Vitrectomy is an ophthalmological operation that is used in patients with pathology of the retina and vitreous body of the eye, and consists of removing, in whole or in part, the vitreous body of the eye. At the end of the operation, a special liquid or gaseous component is injected into the eye cavity to restore the original volume and shape of the eyeball. Performing this type of surgery on the posterior part of the eye requires impeccable skill and high qualifications from an ophthalmologist (such a specialist is called a vitreoretinal surgeon).
Depending on the volume of the removed vitreous, vitrectomy can be total or subtotal (partial), which in turn is divided into anterior and posterior.
Reasons for deletion
In ophthalmology, there are a number of eye diseases, the development of which inevitably leads to vitrectomy. The only method to prevent complete loss of vision is removal of the vitreous.
Indications for surgical intervention:
- eye injuries from foreign body penetration;
- rupture, retinal detachment;
- infection of the eye;
- complicated retinopathy;
- clouding or hemophthalmos (impregnation of the vitreous body with blood);
- dislocation of the natural or artificial eye lens.
Attention! Hemorrhage in the eye requires special attention. Such a patient’s condition threatens retinal detachment, when only emergency help can save the situation.
The need for vitrectomy is determined by the doctor.
Possible complications of vitrectomy
After vitrectomy surgery, there is a risk of infection getting inside the eye, causing inflammation in the eye tissues. In addition, the operation itself to remove the vitreous humor of the eye can cause retinal detachment, increased intraocular pressure, and the development of cataracts.
The risks of anesthesia depend on the general condition of the patient and the presence of concomitant diseases - they are discussed with the anesthesiologist separately.
How to prepare for surgical treatment
During the period of preparation for vitrectomy, the indicated measures are carried out: the patient’s well-being, the state of the visual analyzer are assessed, and concomitant diseases are identified. Procedures carried out:
- examination of the visual organ with a slit lamp;
- coherence tomography;
- Ultrasound of the retina;
- examination of the fundus with a dilated pupil;
- fluorescein angiography (injection of a special dye into the fundus of the eye and subsequent observation of its movement through the vessels).
If the patient is taking anticoagulants, insulin for injection, or antiarrhythmic drugs, the surgeon or anesthesiologist should be notified about this.
Types of vitrectomy
The choice of the type of operation to remove the vitreous depends on the degree of removal: it can be either complete (total) or partial (subtotal).
Partial removal is divided into anterior and posterior vitrectomy, with the anterior one minimizing the occurrence of complications, helping to restore vision. Posterior – allows the surgeon to perform manipulations in the back of the eye.
If conditions allow and there are no contraindications, it is practiced to prescribe microinvasive vitrectomy - gentle surgery performed using high-precision equipment using three punctures of the eye.
Microinvasive vitrectomy is performed only in medical centers equipped with special equipment and highly qualified ophthalmic surgeons with extensive experience in performing such operations.
The use of this method in an outpatient setting is associated with extreme risk and is therefore rarely practiced.
The undeniable advantages of microinvasion:
- the level of injuries is reduced to a minimum;
- does not require hospitalization of the patient;
- the risk of bleeding is low.
The duration of the process is 30–40 minutes. If you need to connect other technologies, the time increases to an hour.
Who undergoes vitrectomy?
Surgery to remove the vitreous humor of the eye is used for a number of eye pathologies:
- Severe degrees of destruction of the vitreous body, significantly reducing its transparency and critically worsening visual acuity, without the possibility of its optical correction.
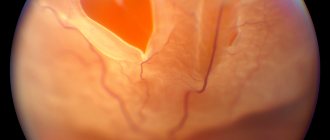
- Treatment of retinal detachment. In addition to direct removal of the vitreous, the removal of membranes and scar tissue of the retina and the subsequent introduction of special liquids (gas, silicone oil) are used to fix the retina in place until it is completely healed.
- In patients with epiretinal membrane - pathological growth of modified tissue in the macula area (the central part of the retina, the zone of best vision). In this case, combined treatment is used, combining vitrectomy and membranoectomy.
