Secondary retinopathy is a disease that affects the vessels of the retina and causes disruption of its blood supply. This pathology can develop against the background of various diseases - diabetes, hypertension, atherosclerosis, etc. Let's consider the main causes of this disease and methods of its treatment.
In this article
- Background retinopathy - what is it?
- Hypertensive retinopathy - what is it?
- Atherosclerotic retinopathy - what is it and how is it treated?
- Diabetic retinopathy
- Retinopathy in blood diseases
- Traumatic retinopathy
- Background retinopathy and retinal vascular changes in children
- Diagnostic features
- Prevention
Background retinopathy - what is it?
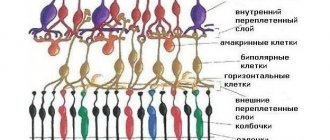
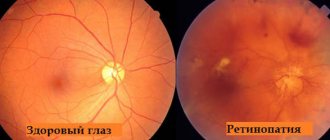
Retinopathy is a series of eye diseases that are characterized by damage to the vessels of the retina of the eye, as a result of which blood and oxygen do not flow to it. This is a rather dangerous disease that can lead to severe vision loss and complete blindness. Often retinopathy is a secondary pathology. It develops against the background of arterial hypertension, atherosclerosis, diabetes mellitus and other diseases. That's why it's called background. Let's look at the main types of retinopathy based on its causes.
How to find out about the disease?
Diagnosis of retinopathy is primarily expressed in a visual examination of the eye for deformations. Ophthalmoscopy is also used to identify pathological changes in the area of the eyeball. Already at this stage, a competent doctor will be able to diagnose retinopathy.
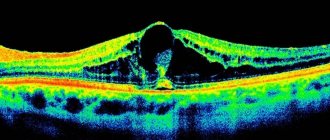
If the presence of the disease is suspected, the patient may be referred for OCT and electrophysiological studies to carefully study the deformities. As prescribed by the ophthalmologist, you should visit a number of other doctors: endocrinologist, cardiologist, therapist and others.
If you have concomitant diseases - diabetes mellitus, atherosclerosis, etc., be sure to visit an ophthalmologist for a preventive examination of the vision apparatus.
To make a diagnosis and combat the disease, comprehensive treatment of both ophthalmological and other pathologies in the patient’s body is required.
Return to contents
Hypertensive retinopathy - what is it?
This form of retinopathy develops as a result of increased blood pressure, which leads to spasms of the arterioles of the fundus and damage to the walls of blood vessels. There are 4 stages of hypertensive retinopathy: Hypertensive angiopathy: dysfunction of the retina, arterioles and venules. They are reversible.
Hypertensive angiosclerosis, which is characterized by damage to the vascular walls with their compaction. The transparency of blood vessels is noticeably reduced.
Hypertensive retinopathy: the formation of pathological foci in the tissues of the inner lining of the eye. Hemorrhages appear, protein fluid is released, and areas of oxygen deprivation are observed in the fundus. Hemophthalmos often develops, in which blood enters the vitreous body. All these processes are accompanied by a decrease in visual acuity and the appearance of dark spots before the eyes. Treatment of arterial hypertension at this stage leads to regression of retinopathy.
Hypertensive neuroretinopathy. At this stage, the optic disc becomes very swollen. Local retinal detachments with exudate are observed. In most cases, this form of retinopathy develops against the background of malignant types of hypertension, renal failure, etc. Emergency assistance is required, as the patient may go blind.
Treatment of hypertensive retinopathy is carried out during laser coagulation of the retina and oxygen barotherapy. But the main therapy is aimed at hypertension. It is necessary to stabilize blood pressure. Its constant increase will lead to the progression of retinopathy.
Secondary type of pathology
A type of retinopathy that occurs together with other diseases in the human body. Often the pathology develops in people who have:
- Eye injury;
- High blood pressure;
- Diabetes type 1 and 2;
- Bruises and fractures of the chest;
- Systemic atherosclerosis;
- Toxicosis;
- Blood diseases.
Let's consider the types of pathologies of the secondary group
Atherosclerotic
It is formed due to a lack of oxygen in the blood vessels. The result is damage to the retina. Character for patients diagnosed with atherosclerosis. Untimely treatment of the disease provokes atrophy of the eye nerve.
