What does the cornea do?
Main characteristics of the cornea of the eye:
- Smoothness.
- Sphericity
- Transparency (the cornea has no blood vessels).
- High sensitivity.
- Mirror shine (due to constant hydration due to tears)
The cornea is characterized by high rates of tissue regenerative abilities. However, the peculiarities of its anatomical location contribute to the fact that the cornea is often exposed to external negative factors. In some cases, this can cause the development of a number of diseases, including infectious etiology.
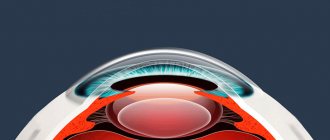
Structure
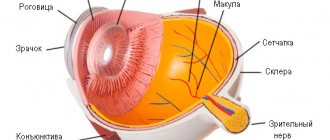
The cornea is similar in appearance to a lens, convex on the outside and concave on the inside. It occupies from 1/5 to 1/6 of the entire surface of the outer shell of the visual apparatus. Unlike the sclera, it does not have a vascular network and is 100% transparent.
The thickness of the element increases along the periphery and decreases in the center. The cornea consists of five layers:
- Anterior (integumentary). Responsible for eye protection and moisture exchange. Consists of epithelial cells.
- Bowman's membrane. Maintains the shape of the cornea.
- Stroma (thickest layer). Formed by collagen fibers, fibro-, kera- and leukocytes. Responsible for the strength of the cornea.
- Descemet's. Provides increased tolerance of the outer layer of the visual apparatus to external and internal stimuli.
- Endothelial (posterior). A layer containing hexagon-shaped cells. They act as a pump, supplying the membranes of the cornea with useful substances from the intraocular moisture. Therefore, when pathological processes are activated in the endothelial layer, swelling of the membrane rapidly develops.
| The cornea communicates with the central nervous system through autonomic neural plexuses. On the surface of the upper layers there are three hundred times more of them than on human skin. For this reason, when an injury occurs that violates the integrity of the membrane, the victim experiences severe pain. |
Due to the lack of blood vessels, the intraocular moisture and capillaries surrounding the element are responsible for feeding the cornea. The main sign of impaired blood supply is clouding of the membrane. This is explained by the germination of capillaries from the limbus or vascular film.
Features of the structure of the cornea of the eye
Nutrition and supply of the cornea with necessary substances is carried out through the capillaries of the marginal loop network in the sclera, as well as through the tear fluid. The diameter of the cornea is on average 1 cm.
Structure and functions of the cornea of the eye:
- Superficial epithelium of the cornea. In accordance with the anatomy, the front part performs a protective function and is also responsible for internal moisture exchange.
- The membrane is called Bowman's membrane. Its function is to maintain the anatomical shape of the cornea. If Bowman's membrane is damaged due to injury or infection, opacification occurs in the area after healing.
- Stroma. This part is needed to provide the cornea with strength; it has maximum thickness and dimensions.
- Descemet's membrane. The most durable layer of the cornea, resistant to infectious agents. If it is destroyed, there is a high risk of infection entering the eyeball.
- Corneal endothelium (inner layer). This layer provides the cornea with nutrients from the moisture of the anterior chamber of the eye, which makes it especially important. Impaired functioning of this layer can cause rapid development of swelling.
What it is?
The cornea is the convex and transparent part of the eyeball. It consists of five shells. It is a natural lens in the shape of a sphere, with the help of the finest fibrous fibers it is attached to the sclera of the visual apparatus.
The element is characterized by increased sensitivity due to the presence of a large number of nerve endings. It has the ability to transmit and refract light impulses.
In the absence of deviations, the cornea corresponds to the following indicators:
- Radius of curvature: from 7.7 to 9.6 millimeters.
- The refractive power is forty-one diopters.
- Ability to recover.
- Absolute transparency and specularity of the surface.
- Strength and integrity.
- There are no capillaries in the shell.
- Spherical shape.
- The horizontal diameter is eleven millimeters.
| Inflammatory processes or injuries lead to disruption of initial indicators and changes in its properties. |
Types of diseases of the cornea of the eye
Among the main diseases to which the cornea of the eyeball is susceptible, the following should be cited:
- Traumatic injuries. They are the result of exposure to external factors. For example, they develop due to the ingress of small solid particles, impact, or bruise. The resulting damage can be deep or superficial. Depending on the depth and location of the damage, visual acuity may suffer and the shape of the cornea may be disrupted after healing.
