Papilledema (papilloedema) is a common ophthalmic disease characterized by swelling of the nerve fibers connecting to the eyeball. This pathology is the result of increased intracranial pressure and is usually bilateral in nature, affecting both eyes at once. Gradually, the pathological process leads to the development of retinal vascular changes, becoming chronic. In the absence of timely treatment, complete loss of vision occurs.
What it is
The optic nerve (ON) is a small disc with a diameter of 1 mm, consisting of sensory fibers of the retina that provide color and light perception to the eye. The ON consists of 4 sections and in its normal state has a pale pink tint. When affected, its shade becomes white or gray. The optic nerve head is localized in the intraocular region and penetrates through the bone canal into the brain.
Due to its complex structure, the ON can be subject to various pathological processes. In the voids between the skull and the brain matter, fluid (CSF) accumulates, which in excessive quantities puts strong pressure on the surrounding tissues and causes pinching. As a result, papilledema develops at the junction of the nerve with the eyeball.
Due to increased intracranial pressure, the functionality of the visual apparatus is impaired, the quality of vision deteriorates, up to its loss.
Course of therapy
First, you need to eliminate the cause of the pathology, but you must not forget to maintain adequate nutrition of the nerves in the eyeball. Doctors prescribe special medications for this that improve blood circulation in the vessels, for example, Sermion or Mexidon.
If a tumor is detected in the brain, the patient will undergo surgery to remove it. After such surgery, the course of recovery depends on the severity of the damage caused by the tumor.
If the course of therapy was completed in a timely manner, the swelling on the optic nerve subsides within 3-4 weeks. In case of complications, the duration of treatment can range from 2-3 months to a year and after its completion the patient will have to visit a doctor for examination at least 2 times a year.
The stagnant disc, through which the optic nerve and blood vessels pass, is a very important part of the eyeball, and if it begins to swell, then treatment must be started urgently. The problem is often not independent, but only a consequence of another pathological process that has arisen in the skull, so it is important to find the culprit in time and eliminate it.
Causes
The main reason for the development of papilledema is an increase in intracranial pressure caused by impaired circulation of fluid inside the skull. This disorder may occur against the background of the following diseases:
- brain tumors;
- intracranial bleeding;
- traumatic brain injuries;
- cerebral edema;
- accumulation of pus inside the skull;
- hydrocephalus;
- craniosynostosis;
- improper tissue fusion.
In addition, edema can occur against the background of such pathological processes:
- neuropathy;
- anemia;
- leukemia;
- pulmonary emphysema;
- intracranial infections;
- respiratory failure;
- inflammation of the optic nerve;
- optic neuritis;
- glaucoma.
In some cases, the disease may be caused by kidney failure, lymphoma, or stroke. The exact cause is determined through detailed diagnostics.
At-risk groups
Perineural papilledema can develop at any age. The only category of people who are not susceptible to developing disc edema are newborns. This is explained by the fact that at this age the bones of the skull are still very mobile and an increase in pressure is excluded. People at risk of developing the disease are those who have:
- decreased immunity;
- traumatic brain injuries;
- cancer;
- various ophthalmological diseases;
- hypotension;
- excessive amount of retinol in the body.
The likelihood of developing the disease increases in people who abuse alcohol, tobacco and drugs. Often swelling of the optic nerve develops after poisoning with methanol or quinine (included in some medications).
↑ Neoplasms
↑ Retinal neoplasms
One of the most common malignant neoplasms of the retina is retinoblastoma, which is one of the true malignant tumors. This disease occurs in the first months (20%) or in the first years (55%) of a child’s life.
Retinoblastoma arises from the granular layer of the retina in the form of increasing proliferation. The disease begins unnoticed, but in the coming months the tumor reaches significant sizes, occupying most of the eye cavity. The eye goes blind early. The pupil becomes wide and acquires a yellow glow, which is called “amaurotic cat's eye.”
Ophthalmoscopically, a prominent yellowish-golden tuberous formation is determined. Subsequently, the tumor grows into the optic nerve, sclera, postorbital tissue, brain, and also metastasizes to the liver, lungs, skull bones and leads to death. Usually one eye is affected, and after a while the other.
Treatment
comes down to early removal of the eyeball followed by x-ray and chemotherapy. Recently, photocoagulation of tumor nodes followed by chemotherapy has begun to be used.