- In the treatment of proliferative retinopathy in patients with diabetes mellitus (diabetic retinopathy). In the early stages of the disease, conservative methods such as laser coagulation of the retina are used; in advanced cases, vitrectomy is indicated to remove opacities of the vitreous body, as well as membranoectomy.
- When the foveal region of the retina is detached with the formation of a macular hole or macular hole.
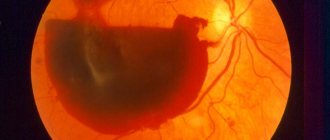
- In patients with hemophthalmos (bleeding in the eye cavity) resulting from trauma or rupture of the retina of the eye, thrombosis of the vessels of the eye, or after subarachnoid bleeding.
Vitreous substitutes
Advanced medical technologies include vitreous replacement options:
- saline solution;
- silicone oil;
- gas bubble of sterile filling;
- “The surgeon’s third hand” is a transparent liquid, a fluorine + carbon compound, which greatly facilitates retinal surgery.
The use of a replacement prevents complications after surgery.
Silicone oil
The substance is biologically and chemically inert and does not cause allergies. The oil has a refractive index equal to the natural light flux, so the retina is quickly restored. The valuable qualities of the oil make it possible for long-term installation in the eye cavity - for a year.
Gas mixture
The main advantage of gas filling is its ability to completely dissolve and be replaced by intraocular fluid. This takes from 12 to 20 days.
A person who has undergone the introduction of a gas substitute must completely avoid air travel for 3 weeks. Changes in atmospheric pressure on board an airplane provoke a dangerous increase in pressure inside the eye.
If the patient has an air bladder inserted, he will need to hold his head in a certain position - the attending physician will give recommendations. The duration of directed fixation is directly related to the extent of surgical treatment.
Liquid perfluoroorganic compounds: pros and cons of use
Another name - “heavy water” is due to the molecular weight of the compounds: it is twice as high as that of water.
The patient does not need a special treatment after this vitreous replacement. A small drawback is that the fluid needs to be changed every 2 weeks.
Features of the postoperative period
For the first 3 days after the completion of vitrectomy, the patient remains in the hospital - constant supervision of the attending physician is required. Vision after surgery is restored slowly over time.
Replacing the vitreous with saline will cause blood clots to form in the eye. If a gas bubble replacement was performed, a dark veil will appear, disappearing a week after the operation. Observations show that the clouding continues for several weeks.
The time of strict restrictions comes for the patient. He will have to fulfill the instructions recommending:
- exclude for two weeks, then limit lifting weights to 5 kg;
- Allow only 0.5 hours a day for reading and watching TV;
- do not be near open fire, including burners on the home stove;
- exclude sports exercises with bending, visiting the pool;
- refuse saunas and steam baths for a month;
- avoid heavy physical activity.
Following such an operation is not required to follow a special diet.
The listed prohibitions apply for the first 3–6 months after removal of the vitreous. Exactly following the recommendations will speed up vision recovery.
Possible complications
Even successful vitrectomy does not guarantee the patient the absence of complications in the postoperative period.
Complicated course of the disease is caused by:
- increased eye pressure;
- damage to the lens;
- retinal detachment;
- vitreous hemorrhage;
- cataract;
- formation of infection inside the eye;
- the formation of new vessels with the subsequent formation of glaucoma.
To avoid unexpected deterioration, preoperative examinations should be carried out as thoroughly as possible.
Department of Vitreoretinal Surgery and Eye Diabetes
The department employs: 14 employees, including 13 candidates of medical sciences, 13 doctors of the highest category.
Specialization of the department: the main focus of the department is the surgical treatment of diseases of the retina (retina) and vitreous body (corpus vitreum).
ABOUT THE DEPARTMENT
At the MNTK "Eye Microsurgery" named after. acad. S.N. Fedorov since 1974 there has been a department of vitreoretinal surgery and eye diabetes. The main focus of the department’s work is the surgical treatment of diseases of the retina (retina) and vitreous body (corpus vitreum), from these Latin words the name of the department comes from.
