickest part. Provides transparency of the cornea.
- Descemet's membrane. It is the framework of the cornea. The strongest and toughest of the layers.
- Endothelium. Inner layer of the cornea. It consists of one row of cells that perform the function of a pump in the process of exchanging nutrients between the cornea and the intraocular fluid of the anterior chamber of the eye.
Rice. 2. Structure of the cornea.
Classification
Corneal erosions are divided into two large groups: infectious and non-infectious. The causes of infectious erosions are:
- Bacterial conjunctivitis and blepharitis (streptococci, staphylococci, Pseudomonas aeruginosa).
- Herpetic keratitis.
- Adenoviral and epidemic keratoconjunctivitis.
- Mycotic keratitis.
- Chlamydial conjunctivitis.
The causes of non-infectious erosions are:
- Keratoconjunctivitis sicca (dry eye syndrome).
- Mechanical injuries (including surgical interventions).
- Toxic damage (drugs, chemicals, molluscum contagiosum, staphylococcal blepharitis).
- Allergies (spring catarrh, drug keratitis).
- Internal pathology (autoimmune and endocrine diseases, hormonal disorders).
- Seborrhea of the eyelid margins.
Ulcerative defects, depending on the depth of the lesion, are divided into:
- Superficial.
- Deep.
- Perforated.
According to the flow of erosion, they are divided into:
- Acute (single reaction).
- Chronic (persistent recurrent).
To size:
- Small (spot).
- Large ones.
By localization:
- Upper zone.
- Lower zones.
- Central zone.
- Middle open area.
- Peripheral zone.
- Diffuse location.
Chronic erosions are divided into two large groups:
- Chronic persistent (constantly present in the patient, despite the treatment). This includes toxic, trophic and mycotic erosions.
- Chronic recurrent erosions (as a result of treatment, epithelization of the defect occurs, but after some time a relapse occurs again). These include herpetic, post-traumatic, post-infectious and dystrophic erosions.
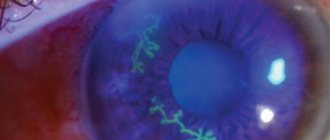
Rice. 3. The photo shows recurrent erosion.
Types and classification
The disease is divided into several forms according to different characteristics:
- Depending on the size, erosion is classified into local and large-scale;
- By location. The pathology may be in the upper or lower part of the membrane;
- By the volume of damage (over all surfaces or affecting one layer);
- According to the duration of the disease (one-time or recurrent).
It is important to distinguish erosion from ulceration. In the first case, there is damage to the epithelium, which can recover on its own. With proper treatment, it does not leave scars and does not impair visual acuity. With an ulcer, recovery does not occur; after the “sore” heals, seals remain on the outer shell.
Corneal erosion is also divided into two forms depending on the cause of the disease.
Recurrent
With such a disease, unpleasant symptoms return over and over again, despite the course of therapy. There are two types of pathology: diffuse (the damage affects the main part of the mucosa) and local (the damage develops in a specific area).
A recurrent anomaly occurs for the following reasons:
- When the conjunctiva is injured, the basal cells responsible for the process of tissue regeneration are affected. As a result of pathology of the cornea, defective cells are formed on its surface, they shrink and expose the lower layers;
- Pathological processes are activated due to inflammation occurring on the outer shell.
The main symptoms of the disease: pain, burning, increased lacrimation.
| The main goal of therapy is to restore the integrity of the basal layer. For this, doctors prescribe fortified ointments that normalize metabolism. Antibacterial medications are used to prevent the cornea from drying out. |
Traumatic erosion
In most cases, the integrity of the membrane is compromised as a result of mechanical impact on the organ of vision. The smooth epithelial layer is damaged when a foreign object penetrates the eye or when contact lenses are used incorrectly. Pathology can also manifest itself due to severe wounds affecting the mucous membrane.
Traumatic erosion is diagnosed when the eye is burned by chemicals or toxins. The disease appears as a result of exposure to high temperatures on the visual apparatus. The integrity of the cornea can be damaged by regular friction of the cilia on the mucous membrane as a result of their improper growth or inversion of the eyelids.
