In some cases, a clinical examination by an ophthalmologist may reveal optic nerve disorders. During the diagnostic process, the doctor assesses the size, shape, depth, paying special attention to the parameters of the temporal edge. Usually the latter looks undermined and can be steep or flat. In some cases, excavation of the optic disc is detected.
In the course of long-term scientific research, it was revealed that the physiological type of the phenomenon is not detected in a quarter of the entire population, especially for people over 40 years of age. In the rest of the patients, this is observed in varying degrees of manifestation.
Structure
Functions
Symptoms
Treatment
Structure
In other words, we are talking about a decolorized area in the very center of the optic nerve. The depression is distinguished by the absence of nerve cells in its structure.
During the diagnostic process (using direct ophthalmoscopy), the specialist determines the area where the blood vessels bend - they cross the optic nerve head. In the case of an alternative diagnosis (reverse ophthalmoscopy), EDZN appears as a pale area. This shade is explained by the presence of a thin lattice plate and a lack of glial cells.
The diametrical indicator of the recess depends on the size of the disc. Thus, with an insignificant diameter of the latter, the pale area will also be small, since there is a high density of nerve fibers emerging from the eyeball. If the diameter of the disc is large, the fibers lose their tone - the depression will increase.
Excavation of the optic disc - what is it?
An excavation of the optic disc (EDN) is a depression of various shapes and sizes in its center. This formation may be natural or the result of pathological changes.
Physiological excavation, which is considered normal, is of three types:
- Small depression in the center
- Expanded recess in the center
- Depression with temporal retraction.
Natural excavation is observed in most healthy people - approximately 75%.
The relationship between the size of the disc and the diameter of the excavation is in most cases genetically predetermined. In its normal state, the temporal edge looks undermined, steep or flat. Its shape is usually oval or round. The shape of the optic nerve is considered incorrect, in which it narrows in the nasal region and widens on the temporal side.
Pathological excavation is called glaucomatous. The cause of this pathology is increased intraocular pressure.
Symptoms
In some cases, even a glaucomatous phenomenon is discovered completely by accident, since the patient does not complain about anything. However, the development of a pathological process (most often we are talking about glaucoma) may be indicated by the following unpleasant manifestations:
- feeling of heaviness in the eye area;
- unexpressed soreness;
- increased visual fatigue;
- double vision;
- limited field of vision;
- decreased vision (especially in poor lighting);
- visualization of a rainbow circle at the moment of eye contact with light;
- feeling of excessive moisture in the organ of vision.
As the pathological process develops, a person ceases to navigate in space due to limited visual fields. In advanced cases, the patient feels as if he is looking at the world through a tube. Twilight vision deteriorates significantly. The patient sees practically nothing in the dark.
The acute course of the disease can cause the patient severe pain in the eye area, which flows into the head area. A person’s temperature “jumps,” he feels chills, feels nauseous, and sometimes vomits. On palpation, the organ of vision seems very hard. This is how angle-closure glaucoma usually manifests itself during an exacerbation.
Causes of excavation
The zone of exit of glial fibers is present in all people. On ophthalmoscopy, it is identified as a discolored circle of varying diameter with curved blood vessels that cross the optic disc. By examining the fundus of the eye, the ophthalmologist determines its shape, width, and size. Based on changes in these parameters, the doctor may suspect a disease. The size of the nerve fiber exit zone is directly related to the diameter of the disc. If a person has a large one, then the physiological excavation will be wide. The types of normal excavation include:
- a small depression in the center of the disk;
- central extension;
- excavation with temporal retraction.
High blood pressure damages the nerve.
Relatively rare causes of disc deepening include traumatic damage (after traumatic brain injury), various neurological abnormalities, papilledema, neuroopticopathy, thrombosis or embolism of the central retinal vein. In all these cases, the expansion of the zone of exit of nerve fibers is accompanied by other specific symptoms.
Diagnostics
In the process of diagnosing the condition of EDZN, the ophthalmoscopy technique is applicable.
Before such an examination, the patient’s eyes are instilled with a drug that dilates the pupil. This method provides the best conditions for assessing the condition of the fundus.
Three methods of the described research are applicable in medical practice:
- Direct ophthalmoscopy. The patient is in a darkened room, and a traditional ophthalmoscope is used during the examination.
- Examination using a flashlight ophthalmoscope. A light beam is directed at the pupil, and a specialist, using tiny equipment lenses, makes a diagnosis on a scale magnified 15 times.
