08/15/2018 Retinal vein thrombosis is a common cause of vision loss in elderly patients. According to statistical data, retinal vein occlusion is the second most common vascular pathology of the retina after diabetic retinopathy. Due to the multifactorial nature of this disease, its treatment to this day remains a challenge even for experienced ophthalmologists.
The mechanism of pathology development
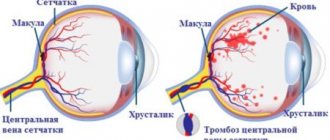
Most often, thrombosis of the central retinal vein and its individual branches is determined in humans. The condition is characterized by a sharp disruption of normal blood flow through the orbital veins and vessels.
If there is a blockage of the central vein, then there is a violation of the outflow of blood. It begins to accumulate in the vessels, which contributes to their deformation. The vascular walls become denser, which leads to slower blood flow. Gradually, a blood clot forms, disrupting normal blood circulation.
Prolonged stagnation of blood leads to the release of its liquid part into the tissues around the vessel. There is an increase in pressure inside the eye, and hemorrhage and swelling may develop. One possible consequence is macular edema, a swelling of the central region of the retina.
In such a case, the condition is dangerous; complete restoration of vision remains in question.
If the blood supply to the eye is disrupted, optic nerve ischemia is often diagnosed, characterized by a sharp decrease in visual function and monocular blindness. The disease occurs more often in men and can lead to complete loss of vision.
Occlusion of the central retinal artery (CRA) and its branches poses a serious danger due to the rapid development of unpleasant symptoms and irreversible consequences.
Symptoms of the disease and diagnosis
The first two stages of the development of this disease occur almost imperceptibly, so it can be quite difficult for a person to detect thrombosis before damage to the vessel.
However, a preventative visit to an ophthalmologist can help prevent the development of the disease. The signs will be clearly visible to an experienced doctor upon examination.
- prethrombosis stage. With the help of an angiographic study, it is possible to detect a slowdown in blood flow in the vessel. Upon examination, dilated, dark and tortuous veins are visible, arteriovenous crossovers become clearer.
- stage of incipient thrombosis. The retinal veins are tense, swelling is visible, the periphery of the fundus is full of pinpoint hemorrhages.
- the stage of complete thrombosis is characterized by a sharp decrease in vision, and this symptom most often brings patients to the doctor. However, the loss of vision is painless. At this stage, new vessels with increased permeability are often formed.
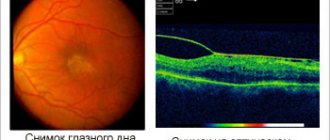
To determine the degree of development of complete thrombosis, fluorescein angiography is performed. To do this, a contrast agent is injected into a vein, which reaches the eye, then the doctor photographs the retinal vessels stained with contrast:
Additionally, retinal vein thrombosis can be diagnosed using optical coherence tomography. The doctor may also order general urine and stool tests, a blood test for sugar, a blood test for clotting, cholesterol, lipids, etc. Diagnosis of the disease may also include measuring blood pressure, an electrocardiogram, as well as consultations with other specialists according to indications (neurologist, therapist, endocrinologist, cardiologist, etc.).
Types of thrombosis
Depending on the degree of damage to the retinal veins, two types of thrombosis are distinguished:
- Ischemic. With this type, most of the vessels in the eyeball are damaged. A serious hemorrhage in the retina is diagnosed, and visual function is seriously reduced. Irreversible consequences may develop if treatment is not started on time.
- Not ischemic. A small area of blood vessels is affected, there is no hemorrhage, visual impairment is minimal and unnoticed by the patient.
In medicine, there is also the concept of complete and incomplete thrombosis of the central vein. The first group includes the ischemic form, the second – non-ischemic. The degree of ischemia directly affects the quality of a person’s vision.
Contraindications to laser use
There are conditions in which ophthalmologists are unanimous in the opinion that surgery is strictly prohibited. Such pathologies include:
- Gliosis (starting from stage III) - as a result of the development of the disease, light-sensitive cells are replaced by structures formed by connective tissue. As a result of such transformations, vision is seriously affected, and the ability to visually perceive the world around us deteriorates.
- Difficult separation of the retina from the vascular network.
- Bleeding inside the eye. Since such changes are temporary, restrictions are also imposed only for a certain period. From the moment the anomaly is eliminated, the patient is allowed to undergo laser coagulation with the permission of the doctor. It is necessary to undergo symptom therapy and eliminate the causes that provoked the disorder.