Classification
Depending on the extent of the pathological process, papilledema can be of 2 types:
- Unilateral. Only one eye is affected. The symptoms are so mild that even during diagnosis, the doctor may not detect the problem.
- Bilateral. Both eyes are affected, the symptoms are quite pronounced. The progression of the disease occurs over 1-3 days, and sometimes over several hours.
Swelling of the MN disc can occur in acute or chronic form. In the first case, the clinical picture develops quickly and suddenly, symptoms appear within a couple of hours.
In case of repeated relapses, the pathology becomes chronic; it takes about 3 days for the first symptoms to appear.
Symptoms of the disease
During the first 6 months after the onset of edema, the pathological process is asymptomatic. In rare cases, glare spots appear. It is also possible that vision and color perception may temporarily become blurred, and the silhouettes of people and objects become blurred. At the same time, symptoms characteristic of increased intracranial pressure are concerning:
- headaches, the intensity of which occurs during coughing, in the morning or during other stress;
- attacks of nausea that develop into vomiting;
- double vision or flickering in the eyes.
Symptoms of papilledema at the initial stage of development of optic disc disease are diagnosed during an ophthalmological examination, which shows the presence of minor hemorrhages on the retina around the disc. The reaction to light remains unchanged.
The appearance of a congestive optic nerve nipple is noted at the stage when atrophy of local tissues develops. This causes blind spots (scotomas). In advanced cases, the patient stops seeing large sectors. In addition, loss of peripheral vision is possible.
Symptoms
Papilledema develops in several stages:
- First. The boundaries of the optic disc become blurred, its veins dilate, and its arteries narrow. Hyperemia of the optic disc occurs.
- Second. The disc increases significantly in size, hyperemia intensifies, hemorrhages and whitish spots appear.
- Third. The optic disc penetrates the vitreous body, small foci of light yellow color appear.
- Fourth. The disc turns gray.
- Fifth. The optic disc acquires a dirty gray tint and becomes very thick. The vessels penetrate the edematous tissue.
At an early stage of development, symptoms may be absent or mild. The following symptoms may indicate the development of a pathological process:
- severe headaches;
- nausea, vomiting;
- ear noise;
- blurred vision;
- diplopia;
- color vision impairment;
- flickering before the eyes.
Read in a separate article: Retrobulbar optic neuritis: symptoms and treatment
With swelling of the optic disc, a gradual decrease in visual acuity is observed, especially in the central part of the visual field. As the pathology progresses, scotomas begin to appear, and a secondary expansion of the perineural spaces of the optic nerves occurs.
Congestive optic disc
- Theories of pathogenesis
- Ophthalmoscopic picture
- Visual functions
A congestive optic disc was first described in 1866 by A. Graefe (German ophthalmologist A. Graefe, 1828-1870) and called a congestive nipple. Later, instead of the word “nipple”, they began to give preference to another word: “disc”.
Typically, a congestive optic disc occurs when intracranial pressure increases (intracranial hypertension), caused by stenosis or occlusion of the cerebrospinal fluid pathways, or the development of a space-occupying pathological process in the cranial cavity, often a tumor, and often a combination of both. Increased intracranial pressure can also be a consequence of such voluminous pathological processes as brain abscess, infectious granulomas, parasitic cysts, and less often it is caused by other reasons, in particular craniostenosis, which occurs due to premature fusion of cranial sutures.
In most cases, but not always, congestive changes in the optic discs appear on both sides. In the process of development, they go through certain stages, while the severity of the manifestations of optic nerve congestion changes, and as the underlying disease progresses, it increases.
E. Zh. Tron (1968) considered congestive optic disc as a certain form of its lesion, which manifests itself in a characteristic ophthalmoscopic picture, and a dysfunction of the eye. With congestive optic discs, there are usually other clinical manifestations characteristic of intracranial hypertension. The nature, localization and dynamics of development of the main pathological process are of great importance. E. J. Tron emphasized the importance of identifying congestive optic discs in the diagnosis of many neurological and neurosurgical diseases, noting that congestive disc “is the most common ocular symptom in brain tumors.”