- Indirect ophthalmoscopy. The patient is sitting or lying down. The patient wears a device on his head, its lens is placed close to the eye cornea. The result is an inverted, enlarged image of the fundus.
- Ophthalmoscopy using a slit lamp. Helps to obtain the same result as in the case of reverse ophthalmoscopy, only on an enlarged scale.
Methods for diagnosing excavation expansion
The simplest examination methods include ophthalmoscopy. Using a special device or lens, the doctor examines the fundus of the eye and notes the presence of changes in the optic nerve head. Using this method, you can determine the shape of the excavation, the presence of its expansion, approximate dimensions, type of pathology, and suspect glaucoma. The photorecording method during ophthalmoscopy is important for monitoring the development of the disease. To confirm glaucoma, the following diagnostic methods are used:
- Heidelberg retinal tomograph. A powerful microscope, which allows you to determine the exact size of the pathology, however, does not show the degree of thinning of glial fibers, and therefore is useless for monitoring the development of the disease.
- Optical coherence tomography. Allows you to examine the deep layers of the disc and monitor the progression of glaucoma, as it shows a section of nervous tissue.
Return to contents
Treatment
Conservative (medication, hardware techniques, gymnastics) and surgical methods of therapy are selected for the patient based on the data obtained during diagnosis. The optic disc can undergo pathological changes due to glaucoma, edema, thrombosis of the central retinal vein, optic disc neuropathy, etc.
Thus, excavation of the optic disc is not a pathological manifestation in all cases. A competent assessment of the clinical picture is made through ophthalmoscopy (its various techniques). When relevant diseases are detected, therapeutic measures are aimed at eliminating the underlying disease.
Symptoms of optic disc diseases
Among the pathologies of the optic nerve head, the following diseases are distinguished:
- Glaucomatous atrophy of the optic nerve (death of its fibers)
- Edema (impaired outflow and fluid retention in tissues)
- Thrombosis of the central retinal vein - disturbance of blood flow in the central vein of the retina or its branches
- Optic nerve atrophy (optic neuropathy).
As a rule, the symptoms of pathologies boil down to a sharp decrease in vision, loss of color, loss of visual fields, and the appearance of spots before the eyes. Patients often complain of sharp, aching headaches on the side of the damaged nerve, as well as pain on the inside of the eyeball, which intensifies with eye movement.
Optic nerve: structure, functions, diseases - “Healthy Eye”
One of the most important elements of the visual apparatus is the optic nerve. It has a complex structure and plays a central role in the transmission of impulses to the brain. The optic nerve, like any organ, is susceptible to a variety of diseases.
Even with minor damage, visual acuity begins to rapidly decline. Without timely treatment, the element atrophies and the person goes blind. The pathology is irreversible, since nerve cells are practically not restored.
What is the optic nerve?
This is a plexus of the finest nerve fibers through which primary optical impulses, read by the cells of the retina, pass and enter the brain. Their structure is different from other fibers. In appearance it resembles brain matter.
Structure
The anatomy of the optic nerve is complex and takes up a lot of space. The average element length is from forty to fifty millimeters. The main part of the nerve is located inside the orbit. It is located in the bone formation, in the same place as the organ of vision itself. The fibers are surrounded on all sides by parabulbar tissue (fatty matter).
The optic nerve has four main sections:
- intraocular;
- tubular;
- cranial;
- orbital.
Optic disc
The optic disc is the beginning of the optic nerve. The disc is formed by processes of retinal cells. The ending of the nerve is chiasm. This is a kind of crossroads located above the pituitary gland inside the skull.
Because the disc is a collection of nerve cells, it protrudes slightly above the surface. Therefore, doctors sometimes call it a “papilla.” The optic disc occupies a small area, a maximum of three square millimeters. Element diameter – 2 mm. The disc is not located strictly in the center of the retina, it is slightly shifted towards the nose. In this regard, scotomas or “blind spots” are formed on the membrane.
The optic disc has virtually no protection. The nerve develops sheaths only when passing through the sclera, i.e., at the exit from the eyeball.
| The blood supply to the disc is carried out by small processes from the ciliary arteries and is segmental in nature. For this reason, if this process fails, a sharp and sometimes irreversible loss of optical function is diagnosed. |
Optic nerve sheaths
The optic disc is not protected by membranes; they are formed only in the intraocular region, at the site of exit from the organ of vision into the orbit. The shells are represented by the following formations of matter:
- soft cerebral;
- vascular (arachnoid);
- dura mater.