The main symptoms of the disease:
- Painful sensations;
- Photophobia;
- Redness of the conjunctiva;
- Increased lacrimation;
- Feeling of the presence of a foreign object;
- Damage to the central part of the cornea leads to a decrease in visual acuity.
Eye drops and antibacterial medications are used to treat the disease. Return to contents
Symptoms of erosive keratitis
The symptoms of corneal erosion are so specific that a preliminary diagnosis by a doctor is established already at the stage of interviewing the patient.
- Acute, often unbearable pain in one eye is the first and most significant sign of the disease. The pain is similar to a foreign body getting into the eye.
- Reactive lacrimation.
- Swelling of the eyelids.
- Blepharospasm (occurs in 80% of cases). Patients are unable to open their eyes and blink with difficulty.
- Photophobia.
- Discharge from the eyes.
- Redness of the eye from the first day of the disease.
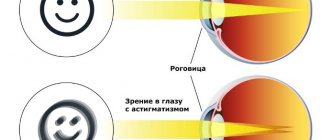
- When erosion is localized in the central part of the cornea, a decrease in visual acuity is observed.
Rice. 4. A slit lamp is used to perform biomicroscopy of the eye.
Symptoms
First of all, pain appears. It occurs due to irritation of nerve endings. The pain may worsen when blinking, especially if there is a foreign body in the eye. After this, uncontrollable lacrimation may occur. The manifestation of symptoms depends on the degree of damage to the eye. If infection is repeated, purulent discharge may appear. A person may suffer from sensitivity to light rays.
A large lesion is accompanied by severe redness of the conjunctiva. There is discomfort, a feeling of sand in the eye, and a strong burning sensation. Such symptoms confirm the presence of an inflammatory process. If erosion is localized in the center, then in most cases visual acuity decreases.
Photo
Traumatic erosion looks like this:
Diagnostics
Erosive corneal damage requires the use of detailed imaging. First, the organs of vision are examined visually. Next, a special optical device is used - a slit lamp, designed to perform biomicroscopy of the eye. With its help, it is possible to determine the size, localization and degree of penetration of erosion into the cornea, detect foreign objects in the conjunctival sac, determine the presence of exudate and tumor changes in the mucous membranes, check the direction of eyelash growth, and examine the inner surface of the eyelids.
Corneal erosions are easily detected by staining the epithelium with a fluorescein solution. The damaged areas turn green.
Additional examination methods include diaphanoscopy, ophthalmoscopy, ultrasound diagnostics, bacteriological and cytological research methods.
If the patient wears lenses, they should be checked under a microscope for damage - cracks and roughness that can damage the cornea.
Rice. 5. The photo shows corneal erosion. Fluorescein staining gives the defect a green color.
Prevention
It is worth noting that prevention of such pathologies is always necessary. Following simple rules will help to significantly reduce the risk of developing such diseases. Recommended preventative measures:
- use of sunglasses;
- protection from injury;
- When working with hazardous substances, be sure to wear safety glasses;
- be examined by an ophthalmologist 1-2 times a year;
- consult a doctor promptly if a foreign object gets into the eye;
- adhere to hygiene rules;
- maintain a healthy lifestyle;
- take the necessary vitamins daily for visual health;
- avoid excessive visual stress;
- get adequate sleep.
If a foreign object gets into the eye, first aid must be provided immediately. The affected eye is washed with purified water. Then you need to add drops. It is strictly forbidden to rub your eyes or try to reach the object yourself. In this way, you can further injure the mucous membrane.
After providing first aid, you should consult a doctor. The main rule of prevention is timely treatment. If the patient contacted a specialist in time and began undergoing therapy, the result will be successful. This is especially important in the development of severe diseases.
Complications
Untimely and inadequate treatment of erosions often leads to the development of numerous complications:
- Cloudiness of the cornea.
- Formation of scar tissue, which leads to decreased visual acuity.
- The development of necrosis of the corneal stroma - an ulcerative defect with the subsequent development of many complications, including loss of vision.
