The term “secondary glaucoma” actually defines a group of diseases caused by various pathological conditions and processes. Accordingly, depending on the causes, the nature of the course and symptoms of secondary glaucoma differ somewhat.
The main factors against which a chronic increase or decrease (which is less common) in the pressure of intraocular fluids may develop include:
- infectious and inflammatory processes in the eyes;
- injuries;
- surgical interventions;
- long-term use of certain groups of medications.
The immediate cause of secondary glaucoma is, as a rule, disturbances in the circulation of intraocular fluids.
Note that the division of glaucoma into primary (“true”, independent disease, not associated with other diseases) and secondary is conditional, artificial: in fact, any glaucomatous status is secondary, because has its own reasons and its own pathological background. As for epidemiological data, the share of secondary glaucoma ranges from 1% to 22% (depending on the region) of all ophthalmological pathology. About 30% of glaucoma cases, especially untreated or delayed treated conditions, result in complete blindness; Thus, glaucoma is one of the leading causes of vision loss (along with cataracts). The percentage of enucleation – forced surgical removal of the eyeball – is also quite high; in case of glaucoma, the frequency of such operations reaches 30-40%.
What is secondary glaucoma
A persistent increase in intraocular pressure can occur as a result of various diseases of the visual system, injuries to the eyeball and other conditions. Then they talk about secondary glaucoma, which develops as a complication of other pathologies. The main common pathogenetic link of all diseases that can lead to secondary glaucoma is a violation of the hydrodynamics of the natural intraocular fluid, an increase in its exudation and the impossibility of normal outflow. The degree of increase in IOP and reversibility of changes depends on the severity and duration of exposure to the secondary glaucoma factor.
Diagnosis and treatment of glaucoma
If you suddenly experience one or more of these symptoms, consult a specialist immediately: the sooner you take action, the greater the chance that your vision will be saved.
Treatment of such a serious disease should only be carried out under the supervision of an ophthalmologist. After collecting an anamnesis, to confirm the diagnosis, the doctor will conduct a special examination: examine the condition of the optic nerve head and fundus of the eye, measure the pressure in the chambers of the eyes, examine acuity, refractive ability and visual fields. In addition, he will prescribe the necessary additional studies: ultrasound, tomography, gonioscopy (analysis of the operation and condition of the drainage apparatus), pachymetry (measurement of the thickness of the lens and cornea), etc.
If the diagnosis is confirmed, the doctor will determine how to treat glaucoma and select a set of necessary measures. Depending on the stage of the disease, these may be:
- local medications - eye drops that will improve the functioning of the drainage system and reduce intraocular pressure;
- laser correction – trabeculoplasty. It can also help reduce pressure inside the eyes;
- surgical intervention aimed at restoring the outflow of accumulated fluid;
- some physiotherapeutic methods.
Reasons for the development of the disease
- Any pathology of the organ of vision can affect the processes of formation and removal of intraocular fluid. However, the most common reasons for the development of such a diagnosis as secondary glaucoma are:
- Inflammatory processes. Acute or chronic inflammation of various membranes of the eye can be associated with the action of bacterial, viral, and allergic factors. Most often, keratitis, episcleritis, scleritis and uveitis lead to the development of glaucoma. Uveal ophthalmic hypertension leads to the development of postveal glaucoma, a common complication of uveitis. Inflammation provokes the formation of adhesions and disrupts the normal functioning of the drainage system of the eye, which prevents the outflow of intraocular fluid and increases intraocular pressure.
- Lens pathologies. Changes in the position of the lens due to dislocations, subluxations and other causes of ectopia of the lens become factors in the disturbance of the internal hydrodynamics of the eye, which leads to an increase in IOP. Most often, the development of pathology in this case is associated with the pressure of the affected lens on the anterior chamber of the eye, as well as with the formation of hernias that put pressure on the trabeculae. The lens irritates the cornea, ciliary body, and provokes closure of the angle of the anterior chamber of the eye.
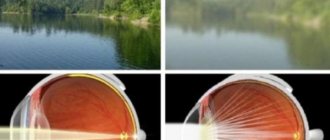
- Cataract. Intraocular pressure increases due to the development of the lens block and narrowing of the anterior chamber of the eye, as a result of which the outflow of aqueous humor is disrupted.