Intracranial hypertension as the main cause of congestive optic discs and their complications
Intracranial hypertension is usually characterized by first periodic and then constant, sometimes exacerbating, diffuse, bursting headache. Against this background, with increased headaches (hypertensive crises), cerebral vomiting, a periodic feeling of fog before the eyes, disorders of vestibular functions, bilateral damage to the abducens nerves, pronounced autonomic reactions, and increased mental exhaustion are possible. workload. Against this background, in cases where the patient is not provided with adequate assistance, Bruns syndrome may develop.
The cause of intracranial hypertension is usually voluminous pathological processes that cause disorders of liquorodynamics - intracranial tumors, cysts, abscesses, infectious granulomas, parasitic cysts, etc. In this regard, the identification of congestive optic discs requires a detailed, targeted examination of the patient in order to clarify the pathological process that caused their development. Most often, such a process is an intracranial neoplasm, less often other voluminous pathological foci, craniostenosis or inflammatory diseases occurring as meningitis or meningoencephalitis, rarely arachnoiditis, causing disturbances in liquorodynamics.
Sometimes there are clinical observations in which congestive optic discs are the main clinical manifestation. First of all, these include the syndrome of primary benign intracranial hypertension.
Theories of pathogenesis
The pathogenesis of congestive optic discs is still considered controversial. The first hypothesis was proposed in 1866 by A. Graefe (A. Graefe, 1828-1870). He believed that the cause of congestion in the fundus was a violation of the outflow of venous blood from the eyeball through the central retinal vein into the cavernous sinus. Infiltration of the optic nerve tissue and its disc was explained by congestion in the central retinal vein. However, this version was later disputed, since venous outflow from the eyeball is possible not only through the central vein, but also through anastomoses between the ophthalmic veins and the veins of the face, as well as through the ethmoidal venous plexus; moreover, thrombosis of the central retinal vein is characterized by a different ophthalmoscopic picture.
In this regard, T. Leber (German ophthalmologist Leber Th., 1840-1917) in 1877 suggested that ophthalmoscopic changes, interpreted as manifestations of stagnation, are caused by inflammation of the optic nerve. He proposed using the terms “papillitis” or “congestive neuritis” in such cases; he was supported by an authoritative figure at the beginning of the 20th century. ophthalmologist A. Elschnig, who agreed that “a congestive nipple is nothing more than a special form of inflammation.” He recognized such inflammation as secondary, usually provoked by an inflammatory focus in the orbit or in the cranial cavity.
Since the essentially different concepts of “congestive nipple” and “neuritis” began to be perceived as one and the same phenomenon detected by ophthalmoscopy, the English physiologist and ophthalmologist G. Parson in 1908, instead of the term congestive nipple, introduced the term “nipple edema” or “papilloedema” "("cerebral edema") . He used the term “neuritis” in cases where there was a relatively small protrusion of the optic nerve head in combination with severe visual impairment. The need to differentiate papilledema from inflammation, i.e. from neuritis, was obvious, therefore Parson’s proposal to introduce a new term into practice was supported by many physiologists and clinicians of that period, in particular K. Wilbrand and A. Zenger, authors of the first monograph on neuro-ophthalmology “Neurology of the Eye” (1912-1913). He readily used this term already in the middle of the 20th century. and the famous Russian neuro-ophthalmologist I.I. Merkulov.
V. Hippel (Hippel W., 1923) significant clarity to the differentiation between congestion and inflammation of the optic disc He emphasized that a congestive optic nerve is not an inflammation of the optic nerve, but something completely different. The scientist noted that congestive manifestations in the optic nerve papilla usually occur in patients with brain tumors and other diseases manifested by increased intracranial pressure. Then he drew attention to the fact that, in contrast to inflammatory damage to the optic nerve, when its nipple (disc) is congested, normal or close to normal visual acuity can be maintained for a long time.
Thus, the question of the pathogenesis of congestive optic discs has been the subject of debate for a long time and until now cannot be considered completely resolved. Many theories have faded into oblivion. And at present, perhaps, only two of them are recognized, which today can be considered as the main ones -
- transport theory of Schmidt-Manz, recognized as the most probable by R. Bing and R. Brückner (1959), and
- Behr's retention theory (German ophthalmologist Behr S., born in 1876), which was considered preferable by E. Zh. Tron (1968) and I. I. Merkulov (1979).
According to the transport theory of the development of the congestive optic disc, the subarachnoid space of the intraorbital part of the optic nerve communicates with the subarachnoid space of the cranial cavity, since it is formed by the meninges penetrating into the orbital cavity along with the optic nerve, consisting of brain tissue.