- The formation of additional vessels during healing (neovascularization). Neovascularization helps accelerate recovery processes and improve the trophism of corneal tissue. But, on the other hand, the newly formed vessels gradually become empty, which leads to a decrease in the transparency of the cornea. The complication can be eliminated only with the use of surgical treatment methods.
Rice. 6 and 7. The photo on the left shows superficial vascularization of the cornea.
Treatment of corneal erosions
With timely and adequate treatment, erosions disappear within 2–4 weeks without scarring. Main directions of the treatment process:
- Antibacterial treatment.
- Anti-inflammatory.
- Decongestant.
- Reparative.
- Protective.
- Replacement therapy.
The duration of antibacterial therapy is 5-7 days. Antibacterial drugs are used in the form of drops and ointments (Levomycetin, Gentamicin (Tobramycin, Tobrex), Ciprofloxacin (Tsipromed, Uniflox, Vigamox). Drops are instilled 3-4 times a day, ointments are applied at night.
After discontinuation of the antibiotic, a transition to the use of antiseptics (Vitabact) is indicated, since the defect may still persist by this time. Antiseptics can be used for a long time - up to 3 - 4 months.
Among anti-inflammatory drugs, hormonal drugs (Oftan, dexamethasone, etc.) are used locally in short courses. When they are contraindicated, non-steroidal anti-inflammatory drugs (Diclof, Indocollir, Acular, Nevanac) are used. Their use is allowed for 3 or more months.
With the development of allergic keratoconjunctivitis, drugs such as Spersallerg, Cromohexal, Prenacid, etc. are used.
Arutimol (a blocker of β1- and β2-adrenergic receptors) and Hiloparin-Komod (contains heparin) have an anti-edematous effect.
For defects in the stratum corneum, Taurine eye drops are prescribed and healing ointments are used to stimulate epithelization processes. The drug Korneregel, created specifically for the treatment of eyes, has good reparative properties, and to a lesser extent, Khilozar-Komod and Balarpan. The processes of epithelization of the cornea are improved by a solution of Quinine hydrochloride, Solcoseryl, Emoxipin, Taufon, Actovegin, Lipoflavon, Balarpan. In case of chronic keratitis with long-term non-healing erosion, the use of drugs containing hyaluronic acid (Vizmed monodoses, Oksial, Hilabak, Hilomax-Komod) is indicated. The preservatives present in them have antiseptic properties.
For chronic erosions, tear replacement therapy is used for a year or more - up to 4 - 5 years. After epithelization of erosion, the use of drugs in gel form (Vidisik, Oftagel) is indicated.
Protective agents include Korneregel, Vismed-gel, Vit-A, Lacrisify, etc. The drugs are applied overnight until the erosion is completely healed; Lacrisify is used in the form of drops. It is also recommended to wear contact lenses (usually daily). Persons who wear contact lenses constantly are recommended to instill antiseptics (Vitabac, etc.). The drugs prevent the accumulation of microflora under the lenses.
Rice. 8. Cloudiness of the cornea (thorn).
Treatment
Most patients are prescribed medication. Initially, you should take drops that promote mucosal regeneration. Among such drugs are Systane and Oksial. In addition to drops, you can use ointments that have the same effect.
Additionally, you will need to take antibacterial drugs. Visoptic and Taufon drops will help restore tear function.
Drug therapy consists of several stages. The treatment is simple. If the patient does not consult a doctor in time, he may face the development of complications. The pathology can become recurrent. In this case, the treatment will take longer.
Traumatic corneal erosion
Violation of the integrity of the epithelium of the cornea due to injury is observed when pieces of metal, plant husks get into the eye, injury from a nail, airbags, rubbing, injury, ignoring the requirements when wearing contact lenses, etc. If eyelashes grow incorrectly, when there is constant injury to the cornea, it may occur macroerosion, when infected, turns into a corneal ulcer, threatening vision loss.
The cornea is injured as a result of exposure to chemicals, high temperature and ultraviolet radiation. Erosions are formed in diseases that occur with a decrease in the intensity of metabolic processes, when different layers of the cornea die off as a result of degenerative processes. Recurrent erosions occur with chronic keratitis.