All membranes envelop the optic nerve layer by layer until it exits the orbit into the cranium. Subsequently, the element and chiasma are covered only by a soft shell. Inside the skull they are located in a special tank formed by vessels.
Blood supply to the optic nerve
The intraocular part of the skull is equipped with a large number of vessels. However, they are small in size and are mainly capillaries. Because of this, the natural blood supply remains normal only if there is good hemodynamics of the whole body.
The optic nerve head is equipped with a minimal number of small vessels that can only supply the element with blood segmentally. The deeper structures of the optic disc are supplied with “red fluid” by the central artery of the retina. But due to the low pressure gradient in it and its small size, blood stagnation and the development of infectious pathologies are often observed.
The intraocular area has a good blood supply, the main part of which comes from the vessels of the soft shell of the brain and from the central artery of the optic nerve. The chiasma is well supplied with blood due to the subarachnoid membrane, into which the “red fluid” penetrates from the internal carotid artery.
Functions
The element is not assigned too many tasks, but all of them are of great importance in human life. Main functions of the optic nerve:
- Transfer of information from the retina to the cerebral cortex using a variety of intermediate structures.
- Lightning-fast reaction to external stimuli (loud noise, bright light, etc.). As a result, a protective reaction is triggered reflexively in the body (jumping, withdrawing the hand).
- Reverse sending of impulses from the cortical structures of the brain to the retina.
Optic nerve - structure, functions, diagnosis of diseases
The optic nerve is a bundle of nerve fibers that ensures the transmission of nerve impulses caused by light stimulation to the visual center of the occipital lobe of the brain from the retina.
Structure and functions
From the sensory cells of the retina, nerve fibers are collected into the optic nerve at the posterior pole of the eye. The total number of nerve fibers that form the optic nerve is slightly more than 1 million, and their number gradually decreases with age.
Anatomy of the optic nerve
Scheme of the structure of the visual analyzer 1 - retina, 2 - uncrossed fibers of the optic nerve, 3 - optic tract, 4 - external geniculate body (ECF), 5 - radiatio optici - optic radiation - a bundle of nerve fibers in the telencephalon.
6 - visual centers in the occipital lobe cortex.
- the second pair of cranial nerves through which visual stimuli perceived by the sensory cells of the retina are transmitted to the brain.
Optic nerve (n.
opticus) is a nerve of special sensitivity, in its development and structure it is not a typical cranial nerve, but a kind of cerebral white matter, brought to the periphery and connected with the nuclei of the diencephalon, and through them with the cerebral cortex, it is formed by the axons of ganglion retinal cells and ends in the chiasm. In adults, its total length varies from 35 to 55 mm. A significant part of the nerve is the orbital segment (25-30 mm), which in the horizontal plane has an S-shaped bend, due to which it does not experience tension during movements of the eyeball.
Over a considerable distance (from the exit from the eyeball to the entrance to the optic canal - canalis opticus), the nerve, like the brain, has three membranes: hard, arachnoid and soft. Together with them, its thickness is 4-4.5 mm, without them - 3-3.5 mm.
At the eyeball, the dura mater fuses with the sclera and Tenon's capsule, and at the optic canal, with the periosteum.
The intracranial segment of the nerve and the chiasm, located in the subarachnoid chiasmatic cistern, are dressed only in a soft shell.
The intrathecal spaces of the orbital part of the nerve (subdural and subarachnoid) are connected to similar spaces in the brain, but are isolated from each other. They are filled with fluid of complex composition (intraocular, tissue, cerebrospinal).
Since intraocular pressure is normally 2 times higher than intracranial pressure (10-12 mm Hg), the direction of its current coincides with the pressure gradient.
The exception is cases when intracranial pressure increases significantly (for example, with the development of a brain tumor, hemorrhages in the cranial cavity) or, conversely, the tone of the eye significantly decreases.
The optic nerve originates from the ganglion cells (third nerve cells) of the retina. The processes of these cells are collected in the optic disc (or papilla), located 3 mm closer to the middle from the posterior pole of the eye.
Next, bundles of nerve fibers penetrate the sclera in the region of the cribriform plate and are surrounded by meningeal structures, forming a compact nerve trunk. Nerve fibers are insulated from each other by a layer of myelin. All nerve fibers that make up the optic nerve are grouped into three main bundles.
