An acute attack of glaucoma is observed due to a sharp increase in pressure, which often leads to irreversible blindness in the absence of medical attention. As a rule, an attack of a sharp excessive increase in pressure inside the eye develops in patients suffering from angle-closure glaucoma. In pathology, the drainage system of the eye is completely blocked, so the intraocular fluid accumulates and puts excessive pressure on the tissues of the eye. With age, the risk of a glaucomatous attack increases, so it is important for patients over 60 years of age to undergo regular follow-up examinations to ensure constant monitoring of IOP levels.
Symptoms of an acute attack of glaucoma
An acute attack of glaucoma can be provoked by various stress factors (physical or nervous fatigue, hypothermia), prolonged work in a position with a tilted head.
Some time before the attack, the patient may experience a number of symptoms that are harbingers of a sudden increase in intraocular pressure. Thus, the patient may experience rainbow circles around light sources or transient blurred vision. In some cases, a sudden increase in intraocular pressure occurs without any previous symptoms.
Most often, the attack occurs at night, between 3 and 4 o'clock. The patient wakes up from a severe throbbing headache in the eye area and the corresponding half of the head, which may be accompanied by symptoms such as heart pain, nausea, vomiting, severe weakness, and abdominal pain. These symptoms include dizziness, blurred vision, glare and rainbow circles before the eyes. In some cases, during an acute attack of glaucoma, the patient develops uncontrollable vomiting, severe pain in the heart, accompanied by changes in the electrocardiogram. Such symptoms are often misinterpreted by the patient and are regarded as a heart attack or migraine attack, which delays the provision of appropriate ophthalmological care to the patient.
What can cause a glaucomatous attack
The greatest danger of glaucoma is that there are often cases when the disease develops asymptomatically, so an attack can occur unexpectedly without obvious reasons. Despite the fact that all the reasons for the development of an acute attack have not been studied, there are the most powerful factors:
- increased pressure levels and blockage of the drainage channel as a result of eye injury;
- a consequence of a stressful situation and anxiety;
- prolonged eye strain and maintaining a head position tilted to the side;
- increased blood pressure;
- excessive alcohol consumption;
- uncontrolled single intake of large volumes of liquid;
- severe physical stress.
Our doctors who will preserve your vision with glaucoma:
Molchanova Anna Aleksandrovna
Ophthalmologist, deals with the diagnosis of the disease and postoperative care of patients.
Estrin Leonid Grigorievich Laser surgeon, the main focus of his work is modern laser methods for the treatment of glaucoma.
On palpation, the affected eye is sharply hardened (“stone”), extremely sensitive to pressure (accompanied by severe pain). When measuring the level of intraocular pressure, indicators can reach 70 – 100 mmHg. Art. With ophthalmoscopy, visualization of the fundus of the eye is difficult; a swollen, full-blooded optic disc may be visible against the background of a pale retina and full-blooded dilated veins.
Diagnostics
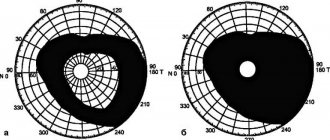
The diagnostic program usually includes a survey and examination of the patient, measurement of visual acuity and fields, refractometry, tonometry, microscopy, gonioscopy, and ophthalmoscopy. The study usually reveals a decrease in acuity and a narrowing of the visual field in the affected eye.
During microscopy, you can see redness and swelling of the conjunctiva, clouding of the cornea, swelling of the corneal epithelium, the presence of cloudy inclusions in the aqueous humor, and dilation of the vessels of the iris. Sometimes it is possible to detect precipitates on the inner surface of the cornea. During an acute attack of glaucoma, the pupil dilates greatly, becomes asymmetrical, greenish, does not react to light and does not accommodate.
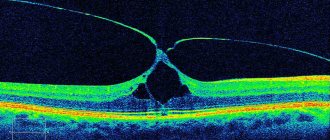
Gonioscopy helps to detect a narrowed angle of the anterior chamber. Due to clouding of the transparent media of the eye, ophthalmoscopy is not always informative. If the examination is successful, swelling and redness of the optic nerve head can be seen in the fundus.
The patient also undergoes ultrasound biometry (b-scan), Forbes compression test, daily tonometry, and topography. A general blood and urine test, RW and determination of blood glucose levels are mandatory. If necessary, a consultation with a therapist and/or endocrinologist is scheduled. Only after a full examination is the patient given a final diagnosis of glaucoma.
Causes and possible risk factors
The occurrence of an attack is associated with an imbalance between the outflow and inflow of fluid in the eye. Its production is carried out by the components of the ciliary body, and the anterior chamber of the eyes, or rather its angle, is responsible for the outflow. When an unexpected obstacle appears in this corner, fluid outflow is disrupted. In this case, the fluid “passes” from the posterior chamber of the eye to the anterior one, exerting strong pressure on the area of the eyeball.
The causes of an attack of increased intraocular pressure lie in the following factors:
- Prolonged state of stress;
- Frequent, unhealthy physical activity;
- Severe cooling or overheating;
- Drinking a large amount of liquid at one time;
- Staying in a static position for a long time with the head tilted forward;
- Adverse reaction to Atropine, which is part of the medication.
Patients who already have visual impairments and documented eye development abnormalities are most susceptible to developing an attack:
- Large or thickened lens;
- Increased size of the ciliary body;
- Thinning cornea;
- Small eyeball;
- Insufficient depth of the anterior chamber.