With an increase in intracranial pressure, cerebrospinal fluid penetrates into the subarachnoid space of the optic nerve, accumulates in it and gradually forms a club-shaped expansion, compressing its fibers. In the nerve, compression occurs primarily on those fibers that make up its outer sections. At the same time, difficulty in blood circulation occurs in the optic nerve. All this provokes swelling of this nerve and its disc. The version is attractive. However, the presence of communication between the intershell spaces in the cranial cavity and the retrobulbar intraocular part of the optic nerve turned out to be not indisputable, since experimental work appeared that refuted the connection between them.
The retention theory of Bohr (1912) is based on the idea that watery tissue fluid, formed mainly in the ciliary body, normally flows along the optic nerve into its intracranial part, and then into the subarachnoid space. According to this theory, a congestive optic disc with increased intracranial pressure is caused by a delay in the outflow of tissue fluid along the optic nerve into the cranial cavity. This is due to the fact that with an increase in intracranial pressure, difficulty arises, and then a blockade of the movement of tissue fluid, as Behr believed, mainly at the point where the optic nerve exits through the bone opening (optic canal) into the cranial cavity.
The fibrous (intracranial) part of the optic canal is formed by a fold of the dura mater stretched between the anterior inclined process and the upper edge of the opening of the optic canal. This fold partially covers the optic nerve from above at its exit from the bone canal into the cranial cavity. With increased intracranial pressure, the fold of the dura mater is pressed against the optic nerve, and the nerve itself is pressed against the underlying bone structures. As a result, the tissue fluid of the eye flowing along the nerve is retained in its orbital and intraocular parts, including in the optic nerve head. The fibers of the optic nerve are gradually compressed by it along the entire circumference of the nerve and, in parallel, its swelling develops and progresses, primarily the swelling of the bundles of its fibers located along the periphery. Over time, usually after weeks, sometimes many months, the pupillo-macular bundle, which occupies a central position at this level of the optic nerve, is also involved in the process.
In the optic nerve head, the pupillomacular bundle is located in its temporal part, and this explains why, with a congestive optic nerve head, swelling of the temporal edge of the disc usually develops later than its other parts. Swelling of the optic disc appears more often, starting from its upper edge. The relatively late involvement of the pupillo-macular bundle in the pathological process makes it possible to understand the often long-term preservation of visual acuity in a patient with congestion in the fundus.
In 1935, Baer wrote that in the initial stage of congestive optic disc tissue fluid accumulates between the bundles of its fibers, which leads to the development of intrafascicular edema of the optic nerve. Subsequently, it appears in the nerve fibers themselves, spreads along the nerve, penetrating into the surrounding subpial space. Baer assumed that the spread of edema of the optic nerve occurs from its disc to the bone canal. Having reached the optic nerve canal, the swelling of the disc breaks off at this level.
Most authors who conducted morphological studies of the optic nerve with congestion in its disc (Hippel E., 1923; Schick F., Bruckner A., 1932; etc.) came to the conclusion that swelling of the optic nerve is especially pronounced in the perivascular spaces of the branches the central vessels of the retina (arteries and veins), as well as in the optic nerve head and its proximal parts, in which these vessels pass.
I. I. Merkulov (1979) adhered to the retention theory of the development of congestion in the fundus and at the same time recognized that disc edema, or congestive disc of the optic nerve, is the result of impaired circulation of aqueous tissue fluid in its subpial space and in the perineural fissures, as well as microcirculation disorders in the optic nerve. He also noted that the pressure of tissue fluid, which accumulates in case of disruption of its outflow in the subpial space, on the optic nerve occurs evenly, in accordance with Pascal’s law, according to which pressure on any part of the surface of the fluid is transmitted in all directions with the same force.
E. J. Tron (1968) recognized the great advantage of Beer’s retention theory that it explains not only the pathogenesis, but also a number of clinical features of the state of visual functions with congestive optic nerve head. At the same time, he noted that not one of the existing theories, including retention, cannot be considered conclusively proven. He believed that, by studying the pathogenesis of congestive optic discs, it is necessary to clarify the extent of the spread of edema along the optic nerve and find out whether the swelling of the nerve, as Behr argued, does not extend beyond its intraorbital segment, ending at the level of the bone optic foramen. In addition, E.Zh. Tron noted that from the standpoint of this theory, such facts as unilateral congestion of the optic disc, different frequencies of optic disc congestion in intracranial volumetric pathological processes of different localization, as well as the possible absence of congestion in the optic discs in some cases of brain tumors cannot be satisfactorily explained accompanied by an increase in CSF pressure.