- Cloudiness of the lens or any other part that affects the quality of vision. Providing timely treatment and eliminating the cloudy spot allows you to remove the restrictions imposed on the operation so that you can proceed with laser treatment without fear.
Reasons for development
This pathological condition develops as a consequence of various health problems of the patient.
There is a division of the most common causes according to the patient’s age:
| Age | Causes |
| Elderly |
|
| Young people |
|
| All age categories |
|
Factors that provoke the development of the disease are also identified:
- Increased body weight.
- Passive lifestyle.
- Alcohol abuse.
- Lack of vitamins in the body.
These factors are not capable of independently triggering the development of thrombosis, but their combination increases the likelihood of its occurrence several times. This disease affects women and men equally.
Causes
Retinal vascular thrombosis is always a consequence of long-standing chronic eye pathology and/or systemic therapeutic diseases.
Risk factors and precursor diseases of retinal thrombosis:
- Atherosclerosis . The deposition of “harmful” lipids in the inner lining (intima) of blood vessels leads to damage to their walls. In response to this, inflammation occurs, which provokes the migration of coagulation factors to the site of damage and increased thrombus formation.
- Diabetes. This disease not only aggravates the course of atherosclerosis, but also contributes to the fragility and pathological tortuosity of blood vessels. There is even the term “diabetic retinopathy” - pathological changes in the vessels of the retina as a result of damage by structurally altered glycosylated (saturated sugars) proteins.
- Arterial hypertension . People with high blood pressure should be especially wary of retinal vascular thrombosis. Due to hypertension, the smallest vessels are damaged, blood supply is disrupted and the formation of blood clots is accelerated.
- Vasculitis - from Latin the term literally translates as “inflammation of blood vessels.” It occurs as an allergic reaction or as a result of connective tissue and blood diseases (hemorrhagic vasculitis, systemic lupus erythematosus, scleroderma, etc.).
- Protruding eyes due to long-term and persistent thyrotoxicosis . Excess thyroid hormones affect the periorbital tissue - it begins to grow. The eyeball literally “sticks out” outward. The vessels cannot keep up with it - they burst and thrombose.
- Tumors . They can grow both from eye tissue and metastasize from other organs. Sometimes a piece of tumor that gets into the vessel blocks its lumen. Read more about neoplasms of the eyelids and eyeball →
Clinical picture
Thrombosis develops gradually. With partial occlusion, a person does not notice any bright signs, the change in vision is minimal. The disease is often diagnosed accidentally during an examination by a doctor.
A sick person may experience:
- Slight decrease in visual function.
- Peripheral hemorrhages.
- Pallor of the arteries.
- Areas of excess blood are difficult to discern.
The ischemic form of thrombosis is characterized by the presence of more pronounced symptoms:
- Massive hemorrhages.
- Severe swelling.
- Excess blood accumulation is very noticeable.
- Noticeable loss of vision.
- Poor reaction of the pupils to light.
- Marked narrowing of the ophthalmic artery.
There are several stages of thrombosis. Each of them is characterized by the development of different symptoms.
Stages:
- The first stage is called prethrombosis. At this stage, venous blood stagnates. The veins become wider, darken, and tortuosity of the vessels appears. The center of the retina becomes swollen. At the first stage, a person may experience blurred vision; this phenomenon is not perceived as a symptom of the disease.
- The second stage is thrombosis. It is characterized by serious circulatory disorders, the occurrence of hemorrhages in the retina and other parts of the eyeball. The boundaries of the optic nerve are poorly visible or not visible at all. Macular edema is present and visual function is severely impaired. The patient notes the presence of a veil before the eyes, loss of visual boundaries. In the absence of adequate treatment, complete or incomplete thrombosis develops, and pathological changes in the retina are noted.
- Postthrombotic retinopathy is the third stage of the disease. The return of a person's vision occurs at a slow pace. Unnatural capillary formations are diagnosed. There are residual hemorrhages in the fundus. During the recovery period, new blood vessels may form in places where they should not be.
Unfortunately, relapse of the disease is possible in the absence of proper treatment.
What complications can occur after laser coagulation?
- The most common consequence of the treatment is swelling of the tissue in the area affected by the laser beam. As a result of the changes that have occurred, vision begins to undergo changes. A swollen cornea causes refractive errors. Objects appear blurry, their contours become blurred. You need to understand that this is a common occurrence. The swelling quickly disappears, and vision returns to its previous levels.