Hypertensive
Formed due to deformation of the retina caused by high blood pressure. Due to the compression of small arteries located in the fundus of the eye, rupture and leakage of fluid occurs.
Hypertensive retinopathy is typical for patients suffering from high blood pressure and renal failure. Often affects pregnant women during toxicosis.
| The disease of this form is common and has consequences in the form of a stable deterioration in the ability to clearly perceive objects, up to complete blindness. |
The pathology occurs in 4 stages:
- Agniopathy (beginning of the course of the anomaly);
- Agniosclerosis (damage to the eye vessels);
- Retinopathy (swelling of the retina);
- Neuroretinopathy (nerve swelling, retinal detachment).
Diabetic
A form of retinopathy that affects people with type 1 or type 2 diabetes. Other causes of the abnormality are excess weight, anemia, nephropathy and hypertension. The disease involves loss of elasticity of the blood vessels in the eye and retinal hemorrhage.
The diabetic form of the disease can lead to complete loss of vision if not treated promptly.
Pathology has a three-stage development:
- Background (dilatation of retinal veins);
- Preproliferative (formation of small and medium-sized hemorrhages);
- Proliferative (changes in the vitreous body).
Retinopathy caused by diseases of the circulatory system.
Occurs against the background of various circulatory pathologies:
- Anemia;
- Leukemia;
- Myeloma;
- Bone marrow tumor.
| Each of the subtypes of the disease is characterized by its own clinical picture, but they are all united by the possibility of complete loss of the ability to see. |
Traumatic
It is formed against the background of a strong shaking of the apple of the eye as a result of sudden compression of the chest. Due to compression of the arteries caused by injury, hypoxia forms in the tissues of the retina. From the point of view of ophthalmologists, the pathology looks like a white clouding localized on the side of the affected area or on the other side of the eyeball.
| Often this type of pathology leads to atrophy of the eye nerve. |
Postthrombotic
Occurs due to eye injury, tumors and the development of glaucoma. The pathology manifests itself some time after thrombosis of the vessels that provide blood flow to the retinal area. The result is severe damage to the retina, resulting in significant loss of clear vision.
The postthrombotic form of the pathology is diagnosed in older people with hypertension and coronary artery disease.
Return to contents
Atherosclerotic retinopathy - what is it and how is it treated?
Retinopathy is a vascular disease that can also occur against the background of atherosclerosis, a chronic pathology that affects the arteries and occurs due to lipid metabolism disorders. This disease may not appear on the visual organs for a long time. At the last stage of retinopathy, capillary hemorrhages form, which leads to the deposition of exudate crystals on the walls of blood vessels. Under an ophthalmoscope, the doctor may see severe pallor of the optic disc. There is a decrease in various visual functions.
Treatment of atherosclerotic retinopathy is based on treatment of the underlying pathology, which includes the use of angioprotectors, diuretics, vasodilators and antisclerotic agents. If left untreated, there is a risk of blockage of the artery of the inner lining of the eye and atrophy of the optic nerve, which can lead to significant loss of vision.
Treatment
Drug therapy depends on the extent of the disease. If the doctor was able to diagnose the pathology at an early stage of development, then drug treatment can be used. Moderate and severe stages may require surgery. Treatment methods are determined by the doctor after determining the cause of the disease and the extent of its damage.
Medication
Drug therapy consists of the use of the following medications:
- angioprotector – drugs to protect the walls of blood vessels;
- vasoactive drugs to normalize microcirculation;
- antioxidants - drugs that are responsible for increasing the resistance of blood vessels to the development of hypoxia;
- vitamin complexes.
Such medications are suitable for treating any type of retinopathy. It is worth noting that medications can only be taken as prescribed by a doctor and strictly follow the regimen and prescribed dosage. Self-medication in such cases is impossible.
Surgical
Surgery is prescribed for severe stages of the disease, when drug treatment will not be effective. Two types of surgical intervention are used: cryosurgical coagulation of the retina, vitrectomy.
The latter operation is used to completely or partially remove the vitreous. Any method requires treatment of the disease that caused the development of retinopathy.