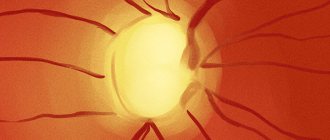
Ophthalmoscopic picture
The ophthalmoscopic picture of congestive optic disc depends on the stage of the process. According to E. J. Tron, there are five of them:
- initial stagnant disk
- pronounced congestive disc
- pronounced stagnant disc
- stagnant disc in the atrophy stage;
- optic disc atrophy after congestion.
These stages do not have a clear demarcation and gradually transform into each other. The development of congestive optic discs and their progression largely depends on the duration and severity of intracranial hypertension, and due to their certain variability, the dynamics of ophthalmoscopic changes in the fundus are not identical. However, such identification of the stages of development of a congestive optic disc still has practical meaning, since it contributes to the characterization of the patient’s set of ophthalmoscopic signs and creates opportunities for judgments about the severity of intracranial pressure and, therefore, allows one to predict the further dynamics of the clinical picture.
In the early stage of development of a congestive disc (initial congestive optic disc), venous hyperemia in the disc area and blurred boundaries are characteristic. A slight uneven swelling of its tissue gradually develops along the edge of the disc, and a slight protrusion of the disc appears. At first, the swelling does not cover the entire circumference of the disc, but only its individual parts, most often these are its upper and lower edges and the place where large vessels pass through the edge of the disc. The swelling then spreads to the inner (nasal) edge of the disc. For the longest time, and this is recognized by almost all authors, the outer (temporal) edge of the optic disc remains free from edema. In the area of marginal edema of the disc, its tissue acquires a whitish tint, due to the fact that the accumulation of tissue fluid between the nerve fibers at the edge of the disc to some extent conceals its usual color. In addition, at the site of marginal disc edema, radial striations can be noted, caused by the expansion of nerve fibers by edematous fluid. The venous vessels of the fundus in the initial stage of the congestive disc gradually expand, while the caliber of the arteries remains the same.
Subsequently, the marginal edema of the optic disc increases and gradually spreads throughout the entire disc; last of all, the disc recess is filled with edematous tissue (physiological excavation). Before filling it, you can still see the central vessels of the retina at the bottom of the recess for some time. With increasing swelling of the optic nerve tissue, there is an increase in the size of the disc, its diameter, as well as the degree of protrusion of the disc above the level of the surrounding retina towards the vitreous body. The veins become not only dilated, but also tortuous, the arteries narrow somewhat. With the spread of edema to the physiological excavation of the disc, according to E. Zh. Tron, the stage of the initial congestive optic disc can be considered completed.
With pronounced congestion of the optic disc, attention is drawn to more significant hyperemia and enlargement of the disc, as well as an increase in blurring of its boundaries. Swelling of the disc borders is observed along its entire circumference, while the disc is already significantly protruding towards the vitreous body. The veins are wide and tortuous. The underlying edematous retinal tissue in places overlaps fragments of blood vessels. The edematous disc tissue becomes cloudy. Hemorrhages and white spots may appear in the fundus. Hemorrhages can be multiple, varying in size, are more often linear in shape and are located mainly at the edges of the disc, as well as in the adjacent parts of the retina. They are usually recognized as a consequence of obstruction of blood circulation in the veins of the disc and rupture of small venous vessels. There is an opinion that toxic factors (I. I. Merkulov, 1979) or concomitant manifestations of aseptic inflammation are also possible in the origin of hemorrhages. However, even with severe congestion of the optic nerve, there may not be hemorrhages in the fundus for a long time. The appearance of white spots of different sizes and shapes in the edematous disc tissue is usually explained by the degenerative degeneration of areas of nervous tissue. They occur in the congestive optic disc less often than hemorrhages, and when they occur, they are usually combined with foci of hemorrhages.