The department's doctors are skilled in the full range of surgical interventions on the vitreous body and retina. Vast experience has been accumulated in the surgical treatment of such serious diseases of the posterior segment of the eye as: retinal detachment of various etiologies, diabetic retinopathy, epiretinal fibrosis, macular hole, hemophthalmos, vitreous opacities, dislocations of native and artificial lenses and others. The constant search for new treatment methods, our own surgical techniques, the use of the most modern technologies and high-tech diagnostic and surgical equipment make it possible to treat patients with the most severe forms of vitreoretinal pathology.
Every year, more than 5,000 patients receive surgical care in the department.
The main achievement of vitreoretinal surgery in recent years is the introduction of microinvasive technologies 25-27 Gauge, wide-angle optical viewing systems, vitreoretinal dyes, endolasers, fixed endo-illuminators 29 Gauge, endo-tamponing agents (silicone oil, gases). All of them are successfully used in the department during the surgical treatment of vitreoretinal pathology.
Advantages of 27G vitrectomy compared to 25G:
- incision 0.33 mm instead of 0.5 mm;
- no need to suture the surgical access;
- healing without gross scarring of the sclera, the risk of postoperative astigmatism is reduced;
- rapid rehabilitation of patients on days 1-2, less postoperative irritation, inflammation and endophthalmitis;
- more delicate removal of preretinal membranes.
Since the operations performed are very complex, they cannot be performed without the appropriate equipment. The operating room of the department is equipped with all the necessary and most modern equipment from the best manufacturers. The new generation of modern operating microscopes and microsurgical combines guarantee unsurpassed quality for modern ophthalmic operations. Not only the fleet of technological equipment is constantly updated, but also the entire set of medicines and instruments necessary for these operations. The use of this modern equipment and medical technologies makes it possible to reduce intraoperative eye trauma and achieve good anatomical and functional results in the shortest possible time after treatment.
For surgical interventions, intraocular methods are used using expensive, complex equipment, which has significantly expanded the indications for surgical treatment. It has become possible to successfully operate on patients even with extremely severe forms of vitreoretinal diseases.
The department performs the following surgical interventions:
• operations for hemorrhage into the vitreous body of various origins - hemophthalmia (with increased blood pressure, against the background of hereditary and systemic diseases, etc.);
• operations for any, including complicated, forms of retinal detachment;
• operations for proliferative diabetic retinopathy, complicated by hemophthalmos, formation of preretinal neovascular membranes, tractional retinal detachment;
• operations for inflammatory diseases of the eye (uveitis, etc.);
• operations for injuries of the organ of vision, accompanied by intraocular foreign bodies and traumatic cataracts, with combined eye injury;
• operations for dislocation of the lens into the vitreous cavity (native and artificial - IOL);
• operations for pathology of the central part of the retina: macular hole, epiretinal fibrosis, vitreomacular traction syndrome, etc.
• combined operations for cataracts against the background of vitreoretinal pathology (proliferative diabetic retinopathy, retinal detachment, macular pathology, hemophthalmos, uveitis, post-traumatic pathology of the vitreous body and retina);
• intravitreal administration of angiogenesis inhibitors for age-related macular degeneration (wet form), diabetic macular edema and macular edema with thrombosis of the central retinal vein and its branches, with choroidal neovascularization against the background of complicated high myopia;
• intravitreal injection of drug-saturated implants for the treatment of macular edema of the retina due to thrombosis of the central retinal vein and its branches, for the treatment of diabetic macular edema and for the treatment of retinal edema due to posterior uveitis.
The department has accumulated extensive experience in surgical treatment of various pathologies, including on previously operated eyes. Surgeries for retinal detachment are performed using episcleral filling methods - in early uncomplicated cases of the disease, and the most modern methods of endovitreal intervention - in severe cases of the disease, including when retinal detachment is combined with opacification of the optical media - the cornea and lens. The department's team is a pioneer in the use of liquid perfluoroorganic compounds in retinal and vitreous surgery. For the development of this method in 1998, its authors were awarded the State Prize of the Russian Federation in the field of science and technology.