Other methods
In addition to basic treatment methods, doctors often prescribe the use of certain procedures. Complex therapy consists of the use of electrophoresis. The procedure has a positive effect on the condition of the eyeball. If the patient is faced with oxygen deficiency, then doctors prescribe the use of hyperbaric oxygenation. The therapy consists of exposure to high pressure oxygen.
Diabetic retinopathy
Retinopathy as a complication of diabetes develops in almost all diabetics. In this case, vascular damage is observed in both types of this disease. The following factors increase your risk of developing diabetic retinopathy:
- long course of pathology;
- complete lack of treatment for diabetes;
- renal pathologies;
- hypertension;
- anemia.
Bad habits (smoking and alcohol abuse) are also factors that provoke retinopathy in diabetes. The disease progresses slowly. For a long time a person may not notice any ophthalmological symptoms. There are 3 clinical stages of diabetic retinopathy:
- diabetic angiopathy - primary and reversible vascular damage;
- diabetic retinopathy: corresponds to atherosclerotic and hypertensive forms of the disease at stages 2 and 3;
- proliferating diabetic retinopathy, which is characterized by the growth of new vessels in the retina.
Newly formed capillaries have fragile walls. Because of this, hemorrhages occur, including in the vitreous body. Hemorrhages subsequently cause scarring and retinal detachment, which is accompanied by severe vision loss. Diabetic retinopathy at different stages manifests itself in the following symptoms:
- persistent decline in visual acuity;
- formation of a veil before the eyes;
- the appearance of floating “flies”;
- deterioration of near vision.
At a later stage, the final loss of visual functions occurs, and the person becomes disabled. How to treat diabetic retinopathy? First of all, you need to monitor your blood sugar levels. You will have to be constantly monitored by an endocrinologist and visit an ophthalmologist twice a year. To improve the condition of the retina, angioprotectors, drugs to activate blood microcirculation and vitamins are prescribed. In case of detachment of the inner membrane of the eye, laser coagulation is performed.
Diabetic retinopathy is often complicated and leads to pathologies such as hemophthalmos, cataracts, and retinal detachment. When scars appear in the vitreous and extensive opacities, vitrectomy is performed - partial or complete removal. But the most serious consequence of diabetic retinopathy is irreversible blindness.
Retinopathy in blood diseases
Blood diseases, including anemia, polycythemia, leukemia, etc., can lead to the development of retinopathy. At the same time, the clinical picture of the disease differs markedly from the course of other forms of this disease. This depends on the background of what kind of blood pathology changes in the retinal vessels began to be observed. Thus, with polycythemia (a benign tumor process), the fundus of the eye becomes bright red, the veins of the retina become especially red. There are signs of vascular thrombosis and papilledema.
With anemia (low content of red blood cells in the blood), the fundus of the eye under an ophthalmoscope is pale, and the vessels are pathologically dilated. Frequent hemorrhages occur under the retina or into the vitreous body, which leads to its/his detachment.
Retinopathy, which occurs against the background of leukemia (blood cancer), is accompanied by the proliferation of blood vessels. They are crimped and fragile, and therefore often burst, causing hemorrhages. The inner lining and optic disc swell.
Treatment of background retinopathy in blood pathologies is based on treatment of the underlying disease and timely laser coagulation. But often the prognosis for the outcome of the disease is unfavorable.
Laser therapy for retinopathy
The use of RIKTA® series devices for the treatment of fundus vascular diseases, diabetic retinopathy, some types of glaucoma, etc. has shown the high efficiency, painlessness and economic feasibility of quantum therapy.
The quantum treatment technique is based on the treatment of retrobulbar fiber and the orbicularis oculi muscle. To use the device on the frontotemporal areas, we recommend a frequency of 50 Hz and a scanning effect not exceeding 2 minutes for each eye, pulse power of the ICL and power of the IR LED 0.25.
This treatment method is carried out under the supervision of an ophthalmologist.
Treatment of the temporal and frontal areas in the treatment of atherosclerotic encephalopathies often leads to a decrease in intraocular pressure and improved vision, which can be explained by an improvement in liquorodynamics, arterial and venous circulation of the eye under the influence of laser therapy.