Severe congestive discs are usually characterized by the same ophthalmoscopic signs detected during ophthalmoscopy, but the degree of their severity by this time is much greater. Due to the intense swelling of the disc, it will withstand significantly and prolapse into the adjacent vitreous body. This distance can be up to 2.5 mm. Particularly noteworthy is the increase in the diameter of the disc; it is sometimes so significant that during ophthalmoscopy the disc does not fit into the viewing area of the fundus even after medicinal dilation of the pupil, and then the disc has to be examined in parts. The hyperemia of the disc at this stage of its stagnation becomes so pronounced that upon examination, its almost complete merging in color with the surrounding retina is noted. In this case, the vessels can be almost completely immersed in the edematous tissue of the disc and become visible only before they leave its limits.
The entire surface of the disc is dotted with small and large hemorrhages and white spots. Multiple foci of hemorrhage are often present in the retina. Then they are located mainly around the congestive optic disc, some of them merge with each other, forming blood “puddles”. Sometimes, with severe stagnation of the optic nerve head, foci of hemorrhage can occur between the optic nerve head and the macular zone; they may also appear at a distance from the disc. In such cases (in 3-5%), they can form small white lesions in the form of a half-star or star, known as pseudoalbuminuric (or stellar) retinitis, which can extend to the macula. Similar changes in the retina are observed in the macular zone in hypertension and kidney diseases complicated by arterial hypertension. A rapid decrease in visual acuity with congestive optic discs usually occurs during their transition from the stage of pronounced congestive discs to the stage of atrophy.
Long-term signs of pronounced optic disc congestion gradually progress to the next stage of its development, known as congestive disc atrophy . At this stage, attention is drawn to the fact that the hyperemic stagnant disc is covered with a gray coating, while the severity of the degree of disc edema gradually decreases. If during the period of culmination of a stagnant disc, foci of hemorrhage and white spots were detected in it, then during the transition of a stagnant disc to its atrophy, they gradually resolve and disappear, while the disc gradually turns pale. As a result, it acquires a white color with a dirty tint, its boundaries remain unclear, its size decreases, but remains somewhat larger than normal. In some places, a small, uneven protrusion of the optic nerve head remains for some time. At this stage of the process, his veins are still dilated and tortuous, his arteries are narrowed.
Subsequently, the consequences of congestion in the disc finally disappear, and the typical final phase of the congestive disc is formed - the stage of secondary atrophy of the optic disc after stagnation. It is characterized by pallor of the disc, some irregularity of its outline and unclear boundaries; the veins and arteries of the disc become narrow. Signs of this stage of development of a congestive optic disc can persist for a very long time, sometimes a year or more. However, over time, its boundaries become increasingly clear, the color is white (the color of foil or muscle tendon), and the size of the disc reaches its original (normal) size. At this stage, secondary atrophy of the optic disc after stagnation is difficult, and sometimes impossible, to distinguish from its primary atrophy, if only ophthalmoscopic data are used. Clarification of the origin of optic disc atrophy in such cases is possible only taking into account carefully collected anamnestic data, as well as comparison of the existing condition of the fundus with the results of previously performed ophthalmoscopy and other methods of neuro-ophthalmological and neurological examination.
If the cause of the congestive disc is eliminated during the treatment process, but before that, secondary atrophy of the optic disc has already developed after congestion, then in this case the disappearance of the remaining ophthalmoscopic signs of congestion in the fundus and the development of an ophthalmoscopic picture simulating the condition characteristic of simple atrophy of the optic disc, happens faster. Congestive optic disc usually develops simultaneously on both sides, but exceptions to this rule are possible.
Unilateral congestive optic disc is possible with an orbital tumor, traumatic damage to intraorbital tissues, and in some cases, supratentorial localized voluminous pathological processes (tumor, abscess, etc.). A unilateral congestive disc is also characteristic of Fester Kennedy syndrome, in which primary optic disc atrophy is detected first on one side (usually on the side of the pathological focus), and then signs of a congestive disc appear on the other side. This syndrome is more common with intracranial tumors growing in the middle cranial fossa, sometimes with tumors of the infero-posterior parts of the frontal lobe.
Thus, the identification of one or another stage of congestive optic disc in a patient often does not in itself make it possible to judge the duration and outcome of the main pathological process. The rate of formation and change of stages of congestive optic disc usually corresponds to the pace of development and localization of the cause that caused it. If a patient develops occlusive hydrocephalus, manifestations of intracranial hypertension, including the development of congestive optic discs, can develop rapidly. Sometimes the manifestations of the initial congestive disc transform into pronounced congestive disc within 1-2 weeks. However, the ophthalmoscopic picture of a congestive optic disc can stabilize for several months, and in some cases, regress, as happens, for example, with primary benign intracranial hypertension.