- Diseases of inflammatory etiology, which can be infectious or non-infectious in nature. The development of such pathologies can cause a violation of a number of properties of the cornea, as well as lead to the germination of blood vessels and the occurrence of opacities.
- Dystrophy. It can be congenital or acquired. The reason for the development is due to metabolic disorders in the connective tissue of the body. More often, dystrophy is diagnosed during preventive examinations.
- Microcornea and macrocornea. The pathology is congenital in nature and represents a change in the size of the membrane, in contrast to normal, to a smaller or larger direction.
- Keratoconus/keratoglobus. Dystrophic change in corneal tissue, which may be accompanied by a change in the shape of the cornea and a severe decrease in visual acuity.
- If symptoms indicating the development of pathologies are identified, immediate diagnosis and choice of treatment is necessary, otherwise there is a possibility of developing a number of complications, including decreased visual acuity or complete blindness.
Corneal reflex and protective functions of the cornea
The function of optical refraction makes the cornea the first step in the functioning of the entire visual system. However, in addition, like the sclera, this part of the shell of the eyeball protects it from the external environment. At the same time, it is the cornea that takes on all kinds of influences from the outside (dust, wind, moisture, temperature changes).
Extreme sensitivity provides reliable protection not only for the deeper structures of the eye, but also for the cornea itself. The slightest irritation, fear, or a particle flashing before the eye causes an unconditioned reflex - blinking, combined with lacrimation. Thus, the cornea protects itself from damage, bright light and other unwanted influences. When you blink, the eye rolls upward under the eyelid and tears are released, washing away possible dust particles to the corner of the eye.
Treatment of corneal diseases
Features of the treatment of diseases and pathologies of the cornea depend on the nature of the origin of the disease. Treatment can be conservative (for example, in the case of inflammatory diseases) or surgical (in the case of injuries or dystrophic changes in the shape of the cornea).
In the absence of a positive treatment result for a long time, as well as against the background of rapid loss of vision or extensive eye injuries, keratoplasty or keratoprosthesis may be used. In the first case, donor material is used, and in the second, artificial elements are used.
Due to the fact that the cornea, which is located on the surface, is devoid of a vascular network, it has a high regenerative ability. In most cases, operations performed on this area of the eye have a positive outcome. In the absence of individual contraindications, surgery is the most effective method of therapy.
Cornea diagnostic methods
The cornea is studied to identify possible damage to its layers, as well as to evaluate its curvature as a possible cause of decreased visual acuity. The following ophthalmological examinations are carried out:
- Biomicroscopy of the cornea. Standard examination of the cornea under a microscope with illumination. This diagnosis makes it possible to identify most diseases, as well as injuries and changes in the curvature of the cornea.
- Pachymetry allows you to measure the thickness of the cornea. This test is performed using ultrasound.
- Mirror microscopy is the study of the endothelial layer using photography. In this case, the shape of the cells is analyzed and their number per 1 square meter is calculated. mm area. The normal density is considered to be 3000 cells per 1 square meter. mm.
- Keratometry measures the curvature of the anterior surface of the cornea.
- Corneal topography is a complete computer examination of the entire area of the cornea. Allows you to accurately analyze the cornea by thickness, curvature and refractive power.
- Microbiological studies are aimed at studying the microflora of the corneal surface. The material for this study is taken under local drip anesthesia.
- A corneal biopsy is advisable if the results of scrapings and cultures are inconclusive or uninformative.
Functions
Main functions of the cornea:
- Refraction of light streams. In terms of its anatomical structure, the shell resembles an optical lens, which collects impulses coming from different directions into a “beam”. Therefore, the cornea is the most important element of the refractive system of the visual apparatus.
- The shell also performs a protective function. It prevents the penetration of dust and dirt particles, which are concentrated in large quantities in the air. Since the cornea has increased sensitivity to light, it reacts almost instantly to changes in temperature. As a result, even with a minor injury, the eye closes at the reflex level. At this moment, tear fluid is produced, which helps to get rid of the foreign object.
Symptoms
When damage occurs on the cornea, numerous nerve endings are exposed, so pain in the eye occurs as soon as the disease begins to develop.
