Changes in the retinal vascular pattern
Retinal:
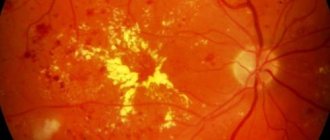
- microaneurysms
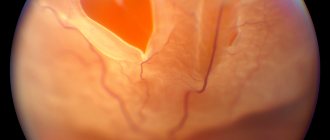
- neovascularization
- perivasculitis
- varicose veins
- vascular sheaths
- vasculitis
Retinopathy:
- NOS
- background NOS
- Coates
- exudative
- hypertensive
Excludes: proliferative vitreoretinopathy with retinal detachment (H33.4)
Angioid stripes of the macula
Drusen (degenerative) macula
Age-related macular degeneration (atrophic) (exudative)
If it is necessary to identify the drug that caused the lesion, use an additional external cause code (class XX).
Retinal degeneration:
- NOS
- lattice
- microcystic
- palisade
- resembling a cobblestone street in appearance
- reticular
Excludes: with retinal tear (H33.3)
Dystrophy:
- retinal (albipunctate) (pigmented) (yolk-like)
- taperetinal
- vitreoretinal
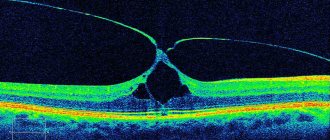
Central serous chorioretinopathy
Detachment of the retinal pigment epithelium
ICD-10 alphabetical indexes
External Causes of Injury - The terms in this section are not medical diagnoses, but rather a description of the circumstances under which the event occurred (Class XX. External Causes of Morbidity and Mortality. Heading Codes V01-Y98).
Medicines and chemicals - table of medicines and chemicals that have caused poisoning or other adverse reactions.
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997 No. 170
The release of the new revision (ICD-11) is planned by WHO in 2022.
Abbreviations and symbols in the International Classification of Diseases, 10th Revision
NOS
- without other instructions.
NEC
— not classified in other categories.
†
— code of the main disease. The main code in the dual coding system contains information about the underlying generalized disease.
*
- optional code. An additional code in the double coding system contains information about the manifestation of the main generalized disease in a separate organ or area of the body.
Diabetic angiopathy is the general name for several pathologies that occur in diabetes.
The disease affects the blood vessels of various organs.
All types of vessels are affected.
In case of mass lesions in small ones, the disease is characterized as microangiopathy, in large ones - macroangiopathy.
The disease is classified into three areas: heart, brain and legs.
What is it and the ICD-10 code
Angiopathy does not have a code according to the ICD-10 international classification, since it is not considered an independent disease. The code is assigned to the disease that led to the development of the pathological condition.
Causes and classification
Angiopathy has several causes. The names in the vessels appear against the background of:
- Traumatic injuries to the chest or cervical spine . Which leads to impaired blood flow and hypoxia.
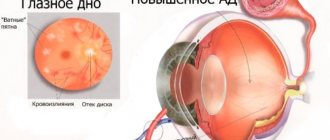
- Arterial hypertension is, simply put, high blood pressure. When blood pressure levels increase, the small capillaries of the retina cannot withstand the load and burst. Hemorrhages occur, which can lead to a decrease in visual acuity, changes in the vessels and their course.
- Arterial hypotension is low blood pressure that occurs against the background of significant dilation of veins and large vessels, leading to the formation of blood clots in the vessels of the retina.
- Cervical osteochondrosis is a disease that leads to impaired blood flow to the brain and increased intracranial pressure.
- Diabetes mellitus is a pathology of the endocrine system, characterized by increased blood sugar levels. In the absence of adequate therapy, diabetes mellitus leads to thickening of the membrane walls and affects the condition of the retinal vascular network.
- Traumatic brain injury - leads to disruption of brain function, increased intracranial pressure, and the development of hypoxia. In this case, angiopathy occurs as a consequence of the injury.
- Pregnancy and childbirth - changes in blood vessels can appear during pregnancy or occur after a difficult birth. In this case, the condition is subject to correction, but only if the cause of the pathology has been established.
- Autoimmune diseases and diseases of the hematopoietic system are nonspecific causes. Against the background of such diseases, changes in the retinal vessels occur quite rarely.
