Drug treatment of glaucoma without surgery
With glaucoma, optic nerve atrophy and vision loss are irreversible. However, to slow down or stop development
progression of the disease is possible. Conservative and surgical methods of combating this pathology are available abroad.
Medications
are the first line of treatment for this disease. They are most effective in treating glaucoma at an early stage. One such medicine is eye drops.
With their daily use, intraocular pressure (IOP) is significantly reduced. This can be achieved by reducing the amount of intraocular fluid and improving its outflow through the drainage system of the eye.
The choice of medications and the schedule for their administration is made by an ophthalmologist. He develops a treatment plan based on the results of a comprehensive vision diagnostic.
APPOINTMENT FOR OPHTHALMOLOGICAL DIAGNOSTICS
The accuracy of diagnosis abroad exceeds 99%. This is the key to the effectiveness of the prescribed treatment. Contact MediGlobus specialists. We will organize a trip for vision diagnostics as soon as possible!
How is glaucoma treated with medication?
First, the patient is prescribed one of the first-choice drugs
. If the drug is ineffective, it is replaced with another preferred drug or a combination therapy of several drugs that have different mechanisms of action is prescribed.
During drug treatment, the patient should be regularly monitored by an ophthalmologist for 2-4 weeks
. Then the results of therapy and the patient’s condition are monitored at least once every 3 months. To prevent the development of drug resistance, they are replaced every 1-2 years.
The following types of eye drops are used in the treatment of glaucoma:
| Prostaglandins | They increase the outflow of fluid from the eye, thereby reducing intraocular pressure. Drugs of this class are used once a day. |
| Beta blockers | These medications reduce fluid production in the eye. Depending on the patient’s condition, these medications are prescribed to be taken 1-2 times a day. |
| Alpha adrenergic agonists | Drops that reduce the formation of fluid in the eye and at the same time increase its outflow. Drugs of this class are prescribed 2-3 times a day. |
| Carbonic anhydrase inhibitors | Reduces fluid production in the eye. They are used 2-3 times a day. |
| Rho kinase inhibitors | Medicines that reduce eye pressure. They inhibit rho-kinase enzymes responsible for the increase in fluid. These drugs are used 1-2 times a day. |
| Miotic or cholinergic drugs | Increases the outflow of fluid from the eye. They are taken up to 4 times a day. |
Results of conservative treatment
All patients with glaucoma undergo drug therapy to reduce intraocular pressure. According to the American Society of Ophthalmology
, it is possible to stop the development of the disease with the help of eye drops in 60% of patients. The remaining 40% of patients are indicated for laser and surgical treatment.
Complications of drug therapy for glaucoma
Glaucoma medications can help preserve your vision, but they can also cause side effects. Correct prescription of medications does not cause complications in 96% of cases
. Rarely, certain medications and eye drops may cause:
- tingling or itching in the eye; redness of the eye and skin around it; clouding of the iris;
- cardiopalmus; breathing problems; dry mouth.
How much does drug treatment for glaucoma cost abroad?
Price of drug treatment for glaucoma abroad
is formed taking into account the stage of the disease, as well as the choice of specific drugs. The cheapest treatment for this disease is in clinics in Turkey or Korea. The initial cost of the course is $200.
Clinics for drug therapy for glaucoma
To combat glaucoma with the help of medications, foreign patients choose clinics in Germany, Israel, Austria, Turkey and Korea. At the same time, they go not only to specialized medical institutions, but also to general hospitals. Among them:
Network of clinics Liv Hospital
Read about the clinic →
Vienna Private Clinic
Read about the clinic →
APPOINTMENT AT THE CLINIC
To sign up for glaucoma treatment abroad, leave your request. Click the button below, fill out your contact information and wait for our call. MediGlobus coordinators respond within 30 minutes.
Reviews from patients about conservative treatment of glaucoma abroad
Where it was held:
Memorial Ataşehir Clinic
What procedure:
Drug therapy
Patient age:
49 years old
Patient from:
Kiev
Angelina:
“I was treated for glaucoma without surgery in Turkey. This was possible since the disease had just begun to manifest itself. To relieve the condition, tablets and eye drops were prescribed. Even now I take these medications on schedule. I can say one thing - it works! Vision does not deteriorate, and this is the main thing!”
Where it was held:
Spreebogen
What procedure:
Drug therapy
Patient age:
45 years old
Patient from:
Kharkov
Yaroslav:
“I went to Germany for treatment of glaucoma with normal eye pressure. For this I chose the Spreebogen clinic. I was prescribed a course of drug therapy here. Taking medication every day bore fruit: the progression of the disease stopped. I'm happy with the result.”
How do antiglaucoma drops work?
When using antiglaucoma drops systematically, the patient needs to be aware of the following features of their effects:
- The pressure decreases after the first use. Repeated use enhances the effect.
- The effect of the drops is of an increasing nature (intensifies after each subsequent instillation).
- In some cases, the drug not only does not lower, but also increases intraocular pressure.
Considering the last point, to select a specific antiglaucoma drug, it is better to contact an ophthalmologist, who will conduct a diagnostic test and determine the patient’s individual reaction to the drug. Remember that by using the drug without a doctor's recommendation, you are putting your eyes at serious risk and can cause irreparable damage to them!
If the doctor has prescribed anti-anglaucoma drops, the patient should regularly come for examination over 2-3 weeks. Further, the frequency of visits can be reduced (once every 3 months). Since the human body gets used to the drug over time, it needs to be replaced every one and a half to two years and re-checked by an ophthalmologist.
Trabeculoplasty – laser treatment of open-angle glaucoma
Trabeculoplasty
is a minimally invasive surgery performed using a laser. It is intended for people with open-angle glaucoma. An ophthalmologist uses a laser machine to improve the drainage system of the eye. After such an intervention, the outflow of fluid is normalized and the pressure in the eyes decreases.
Indications for selective trabeculoplasty
This method is used when medications in the form of eye drops are ineffective or cause serious side effects. It can be used as an initial treatment for glaucoma. Trabeculoplasty is suitable for patients with primary or secondary open-angle glaucoma.