As the patient recovers, the feeling of pain may be replaced by the sensation of a foreign body in the eye. Due to the exposure of nerve endings and pain, photophobia and excessive lacrimation appear.
The nerve endings become inflamed, the eye becomes sensitive to external factors, and redness of its mucous membrane appears. A secondary viral or bacterial infection may occur, worsening the course of the underlying disease. If the erosion is located in the center of the eye, or it is large in size, the patient’s vision may deteriorate. This occurs due to swelling of the corneal tissue and a decrease in its transparency.
One of the directions of development of ophthalmological science is associated with the development of new and improvement of known diagnostic technologies, providing the possibility of a comprehensive assessment of the anatomical and functional state of various structures of the eyeball and its adnexal apparatus. The main functions of the cornea are associated with light transmission, light refraction and maintaining the shape of the eyeball, and methods for assessing the functional state of the cornea are with the assessment of its structure, refractive and biomechanical properties, respectively.
Modern diagnostic methods can be conditionally divided into basic and special (clarifying), with the main criterion for such division being the possibility of using the study in an outpatient setting (or during the initial patient consultation). Trends in improving diagnostic technologies can be formulated as follows: 1) development by expanding the block of special methods; 2) complication; 3) availability of trained personnel; 4) accumulation of experience for correct processing of research results.
The need for an integrated approach to the study of the cornea is associated not only with the diagnosis and monitoring of its diseases, but also with the dynamic assessment of the condition of the cornea after the currently widely used keratorefractive [1] and various intraocular (primarily performed for cataract) operations.
In the modern methods of studying the cornea currently used, various principles for obtaining information can be used: microscopic, optical, topographic, mechanical, metric, tomographic, but most often the diagnostic technology simultaneously contains several research principles.
This article summarizes the experience of clinical application (more than 10,000 studies) of modern methods aimed at assessing the refractive properties and structure of the cornea. A detailed discussion of the possibilities for studying the biomechanical properties of the cornea is presented in a separate report in this issue of the journal.
Methods for studying the refractive properties of the cornea
Relatively recently, the main and essentially the only method for assessing the refractive properties of the cornea was to study the radius of curvature of its anterior surface and, accordingly, the refractive power in the central zone (ophthalmic or keratometry). Meanwhile, since the geometric shape of the cornea is close to a paraboloid of rotation, the radius of its curvature changes (specifically, increases) in the direction from the center to the periphery. That is why methods of topographic study of corneal curvature and refraction are currently widely used. In addition, in recent years, various methods for assessing eye aberrations—image errors caused by defects in the optical system of the eye—have been actively used in clinical practice.
Computer videokeratotopography (videokeratography)
Computer videokeratography is one of the most widely used methods for topographic study of corneal refraction (CT-1000 computer topographer, Japan). The method is based on computer processing of concentric rings of the Placido disc projected onto the cornea, any distortion of which is recorded for computer analysis. The result can be obtained both in digital terms and in the form of a color-coded map. The method makes it possible to determine the refractive power and radius of curvature of the cornea, as well as obtain three-dimensional models of all types of corneal maps for a visual representation of changes in various parameters [8, 19].
The software of modern computer diagnostic systems provides for determining the values of statistical indices characterizing the topographic features of the cornea [54, 56, 60, 61]. Thus, the surface asymmetry index reflects the difference in optical power between opposite half-meridians. The lower the values of this index (normally less than 0.5), the higher the degree of symmetry of the corneal surface.
The surface regularity index is determined by comparing the optical power within a zone of the cornea with a diameter of 4.5 mm and outside the latter. Index values above 1.0 indicate surface irregularity. To diagnose keratoconus, the Rabinovich index is also used: the difference in the refractive power of the cornea above and below the center of the cornea by 3 mm. Positive index values indicate steepening (decreasing the radius of curvature) of the lower part of the cornea, negative values indicate steepening of the upper part of the cornea. An index value of more than 1.2 D may be a sign of keratoconus [55].
The asymmetry index of the steepest radial axes is the angle between the steepest semi-meridians above and below the horizontal axis. An index value above 21° may be a sign of keratoconus [52, 53, 55].