- Injuries. Wounds, bruises, contusions, and burns of the eye increase the production of intraocular fluid, lead to the development of sclerotic changes along the optic canal, disrupt the angle of the anterior chamber and interfere with normal hydrodynamics.
- Degenerative changes. The outflow of intraocular fluid is disrupted due to dystrophic changes in the structures of the organ of vision.
- Vascular diseases. Thrombosis or a persistent increase in pressure in the episcleral veins also leads to the formation of glaucoma.
- Pathological neoplasms. Benign and malignant tumors in the cavity of the eyeball mechanically increase IOP.
Phacotopic glaucoma
This type of glaucoma is caused by luxation of the lens into the anterior chamber or vitreous substance. As a result of penetration of the lens into the anterior chamber, the disease proceeds similarly to angle-closure glaucoma. In this case, you cannot do without removing the lens. At the medical center, everyone can undergo an examination using the most modern diagnostic equipment, and based on the results, receive advice from a highly qualified specialist. The clinic provides consultations to children from 4 years old. We are open seven days a week and work daily from 9 a.m. to 9 p.m. Our specialists will help identify the cause of vision loss and provide competent treatment for identified pathologies.
Main symptoms
Usually the pathological process affects only one eye, and in bilateral cases the damage does not occur symmetrically. The degree of increase in IOP in one eye is greater than in the other. Most often, patient complaints are not specific and are associated with the underlying disease, which leads to the development of glaucoma. Clinical symptoms increase slowly; patients can learn about secondary changes in the processes of formation and removal of intraocular fluid already at an appointment with an ophthalmologist during a comprehensive examination.
The main insidiousness of glaucoma is that in the initial stages of the disease it does not manifest itself in any way and can only be detected during an ophthalmological examination.
Manifestations of pathology may include the following:
- Progressive decrease in visual acuity. The rate at which vision decreases depends on the form of secondary glaucoma and the cause of its development. Usually within a year there is a noticeable deterioration in visual functions up to their complete loss.
- Pain syndrome. Patients may feel pressure inside the eye and increased ophthalmotonus. Sharp pain may be a sign of lens malposition, hemorrhage, or a sudden increase in IOP to high levels.
- Optical illusions. Flashing “floaters” before the eyes, the appearance of rainbow circles when looking at brightly lit objects or a light source can also be signs of the formation of secondary glaucoma.
- Headache. Overstrain of the visual system is accompanied by headache, dizziness, and fatigue when performing various tasks.
Causes
Several conditions can cause the condition to worsen. The disease is closely related to changes in fluid pressure in the eye. In addition, insufficient blood supply to the second pair of cranial nerves is also a condition that can lead to an uncompensated condition.
Causes of uncompensated glaucoma:
- inflammatory pathologies;
- lens shift;
- burns and wounds;
- malignant or benign tumors;
- cataract.
How does secondary glaucoma differ from primary glaucoma?
Secondary glaucoma can also be open-angle or closed-angle, it has the same stages and signs as primary. However, a secondary increase in intraocular pressure has a number of characteristic differences from the primary forms of pathology:
- secondary glaucoma is always a consequence and complication of other diseases;
- most often the damage occurs asymmetrically, the disease affects one eye;
- vision loss occurs quite quickly;
- the processes are reversible if the underlying pathology can be treated.
Symptoms of glaucoma
The symptoms of chronic and acute forms of the disease are different.
So, for chronic
Glaucoma is characterized by:
- weariness, lack of expression of symptoms;
- gradual deterioration of peripheral vision (in later stages - tunnel vision);
- disturbances in light perception, twilight blindness;
- the appearance of halos, light or rainbow circles around light sources;
- blurred vision;
- sometimes – headaches, discomfort in the eye area.
Acute
the form is characterized by:
- sharp, sudden pain in the affected eye;
- headache on the affected side;
- hyperemia of the white of the eye;
- corneal edema;
- lack of pupil reaction to light;
- the sudden appearance of halos when examining objects.