When the cornea swells, fluid-filled blisters form in its thickness, which, when ruptured, form large areas with a disturbed structure.
Symptoms
With traumatic erosions, corneal syndrome develops:
- At the moment of rupture of the epithelial layer, sudden lacrimation is recorded and then, as the defect grows, its increase is noted.
- The occurrence of damage is always accompanied by pain, as numerous nerve endings located in the corneal tissues are exposed. Acute pain gradually turns into a sensation of a foreign body in the eye, often accompanied by aching pain, especially under the influence of light.
- When erosions are localized in the central zone, a decrease in visual acuity is observed. Clarity of perception is impaired in the presence of extensive foci of damage localized along the periphery.
- When the cornea is injured, reflex blepharospasm develops (involuntary closure of the eyelid).
Healing of corneal erosions occurs unevenly. The tree-like configuration of the healing areas is similar in appearance to herpetic keratitis
Diagnostics
When examining the organ of vision using a slit lamp, abrasions of the conjunctiva and subconjunctival hemorrhages, stromal edema, folds of Descemet's membrane, and the presence of cellular elements, including blood, in the humor of the anterior chamber are revealed. In case of severe traumatic erosions, it is possible to detect blood clots in the white of the eye.
Erosions are easily identified by staining the cornea by instilling a 1% fluoroscein solution. The light green colored area of damage can be easily visualized and measured.
Further, if necessary, the examination should be continued:
- Inspect the unaffected part of the epithelium for disruption of its normal attachment to the underlying basement membrane. In such cases, erosion can appear at the slightest injury.
- Inspect the cornea for the presence of keratitis, followed by taking a smear for culture for bacteriological examination.
- If linear vertical erosions are detected, the conjunctiva of the upper eyelid should be carefully examined for the presence of a foreign body.
Rice. 9. The photo shows corneal erosion. Fluorescein staining gives the defect a green color.
Treatment of traumatic erosion
At the first stage of treatment, after instillation of a local anesthetic into the eye, the foreign body is removed from the surface of the cornea and exfoliated epithelium. Partially exfoliated epithelium does not fit back, since when blinking it is re-displaced and causes additional discomfort to the patient, and also slows down recovery.
Further, broad-spectrum antibiotics or sulfonamide drugs are prescribed for prophylactic purposes. The course of treatment is 3 – 5 days. It is recommended to prescribe ointments with antibiotics (Erythromycin, Bacitracin, etc.).
Many ophalmologists believe that the use of dressings for erosions does not affect the rate of healing of the defect and increases the risk of complications. It is strictly forbidden to use bandages on people who wear contact lenses or when organic foreign bodies get into the eye.
Erosions epithelialize quickly, so the pain syndrome does not last long. For pain of moderate intensity, solutions of Dicaine or Inocaine are prescribed; for severe pain, narcotic painkillers are prescribed. The constant use of local anesthetics is unacceptable, as this leads to disruption of the healing process and thinning of the stratum corneum.
For defects in the stratum corneum, Taurine is used to stimulate epithelization processes, and healing ointments are used. The processes of epithelization of the cornea are improved by a solution of Quinine hydrochloride, Solcoseryl, Emoxipin, Taufon, Actovegin, Korneregel, Lipoflavon, Balarpan.
Complications of corneal erosion
In the absence or irregular treatment, in some cases, post-traumatic keratitis develops, followed by the development of a creeping corneal ulcer.
There have been cases of the development of repeated corneal erosions in the absence of trauma, which is associated with disruption of the normal adhesion of the epithelium to the underlying basement membrane and stroma of the cornea.
Rice. 10. The photo shows corneal erosion of a traumatic nature.
Causes
Most often, the development of pathology is caused by the following factors:
- Penetration of a foreign object into the conjunctiva;
- Mechanical damage to the organ of vision. The integrity of the outer shell can be damaged by tree branches, pet claws, etc.;
- Chemical burn;
- Damage to the cornea as a result of improper use of contact lenses;
- Exposure to high temperatures;
- Effect of ultraviolet radiation;
- Dystrophic pathologies of the cornea;
- Surgical intervention on the visual apparatus;
- Neoplasms on the inner surface of the eyelid;
- Violation of eyelash growth. The anomaly develops against the background of demodicosis;
- Abnormal eye structure.
