Nylon 10/0 (to sew the cornea)
Last chance surgery or corneal transplant requires donor tissue.
Specifically, we are interested in tissue with a thickness of 500–600 microns for penetrating keratoplasty. Next, you need to work with this film by hand, sewing with thin nylon thread. Then, when the cornea grows together, remove the suture. No biodegradable materials - their breakdown products will begin to lyse and can cause inflammation, which will exclude a positive result of the operation. Moreover, it is recommended to stitch the graft around the perimeter twice - this increases the chances of its correct and uniform fixation. The second layer of nylon is most often not removed at all, because as long as it doesn’t interfere, we don’t touch it.
But let's start from the beginning. Specifically, in situations where a person may need this operation, which is difficult for Russia, but completely familiar in Germany. It comes in three types:
- Through, that is, removal of the patient’s entire cornea, for example, with a diameter of 7 to 8.5 mm and sewing on a new one.
- DALK, that is, transplantation of corneal tissue excluding Descemet's membrane and endothelium.
- DMEK, that is, “installation” of only a layer of Descemet’s membrane and endothelial cells instead of the same layer in the patient.
Keratoplasty in Germany is a very common operation. In our clinic in Marburg, my head of department and I performed 210 transplants last year, and the year before that - 236 transplants. Since March of this year, at the Moscow SMILE EYES clinic, we began transplanting corneal tissue - both layer-by-layer and end-to-end transplants.
Types of keratoplasty
Complete transplant
It may be required if both the outer and inner layers of the cornea are damaged. This is called penetrating keratoplasty (PK) or full thickness grafting. The diseased or damaged cornea is removed. A clear donor cornea is then sutured in its place. Despite the greatest trauma of all options, this is the simplest version of keratoplasty.
PC has a longer recovery period than other types of corneal transplants. Restoring full vision after PC may take up to one year or longer.
There is a higher risk of graft failure with PC than with other types of corneal transplants.
Partial corneal graft transplantation
Sometimes only the anterior and middle layers are damaged. In this case, only these layers are deleted. The endothelial thin posterior layer remains in place. This graft is called deep anterior lamellar keratoplasty (DALK) or partial thickness corneal transplant. DALK is usually prescribed to treat keratoconus, or corneal bulge.
Healing time after DALK is shorter than after full corneal transplantation. There is also less risk of rejection of the new cornea. This operation is more complex, and is performed in only a limited number of clinics in the CIS.
All modern cornea transplant operations are performed in Belgium, including DALK. In some clinics, the intervention is performed using a femtosecond laser, which makes it safer.
Deep anterior lamellar keratoplasty (DALK) involves excision of the cornea down to the level of Descemet's membrane. A blind corneal disc is formed on the recipient's eye. A cut-out end-to-end donor disc without endothelium is placed on the recipient's Descemet's membrane, freed from the surface layers of the stroma, and fixed with sutures. The main advantage of the method is considered to be the minimal risk of graft rejection.
After DALK, the graft becomes transparent already 3-5 days after surgery. The operation provides better functional results: after engraftment of the graft, visual acuity of 0.7-0.9 is achieved, and some patients receive one hundred percent vision.
Corneal transplant operations are performed at the Saint-Jean Clinic by a team of doctors led by Dr. Jérôme Vryghem. This specialist performs more than 2 thousand ophthalmological interventions every year. Since 2007, he has been one of the first in Belgium to use the femtosecond laser. This technology makes it possible to make more precise cuts in the corneal tissue in any way. The femtosecond laser makes it possible to take an individual approach to the choice of surgical procedure.
Endothelial keratoplasty
In some eye diseases, the innermost layer of the cornea, called the “endothelium,” is damaged. This causes swelling of the cornea, which affects your vision. Endothelial keratoplasty is a surgery to replace this layer of the cornea with healthy donor tissue.
The damaged layer of the cornea is removed through a small incision. The new fabric is then placed in place. Only a few stitches, if any, are required to close the incision. Most of the cornea remains intact. This reduces the risk of new corneal cells being rejected after surgery.
There are two types of endothelial keratoplasty.
- DSEK (or DSAEK) - endoscopic Descemet's membrane keratoplasty (automated). In DSEK/DSAEK surgery, the donor tissue is easier to graft and position because it is thicker than the donor tissue in DMEK surgery. Therefore, this operation is more common.