Traumatic retinopathy
Background retinopathy may result from eye trauma. Signs of hemorrhages are observed immediately. The pathological process develops extremely quickly. If no measures are taken, the risk of optic nerve atrophy increases. Such changes are irreversible. A person loses visual functions. The consequences of such injuries are treated by eliminating hypoxia. It is necessary to restore blood and oxygen supply to the retina. Vitamins and medications are prescribed. The patient is under constant medical supervision.
Preventive actions
First of all, measures to prevent the risk of developing the disease should be aimed at ensuring that the body receives a sufficient amount of vitamins and minerals. To prevent primary type retinopathy, you should avoid stress and chronic fatigue, and also do not ignore frequent headaches.
To reduce the risk of the secondary group, you should pay special attention to the treatment of concomitant diseases and avoid injury to the chest and visual organs.
Proper nutrition, an active lifestyle, weight control and proper rest will help prevent the development of other pathologies that can cause ophthalmic diseases.
Background retinopathy and retinal vascular changes in children
Retinopathy occurs quite often in children. The reasons for the development of pathology are exactly the same as in adults: diabetes, injuries, blood diseases, and, less commonly, atherosclerosis and hypertension. There is also a separate type of this disease - retinopathy of prematurity. It is observed in newborns in the following cases:
- born before 31 weeks;
- body weight up to 1.5 kg;
- after a blood transfusion;
- after saturating the body with oxygen.
Pregnant women who suffer from blood diseases, diabetes, and hypertension should be constantly examined, including by an ophthalmologist. The risk of having a child with retinopathy or developing it later is quite high. If the pregnant woman herself shows signs of this disease, the question of artificial termination of pregnancy arises.
Retinopathy in children often causes other ophthalmopathologies:
- myopia;
- strabismus;
- glaucoma;
- amblyopia.
The retina can also detach, causing severe vision loss. Vascular changes can be detected within 3-4 weeks after the baby is born. The baby is under close supervision of specialists. He is examined by an ophthalmologist every two weeks. Doctors monitor the process of retinal formation. Very often, retinopathy disappears on its own, that is, it regresses. Sometimes the pathology progresses quickly. In such cases, laser coagulation is performed.
Development mechanisms
It is known that the formation of the choroid that nourishes the retina begins at the 4th month of gestation and continues until childbirth. Thus, the birth of a very premature baby automatically means an unformed blood supply system to the retina. However, if previously, for example, a 7-month-old newborn with severe underweight was practically doomed, then since the mid-twentieth century the development of neonatology has sharply increased the survival rate. At the same time, ophthalmologists talk about well-groomed children (the first description of the pathology appeared in the 40s).
It was found that the main reason was the mutually exclusive needs of the unformed organism: on the one hand, for the normal development of the vascular (blood supply) system of the retina, it must be nourished through glycolysis, that is, the oxygen-free breakdown of sugars. But on the other hand, the strategy for life support and nursing of premature babies clearly requires intensive oxygenation in the incubator, which suppresses the processes of glycolysis. As a result, at 3-6 weeks of life (but no later than the 10th), severe, in some cases irreversible, organic changes may begin in the retina, fraught with profound insufficiency or loss of visual functions.
Diagnostic features
Diagnosis is carried out by various specialists, depending on what caused the development of background retinopathy. Of course, ophthalmological examination methods are also prescribed. Among them:
- tonometry: measurement of intraocular pressure;
- angiography: examination of blood vessels;
- laser scanning;
- Ultrasound;
- perimetry - assessment of visual fields;
- ophthalmoscopy - examination of the fundus of the eye.
These are the basic procedures. As an additional method, electroretinography can be prescribed to measure the electrical potential of the retina.
Prevention
To reduce the risk of complications, you must adhere to the following rules:
- monitor your blood sugar levels;
- measure your blood pressure daily;
- do not self-medicate;
- visit the clinic regularly;
- try to eat right;
- spend more time in the fresh air;
- take vitamins;
- do physical exercise.
The diseases listed earlier (atherosclerosis, hypertension, diabetes, etc.) force a person to carefully monitor their health and constantly undergo examinations. If you do not do this, complications may arise, and not only in the eyes.
In order to prevent retinopathy of prematurity, women at risk of premature birth should be hospitalized. If the baby is born prematurely, he will receive prompt medical attention. If retinopathy is detected in a newborn, the child will have to visit an ophthalmologist twice a year until the age of 18, even if the disease has subsided without treatment.