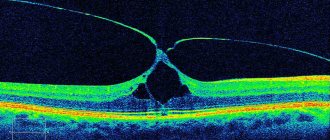
Visual functions
Visual acuity and visual fields during the development of congestive optic discs in typical cases can remain unchanged for some time, sometimes for a long time (correspond to the premorbid state). The first clinical sign of papilledema development is usually an enlargement of the physiological scotoma, a blind spot that is most easily detected by campimetry. Swelling of the optic disc tissue spreads to the adjacent parts of the retina and affects its functions. The increase in signs of stagnation and the size of the disc leads to a further increase in the size of the blind spot.
In 1953-55. S. N. Fedorov, using campimetry data and strictly standardized photographs of the fundus of the eye in patients with intracranial tumors, in the process of completing his Ph.D. thesis, showed that an increase in the size of the blind spot outstrips the appearance and subsequent development of ophthalmoscopic signs of congestive optic discs, primarily changes in their diameter . If, in a patient with congestive optic discs, the tumor was removed before their atrophy occurred, then the decrease in the blind spot began to decrease before the ophthalmoscopic picture, indicating a tendency towards normalization of the discs.
The first visual disturbances subjectively perceived by patients with congestive optic discs are usually short-term episodic sensations of fog before the eyes. These short-term but significant visual disturbances usually occur during periods of physical stress or being in a bending position. K. Baer believed that such periodic blurring of vision could be explained by a deterioration in the conductivity of nerve fibers in the area of the optic nerve canal as a result of a temporary increase in intracranial pressure in the patient.
The boundaries of the visual fields with congestive optic disc can remain within normal limits for a long time. However, after months, sometimes after a year or more, a narrowing of the visual fields of a concentric type, revealed by perimetry, appears and gradually increases, with their boundaries first narrowing into colors, and then into white light, in most cases evenly along all meridians.
As the severity of optic disc atrophy increases, a decrease in visual acuity appears and increases quite quickly. Sometimes the loss of vision can develop catastrophically: with rapidly progressing atrophy of the optic nerves, blindness may occur after 2-3 weeks.
However, if a patient with congestive optic discs undergoes a radical neurosurgical operation or palliative intervention aimed at reducing intracranial pressure, congestion in the fundus begins to regress after a few weeks and this process continues for 2-3 months, and sometimes longer. The development of signs of regression of congestion in the optic nerve head is usually preceded by a gradual decrease in the size of the blind spot. Preservation of vision is more likely if neurosurgical intervention was performed before the appearance of ophthalmoscopic signs of secondary optic disc atrophy. In such cases, one can hope for the possibility of normalization of the condition of the fundus and almost complete or complete restoration of visual function.
Diagnostic methods
The symptoms of optic edema are similar to the clinical picture of many other ophthalmological diseases. Therefore, it is impossible to make an accurate diagnosis based on patient complaints alone. To determine the disease and identify the characteristics of the pathological process, various instrumental studies are required:
- Ophthalmoscopy. The fundus is examined.
- Biomicroscopy. Using a microscope, eye structures are studied.
- Perimetry. The visual fields are assessed.
- Tonometry. Intraocular pressure is measured.
To obtain a more detailed picture of the course of the disease, an ultrasound of the eye, CT or MRI can be performed. For a more detailed examination of the nerve fibers during diagnosis, the pupils can be dilated using special drops. If necessary, other diagnostic measures are prescribed. In some cases, a lumbar puncture is performed to collect cerebrospinal fluid. This diagnostic method allows you to identify signs of the inflammatory process. Reviews about its implementation are usually positive.
Treatment
Treatment tactics for disc edema depend on the cause of the disease and the severity of its course. The therapy is based on eliminating the root cause, since if the underlying disease is eliminated, then the swelling will go away much faster. Measures are also taken to reduce the level of intracranial pressure.
Drug therapy
To eliminate swelling of the optic nerve, medications from the following groups are prescribed:
- Corticosteroids: Prednisolone, Cortisone. Stops inflammatory processes.
- Diuretics: Furosemide, Acetazolamide. Restores the balance of cerebrospinal fluid and promotes weight loss.