Surgical treatment of epiretinal fibrosis, macular hole, vitreous opacities and other pathologies is carried out using the method of vitrectomy (removal of the vitreous body), followed by revision of the fundus structures and removal of the epiretinal and internal limiting membranes, treatment of the wet form of macular degeneration, macular edema of various etiologies - by injection of special drugs (angiogenesis inhibitors) directly into the vitreous cavity (vitreal cavity of the eye). Progress in the treatment of severe diseases of the vitreous body and retina is due to the improvement of instruments and the development of new techniques and approaches in surgery.
Employees of the Department of Vitreoretinal Surgery and Eye Diabetes
Equipment
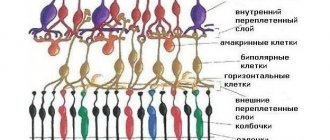
About the vitreous body
The vitreous body is approximately 99% water and contains collagen fibers, proteins and hyaluronic acid. This clear, gel-like substance that makes up the center of the eye takes up about two-thirds of its volume and helps maintain its shape.
Due to its consistency, the vitreous body can be affected by various pathological processes, which lead to its clouding and filling with blood. This, in turn, makes it difficult for light to reach the retina correctly, causing decreased vision, clouded tears, detachment and other serious pathologies.
What is vitrectomy?
Modern plastic vitrectomy was developed by Robert McHamer in 1970. Machemer created a suction device that was the first closed-system vitrectomy device, which was necessary to control intraocular pressure levels during surgery. This achievement was monumental in ophthalmology as it allowed controlled access to the posterior segment of the eye for the first time.
Initially, vitrectomy was used primarily to clear opacity such as blood from the vitreous.
In modern ophthalmology, technological development and improved equipment allow this procedure to be used much more widely. This intervention is now a fairly routine procedure for the vitreoretinal surgeon and can be performed as an outpatient procedure. Long gone are the days when 20 gauge vitrectomy was first introduced. Ophthalmologists now have 23, 25 and 27 gauge systems with improved duty cycles and cutting speeds.
Visual acuity after vitrectomy
Recovery of visual acuity after surgery will depend on the underlying disease that necessitated the need for vitrectomy. In case of treatment of destruction of the vitreous body or hemorrhage in the eye cavity, complete restoration of vision is possible. If there has been retinal detachment or other severe pathologies of the eye, the degree of vision restoration may vary, from satisfactory to residual vision, providing light perception. In some cases, the process of vision restoration can take years.
To avoid complications and ensure sufficient effect of surgical intervention, contact only specialized ophthalmological clinics.
In our clinic in Moscow, both Russians and citizens of other countries can get a consultation with a vitreoretinal surgeon and undergo treatment in the shortest possible time. The specialists of our ophthalmological center - highly qualified Moscow ophthalmic surgeons - have the appropriate level of professional training to perform microsurgical interventions in the eye cavity. Every month, our doctors perform operations on the posterior segment of the eye, which ensures constant improvement of methods for performing such interventions. The clinic is equipped with the most modern microsurgical equipment, which allows successful surgical interventions of any degree of complexity. Call today and we will preserve the priceless gift of vision!
Kinds
Vitrectomy of the eye can be of two types, depending on how the vitreous body is removed, completely or partially:
- Total (the entire vitreous body);
- Subtotal or partial (part of the vitreous).
Subtotal vitrectomy, in turn, is divided into anterior and posterior.
Front
In rare cases, the vitreous penetrates through the pupil into the anterior chamber of the eye.
This may happen:
- after eye injury;
- during surgery for cataracts or glaucoma;
- as a result of problems with the lens of the eye.
Because vitreous gel leakage can cause serious problems, anterior vitrectomy is necessary to minimize the risk of complications and promote vision restoration.