- When using large coagulants, there is a risk of laser energy being transferred to the iris. This often causes the development of an inflammatory process in the visual organ. The result of inflammation can be deformation of the pupil due to the appearance of posterior synechiae on the retina. The defect can only be corrected by repeated surgery.
- Closing the angle of the anterior chamber of the operated eye, which provokes sudden changes in intraocular pressure. The consequences of such a development of events can be the most dire. Ophthalmologists classify pathology as one of the most serious complications.
When using a narrowed laser beam for coagulation, the reaction of the visual organ may be difficult to predict. In some cases, cataracts may develop. The retina itself may change due to hemorrhages occurring on its surface. In this case, detachment can occur in a completely different place.
Incorrect application of coagulants often causes swelling of the macula. This leads to a decrease in the quality of vision and limited vision in the dark. Also among the possible complications due to laser coagulation is ischemia of the optic nerve, a sharp weakening of the ability to see.
Since the risks of side effects cannot be completely excluded from any operation, the patient is recommended to be observed by a doctor regularly after coagulation in accordance with the schedule drawn up for him.
Diagnostics
An experienced ophthalmologist can easily determine the degree of thrombosis. Diagnosis of the disease consists of interviewing the patient and conducting specific examinations. The doctor finds out when changes in visual functions began, what medications the patient is taking, and whether the person has certain diseases.
After conducting a survey and collecting information, studies are prescribed using special techniques:
- Visometry. The method involves studying visual acuity. In the ischemic form of thrombosis, the severity exceeds 0.1, in the non-ischemic form - below this indicator.
- Tonometry. During the study, the pressure in the eyeball is measured. Indicators are taken throughout the day. In a diseased organ, the numbers will be 2-3 mmHg. Art. lower than in a healthy person.
- Perimetry. A method that helps determine the narrowing of the field of vision (scotoma). With thrombosis, a similar phenomenon is observed in the area of the affected retina. The density of the scotoma varies with different amounts of hemorrhage and the presence of ischemic foci.
- Microperimetry. The method is used to determine the reaction of certain parts of the retina to light, which allows you to accurately identify the affected area.
- Biomicroscopy. Allows you to see signs of thrombosis: crushing of the anterior chamber of the eye, a suspension of blood in the vitreous body, lack of a friendly reaction of the pupils when illuminating the diseased eye.
- Optical coherence tomography. Examination using a scanning beam helps determine the structure, size of swelling and features of the course of the disease. The method is used to evaluate the effectiveness of treatment.
- Fluorescein angiography (FA). An effective technique that helps determine the type of thromboembolism, the degree of the pathological process, the affected area, and the period of onset of the disease. The method is often used during the first examination; it helps determine the presence of thrombosis if other methods have not helped.
After confirming the diagnosis, appropriate treatment is prescribed aimed at eliminating the causes and symptoms of thrombosis and restoring visual function.
Self-determination of the disease at an early stage is impossible.
Symptoms are minimal; people often do not pay attention to minor visual impairment. Intense signs are observed during a serious course of the disease, when the person no longer sees well.
A preventive ophthalmological examination is required at least once every 6 months. Regularly visiting a medical specialist will help you not to miss the onset of the disease and select therapy on time.
Symptoms
Often retinal thrombosis occurs without significant symptoms. You should be wary if your vision begins to rapidly deteriorate. Most often, the disease manifests itself in a unilateral form, but it can affect both eyes. Sometimes it progresses rapidly.
In the early stages, you can notice an increased expression of the vascular network in the eye, small pinpoint hemorrhages. Thrombosis at this stage can only be recognized by special studies, angiography, which is why it is so important to undergo regular medical examinations. This is especially true for those who are prone to blood clots.
In later stages, the following symptoms may occur:
- periodic blurred vision;
- dark spots;
- image distortion and veil;
- feeling of sand;
- blinking pain.
Blurred vision
Principles of treatment
Treatment of thrombosis depends on the severity of the disease. For uncomplicated types, the use of medications is sufficient.
Complicated forms of thrombosis will require surgical intervention. The choice of treatment method remains with the doctor.
Conservative treatment
The use of medications helps restore normal blood circulation in the eyeball and visual functions.
The doctor will select medications based on the degree of thrombosis and the patient’s condition. Before treatment, the patient must inform the doctor about the medications he is taking.