- DMEK - Descemet's membrane endothelial. In DMEK surgery, the donor tissue is thin and may be more difficult to graft. But recovery is faster and the long-term results of the operation are better because the graft tissue is thinner. But this operation is performed abroad only in ophthalmological centers with the highest level of technical equipment and training of surgeons. In Belgium, this method has been introduced since 2012.
Artificial corneal implant
In this type of surgery, an artificial flexible keratoprosthesis is implanted into the corneal pocket using a minimally invasive procedure.
There is a large discrepancy between the availability of corneal tissue for transplantation and the number of patients requiring corneal transplantation. Artificial implants can solve this problem. But only in the last few years have they been able to provide levels of vision restoration comparable to donor corneas.
Nowadays, in patients at high risk of rejection with a human donor, a keratoprosthesis can provide good visual results with a good risk-benefit ratio.
Bionic corneal implant
This is an innovative method that is just entering the practice of leading ophthalmological clinics in Europe. A corneal prosthesis is created by 3D printing from decellularized corneal stroma and stem cells.
This cornea is completely biocompatible, and 3D cell printing technology allows the microenvironment of the cornea to be reproduced. As a result, the transparency of the implant is similar to that of the human cornea.
Donor material
The donor disc is taken from corpses no later than 24 hours after death. The flap is cut out to be as large as possible and only before transplantation does it acquire the required shape and size. It must be preserved in a container with a special medium and its storage time should not exceed 5-7 days. All trephines are stored in eye banks at large ophthalmological centers.
The corneal flap is checked for the presence of infectious processes, microscopy is performed, and optical purity and viability are established. Each eye bank has waiting lists with recipient details. When the necessary material becomes available, the candidate is urgently called for a surgical procedure. Material is not collected from newborns and elderly people (over 70 years old).
Transplantation is contraindicated if the donor has the following diseases:
- Hepatitis B;
- Retinoblastoma;
- Bacterial/fungal keratitis;
- Bacterial/fungal endophthalmitis
- HIV;
- Herpes simplex virus;
- Hepatitis C;
- Human T-cell lymphotrophic virus;
- Ocular adenocarcinoma;
- Malignant tumors of the segment;
- Reye's syndrome;
- Subacute sclerosing panencephalitis;
- Progressive multifocal leukoencephalopathy;
- Leukemia;
- Active disseminated lymphomas;
- Active infective endocarditis;
- Active septicemia;
- Dementia of unknown cause;
- Down syndrome;
- Congenital rubella.
Indications and contraindications
Indications for transplantation by prevalence
- corneal ulcers - 25.8%;
- keratoconus -21.1%;
- keratopathy - 19.1%;
- previous unsuccessful transplantation - 10.2%;
- non-herpetic scar of the cornea - 9.8%;
- stromal corneal dystrophies - 2.9%;
- pellucid marginal degeneration (PMD) - 2.7%;
- traumatic corneal opacity - 2.3%;
- thin Descemet's membrane - 1.9%;
- postherpetic scar of the cornea - 1.8%.
Other indications included corneal endothelial dystrophy, post-laser in situ keratomileusis, (LASIK) keratectasia, corneal fibrosis and anterior segment dysgenesis.
The main indication for the use of an artificial implant is multiple previous failures of using a donor graft. In addition, an artificial corneal prosthesis is indicated for conditions such as severe ocular surface disease, chemical burns, Stevens Johnson syndrome, limbal stem cell deficiency, congenital aniridia, or dry eyes.
Contraindications
There are absolute and relative contraindications for corneal transplantation in each country, which vary greatly by region. The National Health Agency for blood and transplant testing in Belgium has the following absolute contraindications:
- the graft will not be able to restore the function or integrity of the cornea;
- surgery can lead to anatomical disruption of the structures of the eye, which will lead to loss of vision.
Relative contraindications include:
- mental illness;
- eye infections;
- acute conditions in chronic diseases;
- and etc.
Preparing for surgery
The most important thing in preparing for a transplant is finding a suitable donor cornea.
There are 4 cornea donor banks in Belgium - in Leuven, Liege, Ghent and Antwerp. All these banks are in close contact with each other. As a result, in Belgium the patient does not wait for a donor cornea to appear - it will always be found in one of the banks and will be used regardless of the choice of clinic for the operation.