As you can see, almost all the reasons for the development of erosion indicate that the person himself is to blame for the appearance of the disease. Following basic safety rules and timely contact with an ophthalmologist will help you avoid problems with the cornea. Return to contents
Corneal erosions in keratoconjunctivitis sicca
Keratoconjunctivitis sicca (dry eye syndrome) occurs due to a marked decrease in tear production and disruption of the stability of the tear film. The disease is more often registered in women and people over 70 years of age. After adenoviral conjunctivitis, the syndrome is registered in 80% of cases, herpetic conjunctivitis - in 78% of cases, chlamydial conjunctivitis - in 52% of cases, bacterial blepharoconjunctivitis - in 87% of cases. The development of dry keratoconjunctivitis is often recorded after photorefractive surgery and keratoplasty.
Burning, pain in the eye, dryness, foreign body sensation, photophobia, poor tolerance to smoke and wind, discomfort after instilling eye drops are the main symptoms of the disease.
Upon examination, dilation of the conjunctival vessels is revealed, there is a tendency to the formation of folds of the mucous membrane, the surface of the cornea is uneven, and flocculent inclusions are noted in the tear fluid.
In dry eye syndrome, microerosions are the most common, less common are large erosions, filamentous keratitis, epithelial keratopathy and corneal ulcers.
In addition to the characteristic complaints of patients and biomicroscopic examination data, special tests are used to diagnose the disease: Nohr's test (determining the stability of the tear film), Schirmer's test (determining the level of tear fluid production), identifying dead cells of the epithelial cover of the conjunctiva and cornea using Bengal staining solution -pink.
Main directions in treatment:
- Tear replacement therapy (Lacrisify, Vidisik gel composition, etc.).
- For allergy symptoms, Prenacid, Octilia, Cromohexal drops are used.
- For defects in the stratum corneum, Taurine is used to stimulate epithelization processes, and healing ointments are used. The processes of epithelization of the cornea are improved by a solution of Quinine hydrochloride, Solcoseryl, Emoxipin, Taufon, Actovegin, Korneregel, Lipoflavon, Balarpan.
Rice. 11 and 12. The photo shows keratoconjunctivitis sicca (dry eye syndrome).
Filamentous keratitis
Filamentous keratitis develops as a result of many pathological processes against the background of hypofunction of the lacrimal glands and drying of the corneal epithelium. The disease is a severe corneal-conjunctival xerosis.
Office workers, women over 45 years of age and elderly people are more likely to get sick.
Patients note dry eyes and even the absence of tears when crying, cutting pain, photophobia, the sensation of a foreign body in the eye and involuntary closing of the eyelids. A filamentous, viscous secretion forms in the eye. The degree of eye moisture is determined by the Schirmer test.
In severe cases, hyperkeratosis develops, sometimes covering the entire area of the cornea. Vision deterioration is gradually observed. Recurrent ulcers and erosions may occur. Chronic inflammation and degenerative changes in the cornea lead to a decrease in its transparency, and less often to softening and perforation. In some cases, prolapse of the membranes of the eyeball is noted.
Rice. 13. The photo shows filamentous keratitis.
Corneal erosions due to allergies
The causes of allergic keratitis are endo- and exoallergens. Among the endogenous allergens, there are bacterial allergens formed during helminthic infestation and tuberculosis. Exogenous allergens include medications, food, pollen, household chemicals, animal hair, cosmetics, etc.
In allergic keratitis, pronounced conjunctival-pericorneal injection is noted, corneal edema and subepithelial infiltration are noted. Infiltrates are located at different depths and in different parts of the cornea, have different sizes and shapes. Superficial infiltrates disappear without a trace during treatment, deep infiltrates often heal with the formation of scar tissue, often leaving areas of opacification of varying degrees of severity. Erosion and ulceration of the corneal tissue often appear.