This operation is a critical tool in the skill set of the surgeon who operates on the anterior segment of the eye. Although planned anterior vitrectomy can be performed to remove traumatic cataracts or for glaucoma, this procedure is most often an unplanned and unwanted adjunct to cataract surgery.
Posterior Pars Plana vitrectomy
Vitrectomy performed for diseases of the posterior segment is called posterior or pars plana. This view is performed by a retina specialist.
Indications
Vitrectomy is sometimes necessary in the treatment of such diseases:
- Macular holes;
- Macular wrinkles;
- Retinal disinsertion;
- Diabetic retinopathy;
- Vitreous hemorrhage;
- Infection in the eye (endophthalmitis).
Parsa plastic vitrectomy is suitable when treatment requires access to the posterior segment of the eye.
General indications are:
- Rhegmatogenous or traction retinal detachment;
- Hemorrhage into the vitreous body (hemophthalmos);
- Remaining lens fragments after cataract surgery;
- Endophthalmitis;
- Epiretinal membrane;
- Macular fossa;
- Vitreomacular traction;
- Intraocular foreign bodies.
Indications for vitrectomy
The purpose of a total or partial vitrectomy is usually the following:
- Restoring the integrity of the retina when it is torn.
- Restoration of vision after total or subtotal hemophthalmos that is not amenable to conservative therapy.
- Prevention of traction leading to retinal detachment, proliferation with the formation of pathological vessels.
- Treatment of diabetic retinopathy leading to the formation of scar tissue.
- Restoration of vision in case of traumatic damage to the vitreous body and the introduction of a foreign body into the body.
Among the contraindications to vitrectomy, experts name: serious damage to the optic nerve or retina, severe clouding of the cornea.
Contraindications
Vitrectomy is contraindicated:
- in the presence of suspicious or active retinoblastoma;
- in some cases of active choroidal melanoma, since the incision of the eye may be associated with the spread of tumor cells through the circulatory system.
In some cases, such as removal of epiretinal membranes or treatment of a macular hole, the use of blood thinners (eg, aspirin or warfarin) is a relative contraindication.
Sometimes patients receiving an indirect anticoagulant (warfarin) cannot stop using it for health reasons. In such cases, the doctor prescribes heparin or enoxaparin before surgery, and warfarin can be resumed after the procedure. On the day of the procedure, such a patient must donate blood for a coagulogram. The prothrombin time should be determined, even if the drug has been discontinued, to ensure that the blood level is low enough for surgery to proceed.
Parsa plasma vitrectomy is often performed in emergency cases when:
- treatment of rhegmatogenous retinal detachment;
- management of endophthalmitis;
- removal of intraocular foreign body.
Under these conditions, the procedure can only be contraindicated if the eye does not have light perception and restoration of vision is impossible.
What is the indication for vitrectomy?
Vitrectomy has opened up new opportunities in ophthalmology for the treatment of many diseases that were considered complex and previously untreatable. A person had to go blind with no hope of recovery. Among these diseases:
- the presence of an eye infection, which manifests itself in severe form;
- cases of retinal detachment due to: penetrating injury to the eye organ, as a result of diabetes mellitus, with a high degree of myopia (myopia), in the presence of sickle cell anemia, as well as due to physiological aging of the vitreous body in the eyeball;
- penetration of an otherworldly object into the eye organ;
- a hole or tear in the macula (macula);
- large retinal tear;
- there has been significant clouding in the structure of the vitreous body;
- hemophthalmos - the vitreous body is partially or completely saturated with blood;
- the presence of diabetes mellitus often causes the formation of retinopathy - damage to the blood vessels of the eye organ, which disrupts the blood supply to the retina;
- in cases of dislocation of the lens or intraocular lens, which was replaced during cataract surgery.
Repeated hemorrhages and gross opacities lead to scarring of the retinal tissue. These scars prevent a person from seeing clearly. The purpose of surgery is to remove them.
What can be a contraindication to vitrectomy?