The axons of ganglion cells extending from the central (macular) region of the retina constitute the papillomacular fascicle, which enters the temporal half of the optic nerve head. Fibers from the ganglion cells of the nasal half of the retina run along radial lines into the nasal half of the disc.
Similar fibers, but from the temporal half of the retina, on the way to the optic nerve head “flow around” the papillomacular bundle from above and below.
In the orbital segment of the optic nerve near the eyeball, the relationships between nerve fibers remain the same as in its disk.
Next, the papillomacular bundle moves to the axial position, and the fibers from the temporal quadrants of the retina move to the entire corresponding half of the optic nerve. Thus, the optic nerve is clearly divided into right and left halves.
Its division into the upper and lower halves is less pronounced. An important clinical feature is that the nerve is devoid of sensory nerve endings.
In the cranial cavity, the optic nerves connect above the area of the sella turcica, forming a chiasma (chiasma opticum), which is covered with the pia mater and has the following dimensions: length 4-10 mm, width 9-11 mm, thickness 5 mm.
The chiasma borders below with the diaphragm of the sella turcica (the preserved portion of the dura mater), above (in the posterior section) with the bottom of the third ventricle of the brain, on the sides with the internal carotid arteries, and behind with the pituitary infundibulum.
Among the bundles of optic nerve fibers are the central retinal artery (central retinal artery) and the vein of the same name. The artery arises in the central part of the eye, and its capillaries cover the entire surface of the retina. Together with the ophthalmic artery, the optic nerve passes into the cranial cavity through the optic canal formed by the lesser wing of the sphenoid bone.
Having passed through the thickness of the fatty body of the orbit, the optic nerve approaches the common tendon ring. This part of it is called the orbital part (lat. pars orbitalis). Then it enters the optic canal (lat.
canalis opticus) - this part is called the intracanalicular part (lat. pars intracanalicularis), and the intracranial part (lat. pars intracranialis) emerges from the orbit into the cranial cavity. Here, in the area of the pre-cross groove of the sphenoid bone (lat.
os sphenoidale) there is a partial intersection of the fibers of the optic nerve - lat. chiasma opticum.
The lateral part of the fibers of each optic nerve is directed further along its side.
Anatomy of the optic nerve
The human optic nerve is not related to the peripheral or autonomic nervous systems.
Its structure involves axons that resemble the structure of the cells of the white matter of the brain. It is covered with a dense membrane of plasmalemma, which is capable of synthesizing myelin formations. The pair of bundles is part of a complex system of cranial nerves (CN), which can consist of several groups:
- visual;
- oculomotor;
- block;
- trigeminal;
- diverting;
- facial
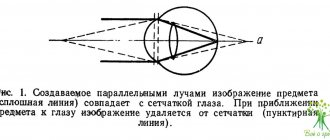
Inverted reflection of objects when analyzing visual sensations
The optic nerve is at least 4 cm in length and can occupy a large area behind the cornea. It is protected from external influences by the bone tissue of the orbit and reliably hidden by a dense layer of fatty parabulbar tissue. Conventionally, ophthalmologists distinguish several parts, as indicated in the topography:
- intraocular or primary;
- tubular;
- cranial;
- orbital.
The optic nerve is formed from processes of brain cells. Therefore, the structure is highly sensitive and contains at least 1 million nerve axons. They connect into a single network with photoreceptors, turning into a unique human vision system.
Features of structure and topography
Unlike other nerves, the optic nerve can form white matter, which is anatomically located in the periphery.
It can innervate with fibers directly into the nuclei and rods of the intermediate cranial region and transmit signals and information to the cerebral cortex. The innervation originates from glial cells in the retina of the eyeball. They are concentrated in the posterior pole in the form of a cone, pass through the cribriform plate and sclera, receiving light signals from all parts of the organ of vision. All fibers gather in a crossing bundle inside the skull near the nasal cavity, thicken, can intersect, and begin to form a thick trunk.
Main parts of the optic nerve:
- intrabulbar;
- intraorbital;
- intracanalicular;
- intracranial.
Inside the skull, the nerve is protected by a dense tendon ring and gradually enters the cavity of the canal formed on the upper part of the sphenoid bone.
Near the brain stem, the fibers bifurcate and enter the cortical visual centers of the brain, which are located in the back of the skull.
In this part, with the help of receptors, the received signals, visual images and information are processed.