Diagnostic methods
Initially, the ophthalmologist needs to carefully collect all the data from the medical history in order to find out which of the reasons could lead to an increase in intraocular pressure. After this, a series of examinations are most often carried out to confirm the main diagnosis, and during diagnostic procedures, increased intraocular pressure is detected. The main instrumental diagnostic methods that can confirm the formation of a deviation:
- Tonometry. Determination of intraocular pressure is usually carried out in all patients over 40 years of age, so this is how signs of glaucoma are most often detected. The procedure can be carried out using the generally accepted contact method or non-contact - there is pneumotonometry technology, in which special equipment evaluates the deviation of the IOP value from the normal 20-22 mm. Hg Art.
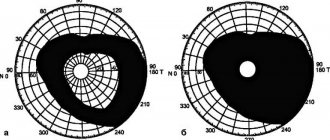
- Tonography. The results of daily measurement of intraocular pressure using computer programs are displayed in the form of a graph. Such a curve allows one to suspect secondary glaucoma. It is characterized by a typical evening rise in IOP with an inverted type of curve.
- Gonioscopy. The parameters of the anterior chamber angle are an important sign for determining the mechanisms of glaucoma development. This method allows you to assess the condition of intraocular structures, determine the decrease in chamber volume, identify angle closure and other disorders.
- Ultrasound. Ultrasound examination allows to identify malignant formations, detect signs of ectopic lens and other organic causes of increased ophthalmotonus.
- Biomicroscopy. The slit lamp brings the visible structures of the eye closer, so it allows you to assess the condition of the cornea, the front surface of the eyeball.
- Refractometry. Assessment of refractive ability does not indicate the development of glaucoma, but may be additional confirmation of existing pathologies of the visual organ. The myopic type of refractive error is characteristic.
- Perimetry. Determination of visual fields also indicates the presence of visual pathology. Most often, peripheral vision will be different in both eyes.
- Optical coherence tomography of the retina and optic nerve shows the integrity of these most important structures of the eye.
- Examination of the fundus by a laser ophthalmic surgeon.
Causes of glaucoma
The causes of glaucoma are numerous. Among them:
- Genetic predisposition. The incidence of glaucoma in newborns is approximately 1 case in 20,000, and 10-15% of cases in the family were diagnosed with the same disease. Often the cause of the disease in this case is hereditary factors.
- Teratogenic factors. This complex of causes is also characteristic of neonatal glaucoma. Glaucoma in an infant can be caused by infectious diseases of the mother during pregnancy, exposure to ionizing radiation, and abuse of tobacco or alcoholic beverages.
- Systemic diseases. Patients with vascular pathologies, endocrinological (for example, diabetes mellitus), metabolic diseases, and thyroid diseases are more prone to the development of glaucoma than their healthy peers.
- Optic neuropathies are lesions of the optic nerve.
- Injuries, bruises of the eyes, complications after surgical interventions.
- Uveitis and other, especially often recurrent, inflammatory eye diseases.
- Complications of untreated cataract.
- Tumor, dystrophic, degenerative eye diseases.
In addition, risk factors for glaucoma include:
- elderly (over 65 years old) age;
- high myopia;
- hypertension;
- local or systemic treatment with hormonal drugs (glucocorticoids).
Glaucoma in an elderly person
Treatment of secondary glaucoma
Since the pathology develops as a complication of the underlying disease, it is necessary to pay special attention to the treatment of primary disorders, which leads to normalization of intraocular pressure.
Main directions of therapy:
- Decrease in IOP. Achieved by instillation of special eye drops - adrenergic blockers, M-cholinomimetics, alpha-2 agonists, prostaglandins.
- Surgical treatment of secondary glaucoma. Often, the prescription of external medications is not enough, so there is a need for surgical interventions - opening the angle of the anterior chamber of the eye, iridectomy, trephination of the cornea, vitrectomy in case of vitreous disorders, lens extraction in the formation of cataracts or lenticular ectopia. Correction of adhesive processes and reconstruction of formed scars are also carried out.
- Coagulation of the retina. The development of retinal detachment and a persistent increase in pressure in the episcleral vessels in some cases requires the use of laser coagulation.
Complications
A number of complications may occur after surgery. The cornea swells and the nerve endings become irritated. This makes the eyes susceptible to various infections.