The KISA index is calculated as a percentage based on keratometry data of the center of the cornea, the value of corneal astigmatism, the values of the Rabinovich index and the asymmetry index of the steepest radial axes. Index values from 60 to 100% are regarded as suspected keratoconus, values more than 100% are considered clinical manifestations of keratoconus [56].
Using the Klyce/Maeda method, the keratoconus index is calculated, which reflects the totality of the topographic characteristics of the corneal surface and allows, to a certain extent, to judge the presence of keratoconus. With a value of 0%, there are no signs of keratoconus; as the disease develops, the index values increase from 1 to 95% [60, 62].
The disadvantages of videokeratography include the limited area of study, which is about 60% of the surface of the cornea, which does not allow qualitative examination of its peripheral parts.
Summarizing the experience of using computer videokeratography, we can identify the main clinical situations in which the information content of the method is quite high.
1. Diagnosis of various forms of corneal astigmatism.
In typical cases, the astigmatic figure on the videogram with direct astigmatism is an “hourglass” figure with approximately equal areas on both sides of the center. In cases of reverse astigmatism, the hourglass figure takes a horizontal position. Astigmatism with oblique axes is represented by an hourglass figure located at an angle relative to the vertical axis. With correct astigmatism, the picture should be symmetrical; different sizes of the hourglass segments or a violation of their symmetry with respect to the axes of the main meridians indicate a violation of the regularity of the corneal surface [8, 57, 62, 67].
2. Changes in the topography of the cornea when exposed to various factors.
The use of almost all types of contact lenses (CL) can lead to statistically significant changes in the topography of the cornea [22]. As a rule, these changes consist of increased corneal refraction and disruption of regularity [20, 43]. Significant distortion of the Placido disc rings can occur when the stability of the precorneal tear film and the structure of the epithelial membrane of the corneal surface are disrupted in dry eye syndrome, including those that occur when wearing CLs [8, 20, 34, 65].
3. Diagnosis of keratoconus.
Typical for the early stages (I-II) of the disease is a topogram pattern (“bow-tie” - bow tie) or local “steepening” of the cornea below the horizontal axis
(Fig. 1, a, b).
Figure 1. Types (a-c) of keratotopograms for keratoconus.
Explanation in the text. In stages III-IV of keratoconus, there is a zone of significant “steepening” of the cornea, slightly displaced downward relative to the center, in addition, the formation of a central zone of secondary stretching in the form of a section with a large radius of curvature (see Fig. 1, c)
[12, 68] .
The so-called subclinical stage of keratoconus is characterized by a local area of “steepening” of the cornea below the center, corneal astigmatism with asymmetry in relation to the horizontal and vertical axis with “steepening” in the lower half, and a topographic picture similar to marginal pellucid degeneration. According to our data, these changes can occur in 36, 12.5, 22 and 11% of cases, respectively.
Changes in at least one of the keratoconus indices are recorded in 78.46% of cases. It should be noted that the average values of the radii of curvature of the cornea in the center at the subclinical stage of keratoconus, as a rule, remain within normal limits [16-18].
4. Diagnosis of the early stages of dystrophic changes in the cornea.
In the early stages, it is often possible to detect changes in the topography of the anterior surface of the cornea with the formation of zones of ectasia of a shape and localization atypical for keratoconus [18].
5. Postoperative changes in corneal topography
arise as a result of various surgical interventions (excimer laser methods for correcting refractive errors, keratotomy, end-to-end corneal transplantation, cataract extraction operations, etc.) In this case, characteristic topographic patterns are recorded [5, 10, 28, 67, 69].
Scanning projection keratotopography
The scanning projection keratotopograph (Pentacam HR device, Germany) is based on the principle formulated in 1904 by Theodor Scheimpflug and allows obtaining high-quality optical sections of objects located at different angles to the camera. Measurement data (front and back refractive topography and corneal thickness) are presented in color maps, diagrams and three-dimensional images [27, 28, 35]. So-called elevation maps are formed by superimposing the obtained data on a “ideal” sphere (BFS) calculated for each cornea.
To diagnose keratoconus, the program provides various indices that characterize the topography of the anterior surface of the cornea. The most sensitive of them are: the apex displacement index relative to the center, the vertical asymmetry index, and the keratoconus index. The question of the informative value of changes in the curvature of the posterior surface of the cornea in terms of early diagnosis of keratoconus remains controversial [31].