Contraindications to laser trabeculoplasty
This treatment method is contraindicated for inflammatory or uveitic glaucoma. It is also not used to combat congenital and closed forms of the disease. Other contraindications are specified by the ophthalmologist.
How is laser trabeculoplasty performed?
Laser trabeculoplasty uses a focused beam of light to treat the drainage system of the eye. The operation does not require hospitalization of the patient.
Before the intervention, anesthetic drops are instilled into the eye. Using a special microscope, laser beams
delivered to the affected areas of the drainage area of the eye.
The procedure lasts 5-10 minutes. The patient does not experience any pain
. During trabeculoplasty, he may see flashes of green and red color. 3 days after surgery, intraocular pressure decreases.
APPOINTMENT FOR TRABECULOPLASTY
Modern laser trabeculoplasty techniques allow 9 out of 10 patients to stop the progression of glaucoma. Contact our coordinators. We will organize a trip for treatment to a clinic that fully meets your requirements.
Results of the laser trabeculoplasty method
The final results of treatment occur after 1-3 months. Trabeculoplasty is performed to preserve the vision that is present at the time of surgery. It will slow down the development of pathology, and will not restore or improve lost vision. The surgery is successful in about 3 out of 4 patients.
Complications after laser trabeculoplasty
The operation takes place without complications in 97% of cases
. In some patients, the pressure in the eyes temporarily increases after the intervention. To relieve this condition, eye drops are prescribed.
Temporary side effects of trabeculoplasty include:
- inflammation and clouding of the iris; decreased vision; pain.
Cost of trabeculoplasty abroad
Laser trabeculoplasty price
is formed taking into account the level of the medical institution and the doctor’s qualifications. Also, the cost of laser treatment for glaucoma is influenced by the surgical technique.
The estimated price of trabeculoplasty abroad is:
| A country | Price |
| Türkiye | from $2,000 |
| Germany | from €2,800 |
| South Korea | from $2,500 |
| Austria | from €2,500 |
Where is trabeculoplasty performed abroad for glaucoma?
Laser treatment of patients with glaucoma is carried out in specialized and highly specialized medical centers. Many patients choose clinics in Turkey and Germany for such interventions. The most popular hospitals among medical tourists are:
Batygoz Ophthalmological Center
Read about the clinic →
Hangil Eye Clinic
Read about the clinic →
Reviews of selective trabeculoplasty abroad
Where it was held:
Dunyagöz Clinic
What procedure:
Trabeculoplasty
Patient age:
38 years old
Patient from:
Murmansk
Igor:
“After reading many reviews about trabeculoplasty abroad, I decided to go to Turkey for glaucoma treatment. My choice fell on the Dunyagoz clinic. Here I underwent additional diagnostics and then underwent laser trabeculoplasty. The procedure lasted no more than 10 minutes. The result is that the disease is stopped.”
Where it was held:
Hangil Hospital
Which procedure:
Trabeculoplasty
Patient age:
45 years old
Patient from:
Irkutsk
Ksenia:
“I decided to leave a review about laser trabeculoplasty, which I performed abroad. I have stage 3 glaucoma. I knew that only surgery could help me. Therefore, I turned to the Korean clinic Hangil. Here I underwent trabeculoplasty with an argon laser. Everything went well. My treatment for eye glaucoma is successful. My vision has stopped deteriorating.”
General characteristics of laser iridectomy and laser trabeculoplasty
Laser iridectomy is performed to normalize the pressure in the eye chambers. This procedure effectively treats angle-closure and mixed forms of glaucoma.
There are situations when laser iridectomy is performed after surgery. This procedure has a preventive purpose; using a laser, you can significantly reduce the risk of relapse.
Laser trabeculoplasty is a procedure in which burns are applied to the inside of the trabecula. This operation helps to improve the permeability of the trabecular diaphragm and reduce the risk of blockade of the Schlemm canal.
Trabeculoplasty is prescribed for primary open-angle glaucoma that cannot be treated with conservative medicine. A local anesthetic is used for the operation.
Iridotomy – laser treatment of angle-closure glaucoma
Iridotomy
is an operation to treat angle-closure glaucoma with a laser. Using a laser machine, the ophthalmologist creates a tiny hole in the iris. This hole allows fluid inside the eye to move normally through the drainage system. The procedure is sometimes called an iridectomy.
TRIP FOR IRIDOTOMY ABROAD
MediGlobus medical coordinators will help resolve organizational issues of a medical trip: visa processing, hotel booking, transfer and meeting at the airport.
Indications and contraindications for iridotomy
The procedure is used to combat mixed or closed-angle glaucoma
primary and secondary etiology. This is an additional measure that is prescribed after the main surgical intervention for incomplete excision of the iris.
Iridotomy is also performed as a preliminary step before trabeculoplasty. It is indicated for patients with open-angle glaucoma
and a relatively narrow angle of the anterior eye chamber.
Iridectomy cannot be done if the cornea is clouded and the depth of the anterior chamber of the eye is shallow. It is contraindicated for inflammatory lesions of the optical system in the acute phase.
How is glaucoma treated with iridotomy?
The procedure is performed on an outpatient basis. Before it begins, the ophthalmologist uses eye drops to relieve pain and constrict the pupil. A special contact lens is placed on the eye
. It makes it possible to direct a high-energy laser beam at the iris and make a hole in it.
- Iridotomy lasts from 5 to 15 minutes. The patient can return home 2 hours after the intervention. Within the first hour after creation holes in the iris
vision is blurry. Then it begins to recover.
After treatment, the eye patch is not used. Anti-inflammatory eye drops are prescribed for 3-5 days. A follow-up visit to the ophthalmologist is carried out after 1-6 weeks. If the patient has used eye drops to treat glaucoma
before the procedure, they are not canceled.
Results of iridotomy
The effectiveness of the procedure varies depending on the degree of disease progression. With stage 1 and 2 glaucoma, positive results can be achieved in 82% to 99% of cases.