Corneal erosion due to drug-induced conjunctivitis
The cause of erosion can be drug-induced conjunctivitis. Mucosal defects occur both acutely (after the first use of the drug) and in cases of chronic disease (90% of cases) as a result of long-term use of the drug. An allergic reaction develops both to the main component of the drug and to the preservative.
In acute allergic inflammation, the main symptoms are redness, lacrimation, swelling of the eyelids and conjunctiva, sometimes hemorrhages, in chronic - itching of the eyelids, moderate discharge, hyperemia, formation of follicles.
Drug-induced conjunctivitis in some cases causes the formation of erosions: more often microerosions, less often macroerosions. Mucosal defects most often occur in the lower pole of the cornea.
With the development of allergic keratoconjunctivitis, drugs such as Spersallerg, Cromohexal, Prenacid, etc. are used topically. Antihistamines and non-steroidal anti-inflammatory drugs are safe and effective.
For defects in the stratum corneum, Korneregel, Lacrisify, etc. are used to stimulate epithelization processes.
Rice. 14 and 15. The cause of erosions in some cases can be drug-induced conjunctivitis.
Corneal erosion in spring catarrh
The cause of the development of vernal keratoconjunctivitis is airborne allergens. The disease usually develops in the spring and is a hypersensitivity reaction - an allergy. In 9.7% of patients with spring catarrh, erosions and ulcers appear on the cornea. Often the disease takes a persistent chronic course, debilitating the patient. Usually, people (usually men) from 3 to 25 years of age are affected. Children aged 3–7 years often get sick. After puberty, the disease usually goes away, but sometimes there is a transition to adulthood and then proceeds as atopic keratoconjunctivitis.
The main symptoms of spring catarrh are itching, photophobia and redness. On examination, inflammation of the conjunctiva lining the inner part of the eyelid and the outer shell of the eyeball (sclera) is noted. On the upper eyelid, small flattened or large papillae appear in the form of tubercles or bumps that deform the eyelid (conjunctival form). Less commonly, papillary growths are found along the limbus (limbal form). Sometimes a mixed form is registered. Discharge from the eye is mucous and viscous.
Damage to the cornea is always observed in spring catarrh. Microerosions are recorded more often, macroerosions are less often recorded. Deformations of the mucous membrane affect the areas of the upper and middle parts of the cornea. In some cases, ulcers and hyperkeratosis appear.
For mild cases of the disease, the antiallergic drug Cromohexal is prescribed, for severe cases - Spersallerg. Antiallergic drugs are combined with corticosteroids (Prenacid, Dexamethasone, etc.). Reparative agents must be used. Additionally, systemic antihistamines are prescribed.
Trophic and dystrophic erosions
With eyelid failure, trigeminal neuralgia and severe edema, trophic erosions of the cornea often develop; against the background of thyroiditis and rheumatoid arthritis, dystrophic erosions occur. In the first case, special attention during treatment is paid to reparative and protective agents; in the second case, to the treatment of the underlying disease and also to reparative and protective agents. Antibacterial agents are prescribed in short courses every 3 months.
The cause of point erosions is keratitis of various origins. The disease is characterized by the appearance of scattered pinpoint defects in areas of the epithelial layer of the cornea. A full examination is required to identify the root cause of the disease. Treatment is etiotropic, pathogenetic and symptomatic. Dry eye syndrome requires tear replacement therapy.
Rice. 16. The photo shows multiple microerosions, covering the open area of the cornea (painted with pink bengal).
Toxic corneal erosions
The development of toxic keratitis is based on the impact of toxins of various natures on the corneal tissue - drugs, chemicals, bacterial and viral toxins.
Corneal erosions with staphylococcal blepharitis
The development of erosions in staphylococcal blepharitis is based on the toxic effect of infection. With the disease, microerosions and erosions of medium size are formed, located diffusely or in the upper part of the cornea. If eyelashes grow incorrectly, when there is constant injury to the cornea, macroerosion may occur, which, if infected, turns into a corneal ulcer, threatening vision loss. Antibacterial drugs, healing and protective agents are used in treatment. Particular attention is paid to eyelid hygiene.