The beginning or exit is the optic disc of the optic nerve (OND), which has the second name “papilla”. This is a node of many nerve cells of neurons of a pale pink hue, reaching a diameter of 0.2 cm. It is located on the retina of the eye near the bridge of the nose. Lateral vision and the formation of blind spots in humans depend on it.
In a middle-aged person, the disc does not have any inclusions, but with atherosclerosis, yellow dots may appear on the section. It has clear boundaries of the circle, but with chronic hypertension and high intraocular pressure it begins to look blurry.
The final site is the optic chiasm, which is the location in the brain where fibers from each eye cross or cross. On the topographic diagram, the tract is located near the hypothalamus. This allows you to correctly process visual images through partial overlay and combination, eliminating spatial distortion.
Structure of the optic disc
For most people, the area remains virtually unchanged throughout their lives. It contains the highest concentration of small capillaries. In the light, when examining the bottom using special equipment, it has a white color due to the scattering of light rays by ganglion cells on the trunk. When they decrease, glaucoma often develops, which quickly becomes chronic.
The exit site of the optic nerve does not have pits or canals and has a smooth surface. Doctors noticed that the shape (excavation) and thickness affect the susceptibility to diseases of the organ of vision. The congenital and acquired number of nerve analyzers is important:
- if the scleral canal is too narrow, the person experiences nerve ischemia with loss of vision;
- a small disc leads to pseudoedema and blurred images.
Atrophy often occurs on the angular part of the disc, which processes information from the temporal nerves and is responsible for peripheral vision. The affected area indicates a tendency to glaucoma or myopia.
Anatomy of the visual pathway
The cells that form the basis of the nerve are not capable of myelination and repair.
In the first intersection at the exit from the medial retina, axons are concentrated that control the movement of the pupil and its contraction in response to light. The signal is then transmitted to the lateral nucleus of the thalamus, which is responsible for different visual angles. The visual pathway can surround the human midbrain and is divided into two parts along the way:
- Medial root. It begins to emerge on one side towards the thalamus and can serve as an important receptor for conditioned reflexes.
- Lateral. Enhances the perception of colors, helps the brain distinguish shades, stimulates the activity of the visual zone.
The optic nerve is part of the pathway and complements the chiasm and tract. The entrance begins from the retina, and a bundle of sensory axons can exit in the region of the occipital lobe.
Blood supply and nerve nutrition
A branch of a million cells constantly transmits and receives visual information. To maintain activity, it is supplied with blood from several large and small vessels:
- central artery of the retina;
- retinal;
- axial
The optic nerve is formed in the first weeks after conception and begins to develop after 3 months of pregnancy. It grows in small bunches, which are separated from each other by strong transverse partitions. Capillaries and veins can cross and pass through them, supplying blood for the growth and functioning of axons.
Around the optic chiasm there is a large plexus of several vessels. They provide an uninterrupted flow of oxygen and nutrients. The most problematic area is the central retinal artery: low pressure is observed in it, blood stagnation often occurs, which threatens the development of infections, inflammation, and deterioration of visual acuity.
Basic functions of the optic nerve
The entire visual pathway in the brain is responsible for receiving information and vision. The main task of the nerve:
- instant transmission of information about a stimulus (bright light, changing colors at a traffic light, turning on a lamp);
- transformation of signals from the retina to the cerebral cortex;
- receiving back processed information about the picture seen;
- allows you to view objects at a distance or close to a person.
The optical tract is responsible for the formation of the first stage of the conditioned reflex: it sends a signal about a bright flash to the brain, which reacts to danger.
Modern research and diagnostic methods
Examination of the fundus and optic nerve
The optic nerve is sensitive to various infections and viruses. In case of damage, topical diagnostics are used using unique equipment. Basic research methods:
- ophthalmoscopy for vascular changes, distortion of the disc shape;
- optical coherence tomography or OCT;
- campimetry to determine the angle and field of view.
The clinical picture of optic nerve damage consists of several components: the general ophthalmological picture, decreased acuity and changes in viewing angle. If there are no signs of inflammation or pathologies on the disc, it is necessary to monitor the condition of the fibers along the path to the brain. In diseases of the chiasm, fundus pressure may not change.
The main task of topical diagnostics is to identify hemianopsia at an early stage. This is a whole group of defects that occur only in one field of vision on the left or right side. A person’s area completely falls out, and their vision narrows. In this case, the complication can affect the top or bottom.