Aberrometry
The use of aberrometry in clinical practice is mainly due to the need to solve various issues of keratorefractive surgery. In addition, aberrometry can be used to assess the influence of various factors on the optical properties of the cornea and the possibility of correcting emerging optical disorders [6].
The principle of operation of the Cherniga aberrometer is based on the projection onto the retina of a grid of 168 points located in the shape of a square, recording its retinal image with a digital camera and computer processing of the results [49]. Beam tracking aberrometry is based on assessing the deviation of a parallel laser beam from the reference or main beam, which is directed strictly along the visual axis. In this case, each point within the pupil is sequentially analyzed [47]. The Shack-Hartmann aberrometer allows one to obtain information about the characteristics of the wavefront based on the analysis of the reflected laser beam using a system of microlenses and computer processing of the results obtained [64]. The OPD-Scan device implements the principle of classical skiascopy by scanning the optical system of the eye through a rotating plane with a slit along the optical axis. When using an additional computer program (OPD station), it is possible to isolate the corneal component of eye aberrations [30].
In keratoconus, disruption of the regularity of the corneal surface leads to a significant increase in optical aberrations, including higher orders, mainly due to vertical coma, resulting in a decrease in visual acuity and quality [9, 12, 40, 42]. An increase in the level of aberrations is observed already at the subclinical stage of the disease. The index of positive coma, described by the Zernike Z polynomial (3;1) and 3.74 times higher than the level of this parameter in emmetropic eyes, is subject to the greatest changes [7, 12, 29, 39].
Surgical interventions on the cornea also affect the aberration pattern. Thus, after radial keratotomy there is a significant increase in higher order aberrations. The structure of aberrations is dominated by aberrations of the 3rd and 4th orders, and a significant increase in spherical and sphere-like aberrations is noted [26]. Excimer laser exposure to the cornea induces higher order aberrations. As a rule, coma and sphere-like aberrations increase [44, 46, 48]. After end-to-end corneal transplantation, a significant increase in the level of higher-order aberrations (5.5 times compared to the norm) was recorded, mainly due to trefoil, spherical aberrations and, to a lesser extent, coma [12, 21, 50]. An increase in higher-order optical aberrations is also recorded in cases of disturbances in the stability of the tear film [41].
The use of rigid gas-permeable CLs (RGCLs) makes it possible to reduce the level of total high-order optical aberrations after both radial keratotomy and penetrating keratoplasty (by 47.9 and 51.3%, respectively). The use of GCL for keratoconus provides a reduction in the level of high-order aberrations in the range of 40-60%, depending on the stage of the disease [9, 12, 13]. It should be taken into account that the use of hard and soft contact lenses for the correction of myopia and correct myopic astigmatism can lead to increased high-order optical aberrations due to lens mobility; Based on aberrometry data, if necessary, the “fit” of the CL is adjusted [20].
Methods for studying the structure of the cornea
The basis of the light transmission function of the cornea is its transparency, which depends on the state of the structural layers: tear film, anterior and posterior epithelium, stroma, Bowman's and Descemet's membranes. In addition to biomicroscopy and the mirror microscopy of the posterior epithelium, which has already become a basic study, special methods are used to assess the structure of the cornea: confocal microscopy, optical coherence tomography (OCT), tiascopy and topographic pachymetry.
Confocal microscopy of the cornea
Confocal microscopy is a non-invasive intravital method for studying the cornea, allowing one to assess the condition of all layers of the cornea, as well as determine the degree and localization of morphological changes. Thus, the Confoscan-4 confocal microscope (Japan) provides the possibility of layer-by-layer scanning of the cornea in an area of 440×330 μm. The study is possible in both central and paracentral areas of the cornea. In the Z-scan system, it is possible to assess the intensity of light scattering in all layers of the cornea based on the analysis of the densitometric curve [45].