Complications of iridotomy
This procedure has the lowest risk of complications compared to other glaucoma treatment methods. In rare cases, patients experience inflammation or bleeding inside the eye.
How much does an iridotomy cost abroad?
The cost of the procedure is determined taking into account the pricing policy of the country, as well as the level of the medical center.
The starting price for an iridotomy per eye is:
| A country | Price |
| Türkiye | from $320 |
| Germany | from €900 |
| South Korea | from $400 |
| Austria | from €700 |
Where is iridotomy performed abroad?
Dunyagöz Ophthalmology Center
Read about the clinic →
Soon Chung Hyang University Hospital
Read about the clinic →
Reviews about the treatment of glaucoma using iridotomy
Where it was held:
Liv Clinic Ankara
What procedure:
Iriditomy
Patient age:
44 years old
Patient from:
Odessa
Olga:
“I went to Turkey for laser treatment of glaucoma with low intraocular pressure. I chose the Liv Ankara clinic. The procedure was painless and quick. My vision is no longer deteriorating. The disease has receded.”
Where it was held:
Batygoz Clinic
What procedure:
Iridotomy
Patient age:
39 years old
Patient from:
Gyumri
Anahit:
“I decided to leave a review about laser treatment for glaucoma. To carry out the procedure, I went to Turkey, Batygoz clinic. All I can say is that they helped me here. The disease has not yet developed. Thank you!"
Pros and cons of the most popular anti-glaucoma surgeries
There are many options for anti-glaucoma operations that involve the use of a laser. Some of the most common and recognized are laser iridotomy (iridectomy) and laser trabeculoplasty. Let's look at their common advantages:
- Fluid leaves the body through natural channels.
- A local anesthetic is sufficient.
- Surgical intervention on an outpatient basis is possible.
- It does not take much time for complete post-operative recovery.
- The body tolerates surgery more easily than with classical surgery.
- Affordable surgery price.
Minuses:
- As the disease progresses for a long time, the quality of treatment decreases.
- The risk of inflammatory processes in the eye.
- Possibility of disruption of the structure of epithelial cells of the cornea, vessels of the iris and lens.
Trabeculectomy – surgical treatment of glaucoma at an advanced stage
Trabeculectomy
is an operation that is performed to reduce intraocular pressure in stage 3 and 4 glaucoma. It is one of the most common surgical methods to combat this pathology in adults. The intervention is used for open-angle and chronic angle-closure glaucoma. It is also used to treat pathologies of inflammatory and traumatic nature.
APPOINTMENT FOR TRABECULECTOMY
Foreign medical centers adhere to modern protocols for the treatment of glaucoma. Operations to combat this pathology are performed by ophthalmologists with 20 years of experience. Contact MediGlobus. We will help you choose the best glaucoma surgery specialist and arrange an appointment with him.
Contraindications for trabeculectomy surgery for glaucoma
- previous failed trabeculectomy; damaged conjunctiva; Stevens-Johnson syndrome;
- neovascular form of glaucoma; uveitic glaucoma; complete blindness.
How is trabeculectomy performed for glaucoma?
During surgery, the eye surgeon creates a tiny flap in the sclera
. He then makes a small hole in the eye to release the fluid. Fluid from the eye may leak through the flap into the bleb, where it is absorbed by the intraocular tissues. This helps reduce blood pressure and slow down the progression of the disease.
Trabeculectomy is performed under general or local anesthesia. It lasts from 45 minutes to 1 hour. After the intervention, a patch is applied to the eye, which is removed after 1-2 days.
After surgery, patients stop taking any glaucoma medications. They are prescribed a course of antibiotics and steroid drugs to prevent the risk of infection.
Prognosis of trabeculectomy in the treatment of glaucoma
Trabeculectomy is the “gold standard” in the fight against advanced disease. According to the World Glaucoma Association, after it is carried out, 80% of patients manage to maintain normal intraocular pressure for 5 years or longer.
Complications of trabeculectomy
Although trabeculectomy is considered a safe procedure, it does have some side effects. These include:
- infection of the wound surface; drooping eyelid; swelling around the eye and bleeding;
- scarring; excessive decrease in intraocular pressure; retinal disinsertion.
Cost of trabeculectomy surgery abroad
The cost of trabeculectomy in foreign hospitals is determined taking into account the severity of the pathology, as well as the qualifications of the ophthalmologist.
The initial price for this intervention on one eye is:
| A country | Price |
| Türkiye | from $2,100 |
| Germany | from €3,500 |
| South Korea | from $2,360 |
| Austria | from €3,100 |
Where is glaucoma surgically treated abroad?
Operations for this disease are successfully carried out in ophthalmological centers and departments of leading hospitals in Turkey, Korea or the Czech Republic. Medical tourists also travel to Israel and Germany for surgical treatment of glaucoma. The following clinics are in demand in these areas:
Spreebogen Ophthalmology Center
Read about the clinic →
Chaim Sheba Clinic
Read about the clinic →
Reviews about trabeculectomy
Where it was held:
Batygoz Clinic
What procedure:
Trabeculectomy
Patient age:
57 years old
Patient from:
Sevastopol
Nikolay:
“I would like to leave my feedback regarding glaucoma surgery. The intervention was carried out in the Turkish Batigöz hospital. To be honest, I was a little worried that it would get worse, but everything went well. In 40 minutes they were able to stop the progression of the disease. It's been 2 years now and my vision remains the same. Thank you!"
Where it was held:
Spreebogen Clinic
Which procedure:
Trabeculectomy
Patient age:
50 years old
Patient from:
Kharkov
Michael:
“I went to Germany for treatment of stage 4 glaucoma. I didn’t want to get treatment in my native country. I've already healed. So, I survived from stage 1 of glaucoma to the last. I chose the Spreebogen clinic. Here I had a trabeculectomy, which was able to slow down the disease. I hope the results last a long time.”