Short description
The most likely signs of angiopathy, in the presence of which you should visit a personal specialist:
Mycelix - for diabetes. Hurry up to get it for free! More details
Among the reasons for the development of angiopathy are the following:
- serious injury to the cervical spine;
- violation of the integrity of the head in the occipital area;
- the presence of high intracranial pressure;
- cervical osteochondrosis;
- the presence of bad habits, for example, such as smoking;
- all kinds of blood diseases;
- old age;
- unfavorable working conditions;
- poisoning of the body with various toxic substances;
- visible disorders of nervous regulation, which are responsible for the tone of the walls of blood vessels;
- high blood pressure;
- individual structural features of the walls of blood vessels.
Expert opinion
Guseva Yulia Alexandrova
Specialized endocrinologist
Ask a Question
Pronounced symptoms of angiopathy, which appeared against the background of high blood pressure, appear only at the last stage and include the so-called veil before the eyes, barely noticeable spots and significant deterioration of vision. If you notice these signs, you should immediately consult a doctor.
Symptoms and signs
Angiopathy has a number of specific signs that a person can notice, but leave without proper attention. Attributing the condition to stress or fatigue.
In most cases the symptoms are as follows
- For the appearance of “flies” in the eyes.
- To reduce visual acuity.
- The appearance of flashes or fog before the eyes.
- For pain or colic in the eyeball area.
- For rapid fatigue of the visual organs.
- For the appearance of pinpoint hemorrhages or burst red blood vessels in the area of proteins.
It is necessary to pay attention to decreased visual acuity, the appearance of floaters or lightning before the eyes. Temporary, but complete or partial loss of vision. When, when getting out of bed or during heavy physical exertion, there is a sharp clouding in the eyes, an acute attack of dizziness.
What ointment helps with stye on the eye and how to use it correctly can be found here.
This indicates that the person has problems with blood circulation in the brain, hypoxia or high intracranial pressure. Against the background of these pathologies, retinal angiopathy develops.
Symptoms may change and occur periodically (only when blood pressure levels increase), but these signs should not be ignored. If alarming symptoms appear, you should consult a doctor as soon as possible.
Clinical picture
Symptoms of diabetic angiopathy of the lower extremities depend on the course of the pathological process:
- Stage I – there are no visual changes, the patient has no complaints, instrumental and laboratory examinations show the development of an atherosclerotic process in the vessels;
- Stage II - the appearance of the so-called intermittent claudication - a specific symptom that is characterized by the need to stop while walking due to severe pain in the legs, which disappears during rest;
- Stage III – pain syndrome appears even in the absence of load on the legs, requiring constant change of position in bed;
- Stage IV - the formation of painless ulcers and dead areas on the skin due to serious disturbances in the trophism of tissues and cells.
Atherosclerosis is one of the manifestations of diabetic angiopathy of the legs.
Accompanying symptoms characteristic of damage to the blood vessels of the legs in diabetes mellitus:
- feeling of burning, tingling, “goosebumps”;
- formation of spider veins;
- pale skin;
- dry skin, peeling, hair loss;
- brittle toenails;
- development of swelling.
Treatment
Therapy is aimed at eliminating the root cause of the pathological condition. If angiopathy occurs against the background of arterial hypertension, the doctor writes a referral to a cardiologist. The doctor prescribes medications that can stabilize blood pressure levels and reduce the risk of bleeding in the retinal vessels and small capillaries.
Diabetic therapy
If angiopathy is associated with diabetes mellitus, then the underlying disease is treated and attempts are made to prevent the development of complications.
So, what medications can an ophthalmologist prescribe:
- vasodilators (Cinnarizine, Vinpocetine, etc.);
- vitamin complexes (narrowly targeted drugs, vitamins for the eyes are used).
- drugs that improve blood microcirculation (mainly drops, such as Taufon).
Drops
List of medications that improve blood microcirculation in the eyeballs:
| Name: | Operating principle: |
| Emoxipin | Available in the form of drops, it is used to treat hemorrhages in the cornea. Has a protective function. By class it is considered an angioprotector. |
| Mildronate | Available in capsule form, it helps improve blood circulation and normalize the functioning of the heart and vascular system. Helps to recover after an illness or heavy physical activity. |
| Trental | Available in tablet form, it improves blood microcirculation and is considered a vasodilator. |
About vitamins for age-related farsightedness, which should be used first, is described here.
As a physical therapy, an ophthalmologist may recommend undergoing a course of magnetic therapy or laser treatment (retinal light).
Diet therapy
If you have diabetes, you must adhere to a special diet, the ingredients of which do not affect blood glucose levels, namely:
- Vegetables.
- Fruits (with a minimum amount of glucose).
- Greenery.
- Lean meats: chicken, beef.
- Sea fish: hake, pollock.