Normally, the anterior corneal epithelium consists of 5-6 cell layers. There are 3 types of cells: basal (1 layer) small polygonal, dense without a clear nucleus; spiny (2-3 layers) and surface polygonal (2-3 layers) with clear boundaries and homogeneous density. Bowman's and Descemet's membranes are not normally visualized, since they are transparent structures and do not reflect light. Normally, subepithelial nerve fibers appear as bright stripes contrasting with a dark background. In typical cases, one can see bright, irregular oval-shaped bodies (keratocyte nuclei) contrasting against the background of an opaque acellular matrix. The density of keratocyte nuclei gradually decreases towards the posterior layers of the stroma. In the anterior stroma, the keratocyte nuclei have a round, bean-shaped shape, and in the posterior stroma they are oval and more elongated. The fibers of the deep corneal nerve plexus are visualized as bright reflective stripes. The posterior epithelium of the cornea is a single-cell layer of hexagonal or polygonal flat light cells [2, 9, 45].
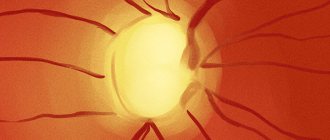
In case of keratoconus, various types of epitheliopathies are detected using confocal microscopy (Fig. 2, a),
Figure 2. Microscopic picture (a-d) of keratoconus.
Explanation in the text. the formation of micropoints (see Fig. 2, b),
the phenomenon of homogenization of the stroma
(see Fig. 2, c)
, zones with impaired transparency and scarring
(see Fig. 2, d)
[3, 9, 21, 45].
In the subclinical stage of keratoconus, morphological abnormalities can be detected in 71.2% of cases. There is a thickening of the Descemet membrane with the effect of increasing light reflection (Fig. 3, a),
Figure 3. Microscopic appearance of the posterior layers of the corneal stroma in subclinical keratoconus.
a — compaction of Descemet’s membrane (shown by an arrow); b — needle-shaped formations (shown by an arrow). in the posterior layers of the stroma - a decrease in the transparency of the corneal tissue and the appearance of needle-shaped formations oriented in different directions, which may be modified keratocyte nuclei (see Fig. 3, b)
. In the middle layers of the stroma, so-called “lacunae” are visualized - dark, cell-free rounded zones, as well as a change in the orientation of the keratocyte nuclei, “lining up” them in a line, often along the vertical axis, which is a harbinger of the formation of micropoints.
It should be noted that the described changes are not strictly specific to keratoconus and may occur with some types of dystrophies, long-term wearing of CLs, and high myopia.
With Acanthamoeba keratitis, in some cases it is possible to detect the presence of Acanthamoeba cysts in the lesion, which are visualized as brightly reflective round formations in the epithelial and subepithelial layers, less often in the layers of the anterior stroma (Fig. 4).
Figure 4. Acanthamoeba cysts in the epithelial and subepithelial layers of the cornea (shown by arrows).
The use of confocal microscopy is also possible for monitoring changes in the cornea in various types of dystrophies (Fig. 5),
Figure 5. Microscopic picture of the posterior corneal epithelium in epithelial-endothelial corneal dystrophy. dry eye syndrome (DES) [4].
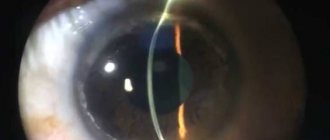
Optical coherence tomography
OCT is based on measuring the reflectivity (reflectivity) of biological structures with the construction of a cross-sectional image of a cross-section of the anterior part of the eye with high resolution [37, 38, 58, 63]. Unlike confocal microscopy, OCT provides the ability to assess the condition of the cornea throughout its entire length, but with significantly lower magnification.
In clinical practice, the method is used for objective assessment of the condition of the cornea after keratoplasty operations, diagnosis and monitoring of various diseases (Fig. 6-8)
[32, 59].
Figure 6. Tomographic picture of the cornea after posterior lamellar keratoplasty (the arrow indicates the interface zone).
Figure 7. Tomographic picture of the cornea with detachment of Descemet’s membrane (detachment area is indicated by an arrow).
Figure 8. Tomographic picture of the cornea after implantation of stromal segments (indicated by arrows) for keratoconus a.
Tiascopy
The variety of functions of the precorneal tear film (maintaining regularity and protecting the anterior surface of the cornea, transporting oxygen and nutrients to the epithelial layers of the cornea and conjunctiva, and removing waste metabolites and dead epithelial cells) makes it an integral structural part of the cornea [11].