Corneal erosion due to molluscum contagiosum
Molluscum contagiosum viruses (a group of poxyviruses) have a toxic effect on the cornea, which causes the development of chronic follicular conjunctivitis and epithelial keratitis.
The disease is manifested by the formation of single or multiple nodules on the skin of the eyelids. They have a hemispherical shape, are slightly pinker in color than the skin, and range in size from 1 mm to 1 cm in diameter. There is a depression in the center. When infused, a curd-like plug is released from the nodule.
Corneal erosions in molluscum contagiosum are localized over the entire surface of the cornea or in its upper part. They are small and often combined with punctate epithelial keratopathy.
When treating nodules, electrocoagulation is used; for large nodules, curettage is used. After their disappearance, the phenomena of corneal erosion and conjunctivitis disappear.
Rice. 17. Molluscum contagiosum on the eyelids.
Rice. 18. The photo shows toxic erosion.
Erosion in infectious keratitis
Quite often, erosions occur against the background of keratitis of an infectious nature.
Erosion in mycotic lesions of the eye
The cause of the development of mycotic erosions is mold, radiant and yeast fungi. They often complicate the course of traumatic keratitis. Risk factors for the development of infection are long-term instillation of antibiotics and corticosteroids, as well as chronic inflammation of the conjunctiva, lacrimal sac and tubules.
Characteristics of fungal infection are severe pain, redness of the eye and severe subjective symptoms of keratitis: blapharospasm, photophobia and lacrimation.
With mycotic keratitis, ulcerations of both the superficial and deep layers of the cornea, subepithelial edema are observed, followed by rupture of the epithelial layer and the addition of a secondary infection.
Complications include perforation of the cornea, involvement of the choroid in the inflammatory process, and development of a cataract.
Diagnosis of mycotic keratitis is difficult, which is why treatment is often carried out incorrectly. The lesion on biomicroscopy has a yellowish or white color, the boundaries are clear, the surface is lumpy and loose. Fungal mycelium is detected in the contents of the ulcerative defect.
Systemic antifungal treatment (ketoconazole, levorin, nystatin). Nonsteroidal anti-inflammatory and antifungal drugs are prescribed locally. To restore vision, lamellar keratoplasty is performed. To prevent secondary infection, antibiotics and sulfonamide drugs are prescribed. Cryotherapy and diathermocoagulation are indicated.
Rice. 19 and 20. The photo shows fungal keratitis.
Symptoms (signs)
Clinical picture
• Creeping cornea ulcer (a rogue ulcer of a bacterial etiology is caused by a pneumococcus of frenkel -vegetables, a diplobacilla of a Moraks - Aqsenfeld, staphylococcus, streptococcus, a pseudoscan) •• severe pain of a cutting, lacrimation, pronounced blepromation, and chemosis, mixed injection, mixed injection. •• yellowish - gray infiltrate of the cornea, quickly disintegrating with the formation of an ulcer with two edges - regressive and progressive (undermined, loosened and surrounded by a rim of purulent infiltrate). The ulcer quickly increases in size due to the progressive edge, gradually covering most of the cornea. From the limbus side, vessels grow into the ulcer (pannus) •• Iritis, iridocyclitis are often associated, and endophthalmitis may develop.
• Tuberculous corneal ulcer •• The presence of a focus of tuberculosis infection in the body •• Along with ulcers of a regular round shape, there are grayish-yellow infiltrates, surrounded by branched vessels (the infiltrate is located in a basket of vessels - lycten), progressing with the formation of ulcerative defects •• The course is long, with prolonged remissions, rough corneal scars form at the site of the ulcers.
• Herpetic ulceration of the cornea is characteristic of tree-like and ulcerative keratitis - tree-shaped ulcers are formed in place of tree-like infiltrates.
• Ulcerations of the cornea caused by hypo- and avitaminosis •• With vitamin A deficiency, keratomalacia develops - against the background of bilateral opacification of the cornea (“milky” cornea), ulcers appear that are not accompanied by pain. Xerotic dry plaques form on the conjunctiva of the sclera •• Vitamin B2 deficiency - vascularization of the cornea, dystrophic changes in the epithelium, and ulcerative defects occur. Usually the course is long and relatively benign.