Vitrectomy is a modern and unique method of surgical intervention, but not all patients can use it. Among the contraindications are: significant opacities of the cornea, allergic reactions to medications, the general serious condition of the patient, as well as problems with blood clotting, which can cause serious complications at the time of surgery and the postoperative period.
Anesthesia
In most cases, local anesthesia with intravenous sedation is appropriate. A retrobulbar block consisting of an equal mixture of short-acting lidocaine 2% and 0.75% can be used; longer acting bupivacaine.
Before performing a retrobulbar block, propofol may be prescribed by the anesthesiologist for short-term sedation (5-6 ml is usually sufficient).
In some cases, general anesthesia may be required. This should be considered by the anesthesiologist for pediatric patients and overly anxious patients. General anesthesia should also be given when the operating time is expected to be longer than usual or when the patient requests it.
Intervention Overview
This procedure involves removing all or part of the vitreous by cutting and sucking it out using tiny ophthalmic instruments that are inserted into the eye. Surgical removal of the vitreous is necessary for unobstructed access to the retina.
During the operation, the ophthalmologist acts on the retina with a laser, cuts out or removes scarred and pathologically altered tissue, gradually aligns its individual areas or restores holes in it.
Tools:
- Pneumatic high-speed vitreotome (disposable or reusable) – is a special cylinder with a knife (removes the vitreous slowly and in a controlled manner);
- Fiber optic luminaires;
- Infusion cannula (infusion port used to replace fluid in the eye with saline and maintain proper eye pressure);
- A 25 cm long flexible tube is attached to the infusion source.
Patients may experience mild discomfort for a few days after the procedure. The removed vitreous does not grow back, but is replaced by fluid that is normally produced by the eye. This gel is very important during eye development, but is not essential for eye health or focus after birth.
Although the results of vitrectomy vary depending on the individual condition, most patients experience improvement in visual acuity after this procedure.
The surgery is considered safe, but there are certain risks associated with any surgical procedure. Some of these include retinal detachment, fluid build-up, new blood vessel growth, infection, and further bleeding (hemophthalmos). Cataract formation often accelerates in patients who have not previously had cataract surgery.
Vitrectomy of the eye
Vitrectomy of the eye is a surgical procedure during which the vitreous body, which occupies most of the organ, is removed from the eye organ. Depending on the affected area, the body may be partially or completely removed. Partial removal is called subtotal vitrectomy. Complete removal of the vitreous body - total vitrectomy.
Removal of the vitreous body allows the ophthalmologist to gain access to the retinal tissue and perform:
- photocoagulation (a kind of soldering of the retina);
- reproduce the restoration of the integrity of the shell, which could be damaged when receiving a serious injury;
- move the formed scar tissue from the surface of the retina that interferes with the eye organ.
Simultaneously with these procedures, additional ones can be carried out (we will consider further).
The removed vitreous body is replaced with silicone oil or a gas mixture - special means that ensure close contact between the retina and the choroid, and also minimize the risk of postoperative complications.
Important: Today, vitrectomy is the only way to solve problems associated with eye disease. These are various hemorrhages, retinal detachment or injury to the visual analyzer.
Such an operation requires not only the use of high-tech equipment, but also highly qualified doctors.
Requirements
- The patient should stop taking indirect anticoagulants.
- During surgery, it is necessary to maintain adequate homeostasis and control intraocular pressure so as not to cause choroidal hemorrhage.
- Before the procedure, you should rinse thoroughly with a diluted povidone-iodine solution.
- A subconjunctival or topical antibiotic should be administered before surgery is completed. The doctor prescribes antibiotic eye drops to the patient, which must be used for at least 1 week.
Microinvasive vitrectomy
This ophthalmic operation involves the extraction (removal) of a small part or the entire vitreous. It is carried out through 3 main punctures measuring 0.3-0.5 mm. The peculiarity of this intervention is that the surgeon inserts much smaller instruments into the eye, while the operating frequency of a pneumatic or electric vitreotome during this procedure is much higher by 2 times - not 2500 per minute (as usual).
Microinvasive vitrectomy is performed using special self-fixing multipoint lamps.