Some modern antihypertensive drugs for the treatment of ocular hypertension and glaucoma
Professor A.A. Ryabtseva, Mohamed Habibur Rahman Sheikh Moscow Regional Research Clinical Institute (MONIKI) named after. M.F. Vladimirsky
The authors believed that one of the most usable methods of treatment of glaucoma is combination of antiglaucoma medications. Most popular are still miotics (Oftan Pilocarpin, Santen) and beta-blockers (Oftan Timolol, Santen). Patient comfort, tolerance and compliance however related to combination eyedrops of timolol and pilocarpin Fotil and Fotil forte, Santen. The epinephrines (Oftan Dipivefrin, Santen) could be employed as the initial therapy in both primary open angel glaucoma and, when treated, ocular hypertension, postoperative treatment. Unlike pilocarpin, epinephrine does not produce miosis and accommodative spasm. The side effects of epinephrine are well known because of long experience and usually not serious.
The most important and widespread method of correcting intraocular pressure (IOP) for ocular hypertension and glaucoma is complex drug therapy using a large arsenal of local antihypertensive drugs. Among them, the most popular are cholinomimetics, sympathomimetics, beta-blockers, adrenergic agonists, carbonic anhydrase inhibitors, as well as combination drugs that have different mechanisms of action on ophthalmotonus and, as a rule, mutually complement the hypotensive effect of each other.
The most widely used antiglaucomatous drugs include miotics. Their main advantage is the pathogenetic direction of action. Constriction of the pupil with retraction of the iris root from the structures of the anterior chamber angle and improved access of aqueous humor to the drainage system of the eye, tension of the trabecular apparatus of the eye during miosis directly improves the outflow of intraocular fluid (IOH).
Among the miotics, pilocarpine has been used for more than a hundred years as a consistently effective treatment for glaucoma. The most commonly used are 1 and 2% solutions. The duration of action of pilocarpine is from 4 to 8 hours. The combination of pilocarpine with methylcellulose or polyvinyl alcohol allows you to extend the effect of the drug up to 12 hours. One of the forms of long-acting pilocarpine is Oftan Pilocarpine (SANTEN), which is a 1% solution of pilocarpine hydrochloride in combination with polyvinyl alcohol. According to the results of clinical use of Oftan Pilocarpine, fairly good tolerability of this form was noted.
Oftan Pilocarpine eye drops, when instilled into the eye, quickly penetrate the cornea. Iphthalmotonus decreases after 2 hours by an average of 6–7 mmHg. The duration of action of Oftan Pilocarpine with moderate ophthalmotonus exceeds 6 hours (maximum up to 8 hours), with high IOP it does not exceed 3–4 hours after a single instillation. The maximum constriction of the pupil to 2 mm occurs 40–60 minutes after instillation and lasts up to several hours. A spasm of accommodation is observed after an hour and disappears after 2 hours. When combined with sympathomimetics, beta-blockers, carbonic anhydrase inhibitors, the effectiveness of Oftan Pilocarpine increases.
Side effects of pilocarpine include persistent miosis with long-term use of the drug, transient headache, follicular conjunctivitis, etc. The use of pilocarpine is contraindicated in iritis, iridocyclitis and other inflammatory diseases of the anterior part of the eye, with lesions of the cornea.
The introduction of b-blockers into ophthalmological practice allowed, along with a pronounced and long-term decrease in ophthalmotonus in ocular hypertension and glaucoma, to avoid the negative effect of miotics on accommodation and pupil diameter, and not significantly change blood circulation in the anterior part of the eyeball. Beta blockers effectively inhibit the interaction of sympathomimetic neurotransmitters with b1 and b2 receptors. The most well-known and widespread in ophthalmological practice is the non-selective b1,2-adrenergic blocker timolol maleate.
One of the forms of this drug is Oftan Timolol (SANTEN), which is available in the form of 0.25% and 0.5% solutions of eye drops. Oftan Timolol does not affect membrane stability. It inhibits the secretion of aqueous humor, thereby lowering intraocular pressure. The effect of Oftan Timolol on the outflow of aqueous humor from the eye is considered insignificant. Oftan Timolol is well absorbed in the eye. The hypotensive effect occurs 20 minutes after instillation, reaches a maximum after 2 hours, and lasts 12–24 hours. Of great importance is that the drug evens out the daily IOP curve, preventing significant fluctuations in ophthalmotonus during the day.
Local and systemic side effects may occur in patients concomitantly using oral b-blockers or calcium channel blockers. Local adverse reactions include dry eye, swelling of the corneal epithelium. Rarely, punctate superficial keratitis (superficial punctate keratopathy), corneal anesthesia. General side effects are extremely rare: decreased blood pressure up to collapse, bradycardia, arrhythmia, dizziness, muscle weakness. Recently, data have been provided on the inhibitory effect of the drug on mental status. In rare cases, in sensitive patients it can cause depression and psychoasthenia.
Oftan Timolol is contraindicated in patients with corneal dystrophies, dry keratitis, bonchial asthma, chronic pulmonary diseases, sinus bradycardia, and heart failure. It should be used with caution in patients with diabetes mellitus, especially in labile cases. It is not recommended for primary use in low-tension glaucoma.
Typically, Oftan Timolol is recommended to instill 1 drop (30 µl) 1-2 times a day into the affected eye. It is recommended to begin treatment with instillation of a 0.25% solution. If this is not enough, a 0.5% solution should be used. The difference in the hypotensive effect of 0.25 and 0.5% solution is about 10–15%.
Oftan Timolol eye drops can be combined with other drugs for the treatment of glaucoma, with the exception of other local b-blockers: cholinomimetics (pilocarpine), sympathomimetics (adrenaline, Oftan Dipivefrin), carbonic anhydrase inhibitors (acetazolamide, dorzolamide hydrochloride).