The patient should be informed of the relative risk of vision loss from surgery.
Patients with end-stage disease often develop inflammatory diseases of the cornea and iris. Perforation of the cornea is possible.
Other complications:
- bleeding;
- high IOP;
- strong pain;
- hypotension;
- corneal decompensation;
- retinal disinsertion.
Disease prevention
There are no specific measures to prevent the disease. If there is an increased risk of developing secondary glaucoma, it is necessary to adhere to the following general preventive measures:
- Be careful with your eyes. It is important to avoid injury, exposure to direct sunlight and other adverse environmental factors.
- Timely contact an ophthalmologist. Any complaints from the visual system require an immediate appointment with a specialist in order to make a diagnosis as early as possible and begin appropriate treatment. Early elimination of the primary disease is the main point in preventing the formation of glaucoma.
- Preventive examinations. Regular visits to an ophthalmologist, even in the absence of complaints, is a good way to early detect even hidden pathologies. Every person needs to measure intraocular pressure regularly, starting at age 40.
- Diet. Sufficient, varied food filled with vitamins and microelements can prevent visual impairment.
- Rest. Work associated with constant visual stress, frequent and prolonged use of the computer, and other unfavorable factors contribute to the development of various pathologies of the visual organ. It is important to provide sufficient rest to the eyes - take breaks every 20-30 minutes and do relaxing exercises.
Tips for recovery after eliminating the primary disease and treating secondary glaucoma include:
- the need to avoid stressful situations and worries;
- good sleep;
- moderate physical activity without sudden changes in body position and lifting heavy objects;
- ban on visiting saunas and steam baths - high temperature provokes surges in intraocular pressure;
- compliance with the rules of visual hygiene. After treatment, it is especially important not to spend a lot of time in front of the monitor. It is necessary to adhere to generally accepted standards of distance between the eyes and the desktop, maintain the physiological position of the back, and maintain posture;
- performing a set of exercises aimed at narrowing the pupil and reducing intraocular pressure.
Secondary glaucoma is a diagnosis for which complete cure cannot be guaranteed. Various risk factors and predisposition to the occurrence of increased intraocular pressure can manifest themselves in the form of pathology at any time. Therefore, it is important to make every effort to prevent visual impairment and associated IOP surges.
Treatment
Treating glaucoma will not restore lost vision, but will only prevent further vision loss. Therefore, the goal is to reduce intraocular pressure either by increasing the drainage of fluid from the eye or by decreasing the amount of fluid produced in the eye. In case of acute angle-closure glaucoma, urgent treatment is required (usually both medication and surgery).
Normal IOP cannot be achieved despite maximal medical therapy. Even if the blood pressure is controlled with medications at the end stage, this is a short-term effect. In the future, fluctuations in IOP will have a detrimental effect on vision.
Treatment begins with medicated eye drops. Commonly prescribed medications include prostaglandins, beta blockers, alpha adrenergic agonists, and miotics.
Use medications as prescribed, otherwise they will worsen damage to the optic nerve. If eye drops alone do not reduce intraocular pressure to the desired level, an oral medication such as a carbonic anhydrase inhibitor may be prescribed to lower eye pressure.
Surgery
At the last stage of the disease, only surgical intervention will help. Preoperative preparation is necessary for a successful treatment outcome.
Before surgery, it is important to normalize blood pressure and undergo blood clotting tests. To reduce inflammation, corticosteroids are prescribed. A few days before surgery, any medications should be stopped.
Before surgery, an anesthetic is instilled into the eyes. A special eye dilator is inserted to prevent the patient from blinking.
Surgeries in the final stage of glaucoma carry more complications. This is due to previous surgical interventions (glaucoma or cataracts).
Surgeries to treat glaucoma include:
- laser - a procedure called laser trabeculoplasty is used to remove blockages in the drainage channels of the eye;
- filtering (amniotic membrane transplantation surgery) - a manipulation called trabeculectomy is used to create an opening in the drainage system that bypasses blocked channels;
- drainage implants – in this procedure, a small tube is inserted into the eye to increase fluid drainage;
- minimally invasive—a tiny tube is placed in the drainage part of the eye to create a permanent opening for fluid to drain.