- Low-fat dairy products.
Important! You need to eat in small portions and 5 times a day. The menu should be individually selected according to the amount of proteins, fats and carbohydrates. You cannot provoke fasting, as well as overdo it with food intake, everything should be in moderation.
The following are strictly prohibited for use:
- Animal and vegetable oils.
- Fatty dairy products.
- Sugar, honey, jam and confectionery.
- Smoked, salted and fried dishes.
- Alcohol.
If a person wants to eat chocolate, it can be replaced with sweets with a marmalade or marshmallow base. There are baked goods on sale that contain artificial sweeteners.
Food products for prevention:
- Provisions made from wholemeal flour.
- Cereals: rice, buckwheat, oatmeal.
- Plant foods rich in fiber.
The body takes a long time to process complex carbohydrates. Therefore, the flow of glucose into the bloodstream slows down, and the pancreas has time to produce the necessary amount of insulin for its normal absorption by the body.
The rate of water consumption per day is 1.5 liters. It is recommended to quench your thirst with still mineral water, herbal and fruit teas. For diabetic retinopathy, for prevention purposes, you need to drink pomegranate, plum or fresh cucumber juice.
Course of retinal vascular angiopathy and treatment during pregnancy
During pregnancy, retinal angiopathy develops for several reasons:
- Preeclampsia or late toxicosis.
- Increased blood pressure levels.
- Increased blood sugar levels.
The condition is diagnosed in women in the third trimester and does not require special treatment. Since therapy should be aimed at eliminating the root cause of changes in the vessels and their bed.
Therapy for pregnant women
- decrease in blood pressure levels (pregnant women are prescribed Dopegit, Papazol).
- normalization of kidney function , diuretics of natural origin will help correct the condition: Canephron, Phytolysin, etc.
- adherence to a diet (refusal of sweet, salty, smoked, spicy and unhealthy foods, adherence to certain nutritional rules).
Angiopathy can occur not only during pregnancy, but also after childbirth. In the event that the birth process was severe or protracted and led to hemorrhage in the retina.
A woman may complain about:
- The appearance of fog in the eyes.
- Decreased visual acuity.
- Bright flashes (lightning).
Why flashes like lightning appear in the eyes and what can be done about such a problem can be found at the link.
In this case, consultation with an ophthalmologist is necessary. After discharge from the maternity hospital, you must urgently consult a doctor, he will help correct the condition and avoid possible complications.
Retinal angiopathy is an alarming sign that should not be ignored. If unpleasant symptoms appear, you should consult an ophthalmologist. The doctor will conduct the necessary diagnostic procedures and prescribe adequate treatment.
Factors of occurrence
The main reason for the development of changes in the blood supply to the eye is diabetes mellitus. But there are factors that worsen the course of the disease:
- Alcohol addiction and smoking.
- Errors in taking medications.
- Development of atherosclerosis.
- Genetic predisposition.
- Harmful effects of the external environment on the body.
- Pregnancy.
- Constant increase in blood pressure.
Hypertensive angiopathy
Hypertensive angiopathy is based on the consequences of hypertension. These may be dilated veins, which can be observed in the fundus, branching of the venous bed, pinpoint hemorrhages, which can be observed on the surface of the eyeball.
At an advanced stage of hypertensive angiopathy, changes already occur in the retinal tissues, pinpoint hemorrhages in the eyeball occur frequently, and opacities of the retina are also observed in different places. If the patient’s hypertensive symptoms are eliminated, the fundus of the eye will again acquire a normal, healthy appearance.
Diabetic angiopathy
Diabetic angiopathy affects people diagnosed with diabetes. With this type of angiopathy, small and large vessels are affected. Damage to the walls of blood vessels occurs, and hemostasis is disrupted. Most often, such processes occur in the vessels of the retina, glomerular blood capillaries of the kidneys, in the vessels of the heart, and in the arteries of the lower extremities.
In these cases, thickening of the basement membranes is observed, mucopolysaccharides begin to be deposited on the walls of the vessels, this leads to the narrowing of the lumen of the vessel and ultimately its blockage may occur. These changes lead to deterioration of microcirculation, which, in turn, leads to tissue hypoxia.
Diabetic angiopathy of the lower extremities has its own characteristics. Sensitivity may be lost, polyneuritis of varying degrees may be expressed (burning, numbness of the foot, pain), ulcers may appear, and in the most severe cases, with diabetic angiopathy, gangrene of the toes is possible. But if a person seeks medical help in time, such an outcome is practically excluded.