Despite the listed effective mechanisms of action on ophthalmotonus, b-blockers are characterized by a lack of effect on the outflow of intraocular fluid, which leads to a less stable and long-lasting result than the hypotensive effect when improving outflow. Therefore, the created combined form of b-blockers and pilocarpine provides greater effectiveness of drug therapy. The most optimal option for combination drugs can be considered a combination of timolol and pilocarpine, produced by SANTEN: Fotil and Fotil Forte. Fotil is available in the form of a solution, 1 ml of which contains 20 mg of pilocarpine hydrochloride and 5 mg of timolol. 1 ml of Fotil Forte solution contains 40 mg of pilocarpine hydrochloride and 5 mg of timolol.
The difficulty in combining timolol with pilocarpine is that a certain pH value of the buffer solution is required for optimal stability and penetration through the cornea. The buffer solution in eye drops containing timolol creates a pH of about 7, which makes pilocarpine unstable. Conversely, buffer systems in pilocarpine eye drops create a pH between 4 and 5 - at these values, the absorption of timolol by the cornea is reduced. In the combined preparations Fotil and Fotil Forte, all components are in one bottle at a pH of about 5.3, when both components remain stable. Methylhydroxypropylcellulose is added to the combination formulation to increase viscosity and lengthen contact time in order to counteract the effect of pH on corneal penetration.
The hypotensive effect of Fotil occurs 30 minutes after instillation and lasts for at least 24 hours. The maximum decrease in ophthalmotonus is observed in periods from 2 to 6 hours and is more than 32% of the initial level. In this case, a narrowing of the pupil of up to 2–3 mm, characteristic of the action of pilocarpine, is noted. Dosage of Fotil and Fotil forte in the treatment of glaucoma – 1 drop 2 times a day. Fotil can be used to treat almost all forms of glaucoma. When prescribing Fotil, you should stop taking other medications used to treat glaucoma.
Among the side effects, reactions directly related to the effect on the eye were noted: a quickly passing burning sensation and moderate pain in the eye immediately after instillation with a duration of 30 minutes to 1 hour, temporal and supraorbital headache, blurred vision for up to several hours, spasm of the ciliary muscle induced myopia. Systemic adverse reactions may include nausea, diarrhea, increased sweating, salivation and a drop in blood pressure due to stimulation of the parasympathetic nervous system, asthma attacks, congestive heart failure, arrhythmia and other reactions associated with the use of timolol and pilocarpine.
It should be noted that the use of combined eye drops Fotil and Fotil Forte significantly improves the quality of life of patients with glaucoma and allows achieving stable compensation of IOP. According to our observations, about 70% of patients forced to instill several eye drops at the same time do not comply with the treatment regimen, which leads to IOP decompensation. This is due to the fact that patients confuse eye drops, skip the next instillation, and exclude some eye drops without consulting a doctor. When using ready-to-use eye drops Fotil and Fotil Forte, all of the above difficulties are automatically eliminated, and in most cases, stable compensation of IOP is noted.
The group of drugs that lower IOP includes sympathomimetics. They do not cause spasm of the ciliary body, dilate the pupil, reduce the production of aqueous humor, and stimulate the uveoscleral outflow of fluid. Among the sympathomimetics, the most famous is adrenaline, which is available in the form of hydrochloride, borate and bitartrate. Epinephrine has been used to treat glaucoma for over 40 years; up to 88% of cases of primary open-angle glaucoma can be treated with epinephrine.
Several years ago, an alternative form of epinephrine appeared on the market - dipivalidrenaline or dipivefrine hydrochloride. Oftan Dipivefrin (SANTEN) as a sympathomimetic agent stimulates b-receptors in the ciliary processes, reduces the production and increases the outflow of intraocular fluid. Composition and release form: 1 ml of eye drops contains dipivefrin hydrochloride 1 mg, as well as benzalkonium chloride, sodium edetate, mannitol, sodium chloride, hydrochloric acid to pH 3; transparent, colorless solution, supplied in white plastic dropper bottles of 5 ml, 1 pc in a box.
Oftan Dipivefrin, being a precursor of adrenaline, belongs to a group of drugs that undergo biotransformation to form the parent compound, after which they become pharmacologically active. This alternative form of adrenaline is formed by the esterification of adrenaline with two molecules of pivalic acid, i.e. with the addition of two pivalyl chains and the formation of dipivalidrenaline. Pivalyl groups enhance the lipophilicity of adrenaline, improving its ability to penetrate the anterior chamber of the eye. The ability of dipivefrin to dissolve in fats is 100–600 times greater than that of epinephrine, and its ability to penetrate the cornea is 17 times higher. Thanks to this, Oftan Dipivefrin can be used in significantly lower concentrations than adrenaline.
Dipivefrin ester compounds undergo hydrolysis in the anterior tissues of the eye, already in the cornea and in the endothelium of blood vessels, and adrenaline (the active ingredient) is restored. Almost all tissues contain enzymes capable of hydrolyzing dipivefrin ester compounds.
Adrenaline increases the content of cyclic adenosine monophosphate (cAMP) in the trabecular diaphragm of the anterior chamber angle, the state of which determines the level of resistance to the outflow of intraocular fluid.
After topical application of Oftan Dipivefrin, the outflow slowly increases and reaches its maximum after 2 hours. Elevation is maintained for 12–20 hours.
The effect on the production of aqueous humor is associated with stimulation of b-receptors of the ciliary processes of the ciliary body and is biphasic in nature. In the initial phase, there is an increase in the production of intraocular fluid, which is insignificant and short-term (1 hour). At the same time, the level of cAMP increases in non-pigmented epithelial cells. During the second phase, although the cAMP content has already been restored, the sensitivity of adrenergic receptors decreases. This change in receptors is believed to cause a decrease in the production of intraocular fluid. The fact is that adrenaline is removed faster from the ciliary processes than from the trabecular tissue, primarily due to the outflow of aqueous humor. The cumulative effect of changes in IOP production and efflux on IOP involves an initial short-term (less than 1 hour) increase in pressure, followed by a decrease lasting longer (12 hours) and four times the magnitude of the initial short-term increase. The initial increase in IOP is often minor.