The condition of the tear film layers can be indirectly assessed using various methods (impression cytology, Norn test, meibography) [11, 51]. Visualization of the lipid layer of the tear film can be carried out using the thiascopy method, based on photographic recording of the color phenomenon of interference resulting from the interaction of rays reflected from two surfaces of media with different refractive indexes [14, 15, 33, 51]. The color of the interference pattern at each point will depend on the wavelength of the light beam passing through the lipid layer and reflected from its inner surface, and the thickness of the layer can be calculated based on the color of the interference at each point in the area under study. To determine the thickness of the lipid layer at each point in the area under study, there is a Michel-Lévy nomogram (color scale). However, determining the thickness of the lipid layer with its help is approximate, quite subjective and does not provide complete information about the structure and uniformity of lipid distribution over the surface of the aqueous layer. To objectify the results of the study and obtain more detailed information, the Research Institute of Eye Diseases of the Russian Academy of Medical Sciences developed the Laсrima computer program, which allows, based on the analysis of a digital image of the interference pattern, to obtain information about the thickness of the lipid layer and to estimate the relative area of the studied area with a certain thickness. Digital images of the interference pattern of the precorneal tear film are obtained using an original illuminator design adapted to a photo-slit lamp.
Computer analysis of images is presented in the form of diagrams, which display, as a percentage, the relative area occupied by a lipid layer of a certain thickness within the study area. The first component of the diagram, conventionally designated by the coefficient n/d, corresponds to the zone of uncertainty in which the tear film is very thin and determining its thickness using this method is impossible. Next, the columns of the diagram are arranged according to increasing thickness of the precorneal tear film. The algorithm and informativeness of the method can be demonstrated using the example of changes in the tear film during dry eye syndrome (Fig. 9-11).
Figure 9. Interference pattern of the precorneal tear film in normal conditions (a) and with dry eye syndrome (b).
Figure 10. Percentage distribution of lipid layer thickness (a) and computer model of the normal precorneal tear film (b). Lipid distribution coefficient (K) = 1.7.
Figure 11. Percentage distribution of lipid layer thickness (a) and computer model of the precorneal tear film (b) in DES. Lipid distribution coefficient (K) =0.53.
In case of dry eye syndrome, there is a larger relative area of the zone with a minimum thickness of the lipid layer (0.07-0.5 µm) compared to the results of studying the normal tear film (63 and 23%, respectively). Areas with a greater thickness of the lipid layer during dry eye syndrome have a minimal area, and areas in which the size of the lipid layer exceeds 0.5 μm are completely absent.
Thus, computer analysis of the interference pattern of the precorneal tear film using the Lacrima program allows you to expand the capabilities of the thiascopy method and obtain additional information about the state of its lipid layer. This technique can be used to diagnose various forms of dry eye syndrome and evaluate the effectiveness of treatment.
Topographic pachymetry
The thickness index is usually used to indirectly characterize the biomechanical properties of the cornea. In addition, changes in thickness can be used to characterize the structural condition of the cornea. Thus, a significant increase in this indicator is characteristic of edema, and structural changes in the cornea with keratoconus can lead to uneven thinning and irregular astigmatism.
The standard method of ultrasonic keratopachymetry, based on recording the ultrasound signal reflected from the interfaces of media with different densities, allows one to determine the thickness of the cornea at the points of application of the device’s sensor. A more informative method is topographic keratopachymetry (scanning projection keratotopograph Pentacam HR, Germany, and coherence tomograph Visante, Germany).
Topographic pachymetry provides a visual representation of the localization of the zone with minimal corneal thickness, including in relation to its center. Normally, the distance between the point with minimum thickness and the apex of the cornea should not exceed 0.9 mm. In some cases, changes in the topographic pachymetry map may be an early indicator of developing ectasia [27].
To assess changes in corneal thickness, indicators such as spatial profile and percentage increase are used, which can be used to assess changes in the cornea from the point of minimum thickness to the peripheral parts [23, 24]. Based on the results of these studies, the pachymetric progression index is determined for all meridians, starting from the point with the minimum thickness of the cornea [25]. Normally, the progression index is in the range of 0.8–1.2, and in the presence of ectatic changes, the value exceeds these figures [66]. With so-called comparative pachymetry, the map shows the deviation of the corneal thickness at any point from the thickness of the normal cornea. The latter indicator is calculated based on pachymetry data from more than 1000 “normal corneas”. A decrease in thickness of 3% or more suggests the presence of keratoconus [36].