It should also be noted that high pressure inside the eye is provoked by the following circumstances:
- Presence of farsightedness since childhood;
- Pathological changes in the blood circulation of the eyes;
- Age category of persons over 40 years old;
- Female;
- Ignoring regular preventive examinations by an ophthalmologist.
The process of developing angle-closure glaucoma can begin suddenly. However, sometimes it is preceded by symptoms indicating the approach of a dangerous condition. These include the following signs of acute glaucoma:
- Blurred vision. Due to excessively high eye pressure, the cornea does not receive sufficient nutrition. Therefore, its tissues become less transparent.
- Looking at the light, the patient sees all the shades of rainbow circles. This “harbinger” manifests itself most clearly in the morning, immediately after waking up.
These symptoms indicate the development of pathology, which at any moment will “escalate” into an attack. Only an ophthalmologist will determine the extent of the disorder and prescribe the correct treatment.
Urgent actions
Help with an acute attack of glaucoma is provided in the ophthalmology department. Therefore, the symptoms of an emergency condition require an urgent call to a team of medical workers. Before their arrival, witnesses to the attack need to do the following:
- Lay the patient down;
- Give him a hot foot bath (will reduce blood flow to the head);
- Apply mustard plasters to calves.
Arriving doctors use eye drops to reduce the acute symptoms of the attack. We are talking about Pilocarpine drops, which need to be instilled every 10 minutes. Intravenous administration of Diacarb is indicated. For pain relief, intramuscular injection of Analgin or Ketorol is used.
The victim is delivered to a medical facility lying down.
Conservative and surgical treatment
After urgent actions, the patient is taken to a medical facility. There, the ophthalmologist carries out diagnostics appropriate to the situation and determines the type of therapy. Glaucoma treatment is carried out only in a hospital setting! Compliance with this condition is mandatory. After all, if the condition does not improve, having determined the type of surgical intervention, doctors will choose the type of surgery for glaucoma.
During the period of conservative treatment, eye drops are prescribed. The most commonly used drugs are:
- Pilocarpine 1%. Stabilizes intraocular pressure;
- Timolol 10.5%. Use only in the absence of contraindications;
- Azopt 2%. Reduces the manifestations of glaucoma.
As an addition to treatment, osmotic agents or corticosteroids are used. Anti-vomiting, sedative or analgesic medications are used according to indications.
The lack of results after 4 hours from the start of therapy is an indication for the use of a “volatile mixture”.
Remember!
Stopping the symptoms of an attack does not mean getting rid of the disease. After treatment, maintenance therapy is indicated in compliance with all prevention rules.
If improvement after therapy does not occur within 12-24 hours, surgery is prescribed. Laser surgeries are most often used. The doctor uses laser beams to burn through the iris of the eye. The resulting small hole helps to properly distribute the accumulated fluid throughout the eye and prevent a reoccurrence of the attack.
However, sometimes such intervention remains ineffective. In this case, an operation is indicated, during which the distance between the cornea and the iris increases.
The absence of well-chosen treatment tactics will lead to complete loss of vision in the patient.
Preventive measures
People who have been diagnosed with glaucoma should constantly follow preventive rules so as not to provoke an attack. All patients over 40 years of age who have vision problems should heed the same recommendations.
- Systematic observation by an ophthalmologist for preventive purposes will allow you to regularly monitor the level of intraocular pressure;
- Correct distribution of hours of rest and workload;
- Maintaining a healthy lifestyle;
- Balanced diet;
- Wear lenses or glasses prescribed by your doctor at all times;
- Elimination of excessive physical activity;
- Refusal of clothing that tightens the body, which interferes with proper blood circulation;
- Daily walks in the fresh air;
- Elimination of stressful situations;
- Proper fluid intake.
Those patients diagnosed with glaucoma are prescribed drugs that maintain intraocular pressure. It is extremely important for such patients not to fall under the “influence” of provoking factors.
Treatment
After providing first aid to the patient, he is referred to the appropriate specialist. Treatment of an acute attack of glaucoma should only be carried out by a qualified doctor in an ophthalmology hospital.
Locally, the patient is prescribed eye drops for glaucoma. The most commonly used drugs are:
- 1% solution of Pilocarpine. During the first hour, it is injected into the conjunctival cavity every 10 minutes, then every half hour or hour. After normalization of IOP, the drug is used several times a day.
- 0.5% Timolol solution. Prescribed in the absence of systemic contraindications. Instilled into the affected eye 2 times a day.
- 2% Azopt solution. Another effective antiglaucomatous agent. Apply 3 times a day.
Additionally, osmotic agents (Glycerin, Urea), corticosteroids (Dexamethasone) or other necessary drugs may be prescribed. Mannitol, Furosemide, sedatives, painkillers, and antiemetics can be administered parenterally to the patient. If within 3-4 hours the IOP does not drop below 35 millimeters of mercury, the patient is administered a lytic mixture (Aminazine, Diphenhydramine and Promedol).
If there is no expected effect within 12-24 hours, surgical intervention (laser irido- and gonioplasty, antiglaucomatous operations) is recommended. If proper medical care is not provided, angle-closure glaucoma leads to rapid loss of vision. More information about treating glaucoma with laser?
First aid
Treatment should be carried out by an experienced ophthalmologist or healthcare professional with sufficient knowledge. Therapy by unqualified doctors can worsen the situation. Read about eye drops for glaucoma.
Immediately after the diagnosis is made, before the patient is referred to ophthalmology, IOP must be lowered and measures taken to relieve pain. For this purpose, Diacarb is used orally, and a solution of pilocarpine in the eyes, which is instilled 3-4 times dropwise into each eye.