This form of epinephrine minimizes the side effects of epinephrine and enhances therapeutic efficacy while reducing drug concentrations and reducing the risk of ocular and systemic side effects.
Oftan Dipivefrin has a hypotensive effect in concentrations as low as 0.025%. At a concentration of 0.1% Oftan Dipivefrin, the effectiveness is equal to a 1–2% solution of adrenaline. The reduction in IOP when using a 0.1% solution of Oftan Dipivefrin is comparable to the effect of a 0.5% solution of betaxolol. Low concentration significantly reduces the risk of side effects, both local and systemic, and allergic reactions are less likely to develop.
Oftan Dipivefrin is effective with long-term use, including in combination with other antiglaucoma drugs. The most effective use of Oftan Dipivefrin is in combination with pilocarpine, because dipivefrine neutralizes the pronounced constriction of the pupil caused by pilocarpine. With this combination, the hypotensive effect of both drugs is enhanced, and the pupil size remains almost normal. In terms of effectiveness, Oftan Dipivefrin is not inferior to a 2% solution of adrenaline, but it is much easier to tolerate by patients.
Oftan Dipivefrin eye drops are recommended for use in open-angle glaucoma, increased intraocular pressure in infectious eye diseases, ocular hypertension, and secondary glaucoma. Oftan Dipivefrin can be used as an alternative treatment for the initial stage of open-angle glaucoma in cases where b-blockers are contraindicated.
Oftan Dipivefrin practically does not cause systemic side effects. Local side effects (mydriasis, maculopathy, allergic conjunctivitis, burning sensation and acute pain) are extremely rare with long-term use; and general (headache, tachycardia, extrasystole).
The first experience of using adrenaline drugs in our clinic was more than 35 years ago (Brickman V.G., 1968). Then they began to study the secretion and outflow of intraocular fluid under the action of epinephrine. It has been established that the hypotensive effect of the drug is associated with improved outflow with a decrease in the secretion of intraocular fluid.
We used Oftan Dipivefrin in patients with primary open-angle glaucoma, with increased ophthalmotonus, in the early postoperative period in cases of the development of reactive postoperative hypertension in patients after antiglaucomatous interventions, after cataract extraction (EC), incl. in combination with IOL implantation. We observed 49 patients (74 eyes) aged from 52 to 83 years, men – 26, women – 23. Two groups of patients were identified. Of these, 34 patients with postoperative hypertension: 14 patients after cataract extraction, incl. 6 after EC in combination with IOL implantation; and 20 patients with glaucoma after antiglaucomatous operations. The second group consisted of 15 patients with glaucoma, incl. 7 patients with primary open-angle glaucoma, 5 patients with combined and 3 patients with secondary glaucoma. Before using Oftan Dipivefrin, patients received parasympathomimetics, timolol group drugs, carbonic anhydrase inhibitors, and general antihypertensive drugs. However, normalization and stabilization of IOP was not achieved.
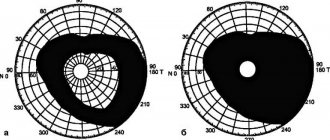
During the examination, traditional and special ophthalmological research methods were used, including visometry, biomicroscopy, ophthalmoscopy, electronic tono- and sphygmography, perimetry, and color campimetry.
The treatment method consisted of instillation of Oftan Dipivefrin into the conjunctival cavity: Dipivefrin is applied 1-2 drops into the affected eye 2 times a day. In 40 patients - in combination with a 1% solution of Oftan Pilocarpine, a 0.5% solution of arutimol, carbonic anhydrase inhibitors, as well as in combination with other antiglaucoma drugs and agents used to treat postoperative changes in the eye. The duration of use of Oftan Dipivefrin is from 2 to 36 days.
In the observed patients, the nature of the postoperative period was as follows.
Among patients with reactive hypertension who underwent antiglaucomatous operations, in the early postoperative period, a suspension of red blood cells in the anterior chamber was noted in 3 patients, and mild reactive hypertension developed in 1 case. In the late postoperative period, flat ciliochoroidal detachment was detected in 2 patients, which was treated with medication.
In the group of patients operated on for cataracts, swelling of the corneal epithelium was noted in 1 patient, descemetitis in 2 patients, and a rigid narrow pupil in 5 patients.
A decrease in IOP level was found 1 hour after instillation of Dipivefrin by an average of 4 mm Hg, and a day later - by 5 mm Hg. A long-term hypotensive effect was achieved in 27 patients with glaucoma and 14 patients with cataracts with reactive hypertension. Among patients with glaucoma, 13 people had the initial stage of open-angle glaucoma, the rest, after a more in-depth study, were classified as having an advanced stage of glaucoma with pronounced dystrophic changes in the iridocorneal zone. In them, stabilization of IOP and visual functions was achieved by combining Dipivefrin with other antihypertensive drugs. In patients with secondary glaucoma, the use of Dipivefrin was ineffective. This group mainly included patients with severe organic pathology of the main drainage path of the outflow of the intraocular fluid: gonioscopically they revealed cicatricial changes in the corneoscleral zone and the area of surgical intervention, obliteration or severe pigmentation of the sinus, extensive planar goniosynechia, as well as synechia in the pupillary zone of the iris.
The use of Oftan Dipivefrin for increasing IOP in the early postoperative period after cataract extraction and antihypertensive interventions had a positive effect in all cases. Vascular injection decreased on days 1–2 in patients after antiglaucomatous operations, and on days 2–3 after cataract extraction and intraocular lens implantation. On the part of the cornea, positive dynamics of changes were noted under the influence of Oftan Dipivefrin instillations: the area of epithelial edema decreased, and the phenomena of descemetitis decreased in the first three days. The dynamics of hemorrhagic complications in the early postoperative period were as follows: a suspension of red blood cells, blood smears on the iris, and hyphema decreased after instillation of the drug in the first 40 minutes. The pupil dilated moderately, acquired a regular round shape, and the depth of the anterior chamber was normalized. Instillation of Oftan Dipivefrin did not affect the occurrence of ciliochoroidal detachment.