Medicines used in therapy:
- Medicines that lower blood pressure. These can be tablets - Nefedipine, Phenigidine. A solution of the drug Dibazol is administered through a vein; Lasix is used for intramuscular administration. Timolol will help reduce pressure in the eyes.
- It is possible to normalize blood flow with the use of fibrinolytic drugs. The drug Plasminogen is injected into the under-eye space for two weeks.
- To avoid relapse of the disease, the patient may be prescribed Acetylsalicylic acid. The intake is carried out under the supervision of a doctor to monitor blood clotting.
- Special hormonal drugs are used to reduce swelling and inflammatory processes. Dexamethasone is often used for a similar purpose - administered under the eyeball, or in the form of droppers.
- If there is pain, analgesics are used.
- Vitamin complexes are required, with the main focus on ascorbic acid and B vitamins.
All medications are prescribed by a doctor. Independent choice of medications can lead to an exacerbation of the process and serious negative consequences.
Surgical methods
Even after successful drug treatment, the patient is recommended to undergo laser coagulation of the retina. The operation is performed under local anesthesia on an outpatient basis. Its duration is no more than half an hour.
It is performed by a qualified ophthalmologist. During surgery, a laser is applied to the blood clot, causing it to dissolve. The result is the restoration of normal blood flow in the vessels of the eyeball.
The operation has some contraindications:
- Retinal disinsertion.
- Presence of cataracts.
- Hemorrhages are diagnosed in the fundus.
- Reduced transparency of the eye media.
Treatment options
Treatment of eye thrombosis can be carried out on an outpatient basis, but it is better to hospitalize the patient. The main goal in the treatment of thrombosis is to restore normal vision, blood supply and nutrition to the eyes. Treatment of pathologies that contribute to thrombus formation is also required.
Medication
The following drugs are used for treatment:
- lowering blood pressure;
- restoring normal blood circulation;
- to eliminate swelling;
- fibrinolytic - to thin the blood and eliminate fibrin from it.
After this, a course of anticoagulants is prescribed to prevent the formation of new blood clots. Most often, thrombosis is treated with the use of corticosteroids against inflammation and swelling. Local medications are also used: eye drops, ointments, creams.
The duration of the course and treatment regimen are prescribed by the attending physician according to individual indications.
Surgical intervention
If medications are not enough to cure or their use is impossible, laser coagulation of the eye may be prescribed. The laser breaks up the blood clot that is blocking the vessel. The operation is quick, painless and bloodless. You need to understand that a laser can eliminate a blood clot, but systematic conservative treatment of the underlying pathology and elimination of provoking factors of thrombosis must be carried out.
ethnoscience
It is not possible to cure eye thrombosis with folk remedies, but you can significantly speed up the healing process and also use them as preventive measures. Herbal decoctions, compresses and applications are used for treatment. For compresses, use black tea, decoctions of plantain, lemon balm, elecampane root, and sage.
The juice of fresh red clover grass helps a lot.
Home remedies can also include massage of the eye area. It prevents blood stagnation and improves its circulation. It is necessary to do eye exercises. They also promote normal blood circulation, train the eye muscles, and can have a significant positive effect on visual acuity.
Possible consequences
In 10% of all cases of vascular thrombosis, complete loss of vision is possible. This complication often occurs as a result of ischemia of the entire central vein and optic nerve atrophy.
Insufficient blood supply leads to other complications after thrombosis:
- Atrophic changes in the nerve.
- Repeated macular edema.
- Secondary glaucoma.
The appearance of a scotoma is possible - an area of the retina of the eyeball with altered or lost visual acuity.
What is laser coagulation of the retina?
Surgery to strengthen the retina helps prevent vision impairment and blindness associated with organ degeneration. Using specialized equipment, the ophthalmic surgeon recreates the integrity of the damaged area. The doctor “seals” problem areas in it, using a laser beam like a microscopic needle.
Indications for the operation:
- Retinal dystrophy. The procedure stops the deterioration of the visual organ, which causes irreversible damage to the photoreceptors.
- Retinoschisis is the accumulation of fluid between the separated layers of the retina.
- Vascular pathologies - surgery is justified for thrombosis of the central vein.
- Diabetic retinopathy is a complication of the eyes in diabetes mellitus with impaired blood circulation in the retina
- Detachment is an anomaly in which the retina detaches from the vascular structure, which disrupts normal nutrition.
Surgery is performed, including to remove certain types of tumors.