Advantages:
- less traumatic;
- significantly reduces the risk of intra- and postoperative bleeding;
- can be carried out on an outpatient basis, this does not require hospitalization of the patient in a hospital;
- usually performed under local anesthesia with sedation (the patient is awake during the procedure, but does not feel pain or see the procedure being performed);
- patients go home with a patch on the eye, which is removed in the doctor's office the day after surgery;
- The duration of the rehabilitation period has been significantly reduced.
The duration of the operation varies from one to several hours, depending on the patient's condition. In certain situations, your doctor may perform other surgery, such as cataract removal.
Progress of the operation
- The vitreous body is removed.
- All existing scar tissue is eliminated (it is necessary to return the retina to its normal physiological position).
- A bubble of air or gas is placed in the patient's eye to help the retina stay in the correct position. The bubble is not removed, it will gradually disappear on its own.
- A special fluid (such as silicone oil) is then injected, which is later removed from the eye through another surgery.
- The silicone is removed as soon as the cornea heals.
Additional steps of the operation
In addition to the actual removal of all or part of the vitreous, the operation may include additional surgical steps.
- Excision and removal of the epiretinal membrane (membranectomy) is a pathological growth of tissue in the macula area that occurs as a result of detachment of the vitreous body of the retina, after an intraocular infection or certain surgical interventions.
- Injecting air into the eye to remove fluid from the back of the eyeball while maintaining a level of intraocular pressure that keeps the retina in position or seals pathological holes in the retina.
- Injection into the eye of a gas-air mixture, most often containing sulfur hexafluoride, octafluoropropane. Due to the fact that the gas is mixed with air, its side effects on the eye are neutralized. This mixture provides a reliable tamponade of the retina during retinal detachment and holds it in place, preventing fluid from leaking through holes in the retina. After some time (from 2 weeks to 2 months), the gas-air mixture gradually leaves the eye cavity, being replaced by its own intraocular fluid.
- Injection of silicone oil or saline solutions into the eye is used to securely fix the retina to the underlying tissues of the eyeball. Silicone oil is an inert substance, so it can remain in the eye for quite a long time, usually for two to three months, but according to indications this period can be extended to several years. After this, the silicone oil should be removed from the eye.
- Laser photocoagulation of the retina allows you to reliably attach individual areas of the retina and seal holes and areas of thinning of the retina. In addition, the method is used to treat pathologically altered defective vessels that occur in patients with diabetes and macular degeneration.
- Scleral strapping is an additional manipulation that involves installing a supporting silicone pad in the form of a soft sponge at the site of retinal detachment to prevent further retinal detachment.
- Removal of the clouded lens, performed simultaneously with vitrectomy.
As a rule, the operation is performed under general anesthesia (with the exception of anterior vitrectomy), because The slightest movement of the patient (if he is conscious) can lead to trauma to the retina by surgical microinstruments.
Postoperative period
The patient may experience slight discomfort during rehabilitation. Doctors recommend wearing a special bandage and avoiding any strain. For some, the doctor prescribes painkillers after surgery.
If a gas bubble has been placed in the eye, the specialist may recommend that the patient keep his head in a special position for some time. With a gas bubble or other substance in the eye, vision will be blurred. There are certain limitations after microinvasive vitrectomy. The patient is advised not to fly in an airplane or travel at high altitudes until the gas bubble disappears.
After the operation, it is prohibited for 6 months:
- lift weights more than 2 kilograms;
- visit the solarium;
- throw back your head and look up for a long time;
- read books and write for more than 30 minutes;
- stand near an open fire or lean over a fire (this includes a gas stove);
- rub your eyes and press on the eyeball;
- engage in professional sports;
- watch TV or work at the computer for a long time;
- bend over;
- exercise intensively;
- visit the bathhouse and sauna;
- You can wash your hair, but very carefully and avoid getting shampoo and soap into your eyes;
- In summer you need to wear sunglasses, you can’t look at the sun.
Source: glazexpert.ru