According to our data, with subclinical keratoconus, the minimum values of corneal thickness in most cases are within the average statistical norm, however, their average values are lower than the values determined during examination of healthy people by 7.88%. In 25.4% of cases, the pachymetric progression index increases, and the comparative pachymetry index in the center of the cornea exceeds the normal value by 2.5 times.
Normal thickness
The physical parameters of the cornea change throughout the day, but the thickness in a healthy person varies within 0.06 mm. Large deviations indicate the need for additional examination to identify the type of disease. In the absence of ophthalmological pathology, the following characteristics of the outer shell of the eye should be observed, presented in the table:
| Corneal zone | Normal thickness in adults, mm | |
| Central | 0,49—0,56 | |
| Corneal edges | 0,7—0,9 | |
Treatment
After the doctor has made an accurate diagnosis, an adequate course of treatment or surgery (depending on the type of disease) is prescribed.
Medicines
Drug treatment is prescribed if any form of keratitis is detected, as well as for mechanical injuries and dry eyes.
If an infectious process is detected, antibacterial, antiviral or antifungal agents are prescribed, depending on the type of pathogen. To eliminate inflammation and prevent scarring, local preparations (ointments and drops) containing glucocorticoids are used.
To treat mechanical injuries and superficial disorders of the cornea, medications are used to accelerate the regeneration of damaged tissue. If dry eyes are detected, moisturizing drops are used to replace natural tear fluid and other moisturizing preparations.
IMPORTANT! All medications, course of treatment and dosage must be prescribed by a doctor, even if the medications are sold without a prescription.
Transfer
Surgical intervention is required only to eliminate the most complex pathological processes. For example, to change the curvature of the cornea and improve its ability to refract light (myopia, hyperopia, astigmatism), operations are used that change the refraction of the eye.
If the pathology is only at the initial stage of development, the ophthalmologist prescribes optical correction using specially selected glasses or contact lenses.
If an irreversible clouding of the cornea or the formation of a cataract is detected in a patient, keratoplasty or transplantation of the stratum corneum of the diseased eye is performed.
Common diseases
All diseases of the cornea reduce vision, the eye loses its basic functions, which significantly reduces a person’s quality of life. But if you consult an ophthalmologist in a timely manner, adverse health consequences can be prevented.
Main pathologies:
- keratitis;
- thorn;
- ulcer;
- bullous keratopathy.
Each of the disorders has its own characteristics of course and treatment. The most dangerous is damage to the cornea of the eye, which can occur both as a result of direct injury and as a result of the development of certain diseases.
Keratitis
Keratitis develops against the background of an inflammatory reaction. It leads to changes and decrease in vision. Corneal syndrome occurs, which is accompanied by profuse lacrimation, blepharospasm, and cutting pain.
| If the course is unfavorable, inflammation leads to partial blindness. Keratitis is often complicated by corneal ulcers. |
Belmo
The thorn occurs against the background of various traumatic factors. Persistent clouding occurs, which reduces visual acuity and often requires complex microsurgical operations. Also, a cataract can form against the background of acute and chronic inflammatory reactions.
Horny ulcers
The basis of a peptic ulcer is cell destruction. It causes the formation of a crater-shaped depression and the development of blindness. The disease is most often infectious in nature. The lesion is caused by staphylococci, streptococci, Pseudomonas aeruginosa, viruses and fungi. Prolonged use of contact lenses, the use of corticosteroid drugs, and infection when particles of dust, dirt, or traumatic objects come into contact with the mucous membrane contribute to the development of pathology.
Bullous keratopathy
Bullous keratopathy is accompanied by swelling of the epithelium. The disease reduces visual acuity, causes severe pain and increased tearing. Among the provoking factors are hereditary predisposition, as well as injuries and eye infections.
Diagnostics
To make the correct diagnosis, the ophthalmologist conducts a thorough examination of the patient. Using a slit lamp (special microscope), the entire surface of the cornea is examined.
To identify the smallest areas of damage, and their presence can sometimes not be noticed during a routine examination due to their small size, the cornea is stained with a fluorescein solution. In most cases, erosion is caused by trauma to the cornea with foreign objects, so during examination the eyelids are always carefully examined to exclude the presence of even small particles of foreign bodies on them.