No side effects of Oftan Dipivefrin were detected during the observation period. There were no contraindications for the prescription of Oftan Dipivefrin eye drops.
Thus, Oftan Dipivefrin improves the course of the postoperative period, relieves reactive postoperative hypertension after planned cataract extraction operations, EC in combination with IOLs, antiglaucomatous operations, reduces the inflammatory reaction, and promotes faster resolution of hemorrhages.
The selectivity of the action of Oftan Dipivefrin in various forms of glaucoma was revealed. The drug is most effective in the initial stage of open-angle glaucoma and in the early stages (first 2–7 days) of postoperative hypertension. It is possible to combine Oftan Dipivefrin with other antihypertensive drugs, as well as in combination with a number of drugs used to relieve reactive eye syndrome.
It is advisable to further study the action of Oftan Dipivefrin and widely use it in practice.
(Visited 18 times, 1 visits today)
Glaucoma valve implantation
- Glaucoma valve implantation
used in the treatment of complex and advanced glaucoma in adults and children. Such devices are designed to drain intraocular fluid from the anterior chamber into the external reservoir, where, approximately 4-6 weeks after surgery, a fibrous capsule is formed that regulates the outflow.
Most often, the Ahmed glaucoma valve
. It contains a flow restrictor of intraocular fluid, which prevents its excessive drainage.
APPOINTMENT FOR GLAUCOMA VALVE IMPLANTATION
MediGlobus specialists will help you organize a trip to implantation of a drainage system for glaucoma in a child or adult. We are in touch with our patients 24/7.
Indications and contraindications for glaucoma valve implantation
The operation is indicated for patients for whom drug therapy for glaucoma has been ineffective. It is also used when glaucoma surgery has failed. Glaucoma valve implantation as a primary procedure is performed when:
- neovascular glaucoma - increased intraocular pressure associated with vascular disease of the eye, in particular diabetes;
- traumatic form of the disease; childhood glaucoma; glaucoma caused by developmental defects of the eye.
A glaucoma valve implant cannot be installed in cases of eye inflammation, blindness, or severe diseases of the nervous, cardiovascular, or respiratory systems.
How is glaucoma valve implantation performed?
The intervention is performed under general or local anesthesia. It lasts 25-30 minutes. During the operation, the ophthalmologist makes a conjunctival incision
based on the vault in the upper part of the eyeball.
The implant is fixed between the two rectus muscles. A silicone tube that drains fluid inside the eye is inserted 2-3 mm into the anterior chamber, ciliary groove or vitreous cavity.
After installing the drainage system, the superficial scleral flap is returned to its place and fixed with two sutures. To prevent infection
of the operated area, the doctor injects a broad-spectrum antibiotic under the conjunctiva. He then applies a monocular patch.
Results and complications of drainage installation for glaucoma
The effectiveness of this technique is about 80%
. The operation takes place without complications in 7 out of 10 cases. In patients after installation of the implant, there may be surges and decreases in intraocular pressure. This is due to the inflammatory process in the operated area or too much fluid outflow. Such side effects require monitoring by a doctor. If necessary, the patient undergoes repeated intervention.
How much does a glaucoma implant cost abroad?
Glaucoma valve implantation abroad is performed by qualified eye surgeons who have more than 10 years of experience in such interventions. The cost of this operation varies depending on the characteristics of the disease.
The estimated cost of installing an implant is:
| A country | Price |
| Türkiye | from $2,300 |
| Germany | from €3,900 |
| South Korea | from $2,600 |
| Austria | from €3,200 |
Where is glaucoma valve implantation performed abroad?
To undergo valve implantation for glaucoma, foreigners most often travel to Turkey or Germany. Among the most popular medical institutions in this area are:
Memorial Clinic Network
Read about the clinic →
University Hospital Munich
Read about the clinic →
What drugs are contraindicated in the treatment of glaucoma?
Treatment of glaucoma: antidepressants are contraindicated
For patients with glaucoma, there are a number of restrictions on taking medications. The thing is that they can make the situation worse. Here is a list of such medications:
- Painkillers (Aspirin, Analgin and their analogues) can cause an attack of glaucoma due to swelling and swelling of the lens, as well as narrowing of the anterior chamber of the eye.
- Nitrate-based vasodilators
- Nasal drops such as Naphthyzin, Oxymetazoline, Xylometazoline, effective in treating the nasal cavity, can cause a short-term jump in IOP. Drops can be replaced with products with an antihistamine component.
- Antiallergic drugs in the form of drops containing Diphenhydramine are especially dangerous for patients with IOP at the last stage. To avoid a negative reaction, it is safer to take tablets instead of drops.
- Hypertensive drugs that lower blood pressure affect the condition of blood vessels in general and the eyes in particular. If your blood pressure rises, you need to talk to your doctor about choosing the right medication.
- Antidepressants.
- Sedatives and hypnotics . The preparations Donormil and Unisome contain doxylamine. By blocking the fluid flow, IOP increases. In stressful situations, taking valerian is safe.
- Oral contraceptives (Marvelon, Siluet, Silest, etc.) contain female hormones. When taken, the hormonal balance of the body is disrupted, which is unpredictable for intraocular pressure.
- Atropine and its analogues , used in ophthalmology, in glaucoma lead to weakening of the muscles of the ocular body. As a result, the accumulated fluid increases the pressure inside the eye.
As mentioned above, in addition to taking medications, it is necessary to adhere to a special regime of physical activity. It is also necessary to follow a special diet of fluid and food intake. Issues related to taking certain medications are solely within the competence of the attending physician.
Lens removal
Surgery to remove the lens of the eye
mainly performed on patients with primary angle-closure glaucoma. This type of disease occurs when fluid cannot drain from the eye. It is treated with a laser peripheral iridotomy, which opens the parts of the eye that allow fluid to drain.
In 80% of patients with angle-closure glaucoma
have cataracts. These two pathologies combine with each other and significantly impair vision. Therefore, removing the lens of the eye is the preferred option for treating cataracts and glaucoma.