- Antibiotics: Amoxiclav, Amoxicillin. Eliminate bacterial processes.
- Antihistamines: Suprastin, Claritin. Allergic processes are stopped.
Depending on what caused the swelling of the optic disc, other medications may be prescribed. Drug therapy helps to cope with the problem in the initial stages of the development of pathology.
The duration of treatment is determined by the doctor individually; self-medication is unacceptable.
Surgical intervention
In advanced cases, when conservative therapy is powerless, there is a need for surgery. The most common procedure is fenestration of the eye disc, during which excess cerebrospinal fluid is eliminated by creating small holes in the structure of the disc. Reviews about this surgical intervention are positive.
Swelling can also be eliminated with the help of lumboperitoneal shunting, aimed at removing excess fluid and normalizing pressure. The essence of this surgical intervention is to connect the spinal cord to the abdominal cavity using a system of shunts. Typically, such an operation is performed if the disease was caused by a tumor.
Methods for treating edema
The basis for the treatment of congestive optic disc consists of procedures whose action is aimed at eliminating the root cause of the development of the pathological process. In particular, techniques are used to eliminate increased intracranial pressure. For this purpose, the treatment regimen for papilledema is often supplemented with surgical intervention.
Surgeries are performed if cerebral palsy is caused by brain tumors of any nature. During the procedure, overgrown tissue is excised. Also, as part of surgery, a hole is sometimes drilled in the skull, which temporarily normalizes the pressure.
For swelling of the optic nerve, corticosteroids are indicated: Methylprednisolone or Prednisolone. To stop the pathological process, hormonal drugs are used in the form of tablets or solutions.
To eliminate stagnation of cerebrospinal fluid inside the skull, diuretics are prescribed: Furosemide, Acetazolamide and others. These drugs are also used as tablets or as an intravenous solution. With the help of diuretic drugs, the removal of excess fluid from the body is accelerated, due to which swelling disappears.
In case of infection of brain tissue, broad- or narrow-spectrum antibacterial drugs are used. In addition to these medications, antihistamines are used to eliminate swelling.
In case of congestive optic disc disease, dietary nutrition aimed at reducing body weight is recommended. This approach often helps reduce intracranial pressure and provide relief to the patient.
In advanced cases, fenestration of the optic nerve sheath (shunting) is performed. In this procedure, the surgeon creates holes in the tissue surrounding the disc through which excess fluid can drain. Several shunts are also installed to divert cerebrospinal fluid from the spinal cord towards the abdominal cavity.
This type of surgery is mainly used for benign tumors in the skull.
Prevention
To avoid the development of papilledema, it is necessary to lead a healthy lifestyle and observe the following preventive measures:
- avoid head injuries;
- strengthen immunity;
- normalize body weight;
- stop drinking alcohol and smoking;
- take medications only as prescribed by a doctor;
- avoid visual, mental and physical stress;
- observe the rules of personal hygiene;
- promptly treat emerging diseases;
- undergo regular preventive medical examinations.
When the first signs of a pathological process appear, you should immediately contact an ophthalmologist.
Diagnostics
If signs of congestive optic disc disease occur, you should consult an ophthalmologist. Without timely treatment, the pathological process causes blindness in one or both eyes.
Diagnosis of optic nerve disc disease is carried out using an ophthalmoscope.
The device allows you to examine the condition of the fundus and identify swollen tissue. Before the procedure begins, special drops are injected into the organs of vision to dilate the pupil. After this, a directed beam of light is applied to the retina of the eye.
To differentiate congestive optic disc from brain diseases, MRI and CT are used. If necessary, a cerebrospinal fluid examination is performed to determine the causes of the development of spinal disc disease. In some cases, a biopsy of brain tissue is used.
Forecast
If the patient consults a doctor on time, the prognosis is favorable in most cases. The outcome largely depends on the underlying cause of the disease. If papilledema occurs as a result of an oncological process, then the chance of a complete recovery is minimal. To avoid complications, even after successful completion of therapy, you should regularly visit a specialist. During the first month, this should be done weekly, and then once every 3 months.
If the disease is left to chance, the prognosis is extremely unfavorable and there is a high risk of going blind.
Author of the article: Kvasha Anastasia Pavlovna, specialist for the website glazalik.ru Share your experience and opinion in the comments.