Artificial lens (IOL)
its volume is significantly smaller than the natural lens. Therefore, it does not interfere with the drainage of intraocular fluid, thereby reducing pressure in the eye.
Replacing the lens stops the further development of glaucoma and prevents the need for additional surgical interventions. Artificial lenses from global manufacturers are used abroad
Germany, United States of America or Great Britain: Alcon, CarlZeiss and Rumex. They have a long service life and minimal risks of rejection by the patient’s body.
How is the lens of the eye removed?
The operation is performed under local anesthesia. It lasts from 5 to 15 minutes. The ophthalmologist makes a 2 mm incision on the cornea
. Ultrasound or laser is used to destroy the affected lens. A flexible artificial lens is installed in its place. No stitches are required. Vision is restored within 3 hours after the intervention. If necessary, the patient is prescribed eye drops to relieve the inflammatory process.
APPOINTMENT FOR EYE LENS REMOVAL
Leave a request on the website. We will call you back and tell you about the intricacies of carrying out this intervention abroad. MediGlobus is in touch with its patients at every stage of their medical journey.
Results of surgery to remove the lens of the eye
According to the results of the European Quality of Life-5 Dimensions questionnaire, 95% of patients with angle-closure glaucoma and cataracts note that after replacing the lens of the eye, vision improved and did not decrease. At the same time, 79% of patients no longer required a continuation of the course of drug therapy with eye drops. After iridotomy, this figure was only 39%.
Complications after removal of the eye lens
The operation, performed by a qualified specialist with many years of experience, reduces the risk of side effects to a minimum.
After lens replacement, some patients may experience the following complications:
- inflammation of the eye; IOL displacement; secondary cataract; hemorrhage in the eye; increased intraocular pressure.
How much does lens removal cost abroad?
The approximate cost of surgery to remove the lens of the eye abroad is shown in the table below.
| A country | Price |
| Türkiye | from $1,900 |
| Germany | from €4,300 |
| South Korea | from $3,000 |
| Austria | from €4,300 |
Which clinics perform eye lens removal abroad?
Medical tourists who need surgery to remove the lens of the eye choose Turkish, German, Korean or Czech hospitals. Most often, foreigners go to such medical institutions as:
University Hospital Cologne
Read about the clinic →
Network of clinics Acibadem
Read about the clinic →
What should not be done, what is contraindicated during treatment for glaucoma?
Treatment of glaucoma
If you have been diagnosed with Glaucoma, first of all, start leading a calm lifestyle. Stressful situations are strictly prohibited. Physical activity and emotional stress are not allowed. What else cannot be done, what is contraindicated during treatment for glaucoma? Here are situations to avoid - tips:
- Avoid situations that cause a rush of blood to the head . This could be work that involves bending the torso. For example: sweeping, work in the garden, which requires bending, as well as washing, etc. All this can lead to irreparable consequences. But you can adapt to the situation, for example: harvesting berries while sitting on a low stool or bench.
- Minor physical activity is allowed. But under no circumstances make sudden movements. This mainly concerns turning the head and bending.
- There are also restrictions on the weight lifted - up to 3 kg per arm, more is prohibited.
- Work that causes eye strain - reading, embroidery, beading - should be done in good lighting.
Take care of yourself, do not overexert yourself, rest and do not lift heavy loads. Thanks to this, you will avoid unwanted consequences associated with glaucoma and vision.
Summary
Glaucoma is a progressive eye disease that is characterized by increased intraocular pressure, decreased visual acuity and gradual atrophy of the optic nerve. Drug treatment of the disease is indicated for all patients. The progression of grade 1 and 2 glaucoma can be stopped with the help of eye drops and tablets. The maximum effect can be achieved if you adhere to the medication schedule developed by the doctor. Trabeculoplasty is a minimally invasive intervention performed for the open-angle form of this pathology. It is successful in 3 out of 4 cases. Iridotomy is indicated in the initial stages of the disease. It is used to combat the closed-angle form of pathology. During the procedure, a laser is used to create a tiny hole in the iris of the eye. This hole normalizes the outflow of intraocular fluid. Trabeculectomy is the “gold standard” for the treatment of advanced glaucoma. After its implementation, in 8 out of 10 patients, intraocular pressure is normal for 5 years or longer. Glaucoma valves are artificial filtration devices that reduce intraocular pressure by diverting fluid to the outer subconjunctival space. The effectiveness of this method is about 80%.
CONTACT MEDIGLOBUS EXPERTS
Find out more information about modern methods of treating glaucoma abroad from the coordinators of the international medical platform MediGlobus.
Acute attack of angle-closure glaucoma: how to treat it
An acute attack of angle-closure glaucoma is characterized by a critical increase in pressure in the eye. If help is not promptly provided in such a situation, this can cause serious deterioration in vision or even complete loss.
To stop an acute attack, drug therapy is used. Another procedure without which it is impossible to stop an attack is laser iridectomy. The operation, firstly, helps to normalize the outflow of intraocular fluid, and secondly, it is an effective prophylaxis to prevent the occurrence of an acute attack in the future.
Without risk to vision, you can use the above methods within 24 hours after the onset of the attack. If treatment does not produce the expected results within this period, surgery is prescribed.
Picamilon
Picamilon improves microcirculation in the vessels of the brain and eyeball. Affects nerve cells, accelerating their regeneration. The drug does not reduce pressure and does not affect the formation of intraocular fluid. Picamilon helps stabilize visual functions in patients with normal pressure glaucoma. In this type of disease, there is no increase in intraocular pressure, but upon examination of the optic nerve head, changes characteristic of glaucoma (glaucomatous disc excavation) are revealed.
Furosemide
Furosemide is a drug with a pronounced diuretic effect. Reduces the formation of aqueous humor and increases its excretion. Due to the strong and long-lasting diuretic effect, it is used only as an emergency drug for an acute attack of glaucoma with pain. When using the drug, it is necessary to monitor the level of potassium in the blood.