Other preparations for surgery include a set of general tests and an assessment of the compatibility of medications taken with the upcoming procedure (for example, taking anticoagulants).
Progress of the operation
- Eye drops will be put into your eyes. You may be given another medicine to help you relax.
- The ophthalmologist may use local or general anesthesia to prevent the patient from feeling pain. During local anesthesia, sedatives may be used to provide additional relaxation.
- A retainer is then applied to keep the eye open. Even if the eye is open, the patient sees very little or nothing at all due to the anesthesia.
- The surgeon will then choose how to transplant the healthy donor cornea based on the patient's specific needs. In some cases, the entire thickness of the cornea is removed and a donor graft is sutured in its place.
- Sometimes only a very thin outer layer of cells is removed from the cornea, and donor tissue is placed in its place and secured with several sutures.
- In other cases, only the inner layer of the cornea is removed and a thin disk of healthy donor tissue is placed on the back of the cornea. An air bubble is then inserted into the eye, pressing this new layer of cells into the surgical site so that the cornea can heal properly.
Surgical technique (by R.MELLES)
- A superficial scleral pocket is formed, just as with phacoemulsification, and the anterior chamber is filled with air;
- Lamellar dissection occurs throughout almost the entire cornea. The depth of dissection in this case corresponds to the zone of internal reflection above the dissector, and should be twice as thick as the underlying stroma;
- The dissected space is expanded by introducing viscoelastic;
- The surface layers of the cornea are removed with a trephine;
- The viscoelastic is washed out and air is removed from the anterior chamber;
- After removal of the endothelium, a full-thickness donor flap is sutured into place.
Postoperative management of the patient is identical to penetrating keratoplasty, except for the reduced need for topical steroids and the option after 6 months. removing stitches.
Rehabilitation after surgery
The day after your corneal transplant surgery, you will need to return to your ophthalmologist's office to have your eye examined.
Sutures from surgery may or may not be removed. It depends on how quickly you heal, the health of your eyes, and the type of stitches used.
During the rehabilitation period, the following rules must be observed:
- Use eye drops exactly as prescribed by your ophthalmologist.
- Do not press or rub your eye.
- If necessary, you can take an over-the-counter pain reliever.
- Wear goggles or a face mask to protect your eyes.
- Talk to your eye doctor about when you can return to your normal daily routine.
- Depending on the type of transplant, you may need to lie on your back for a while after surgery. This helps the new donor tissue stay in place.
Depending on the type of transplant and how the eye heals, it may take a year or more to fully recover from this surgery.
Possible complications
Organ rejection is when the body's immune system sees the transplanted tissue as foreign and tries to get rid of it. Rejection is a problem for 3 out of 10 people who have a corneal transplant.
Warning signs that corneal rejection is developing include:
- eye pain;
- increased sensitivity to light;
- redness of the eyes;
- cloudy or hazy vision.
Sometimes cornea transplant surgery can cause other eye problems, such as:
- infection;
- bleeding;
- retinal disinsertion;
- glaucoma (due to increased pressure inside the eye).
Even when a corneal transplant works as expected, other vision problems can limit the quality of your vision. For example, the new cornea may not curve evenly (astigmatism). Or you may have an eye disease such as macular degeneration, glaucoma, or diabetic retinopathy. Due to such problems, vision after keratoplasty is not restored 100%.
You may also need more than one corneal transplant. The first transplant may result in rejection.
However, repeat transplants have a higher rejection rate than the first transplant.
Anatomical and physiological features
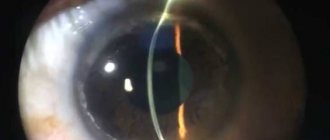
The cornea is the outermost transparent layer of the eye, located just in front of the anterior chamber, iris, and pupil. It has the appearance of a spherical membrane, borders the sclera on the limbus and is involved in the refraction of light. Five distinct layers make up its microstructure, including the epithelium, Bowman's membrane, stroma, Descemet's membrane, and endothelium.
In addition to protecting the eyeball from aggressors and ultraviolet radiation, it is responsible for approximately 65%-75% of light refraction.
Tears, due to their lipid, water and mucin components, are important for maintaining her health as they help keep the surface moist and clean.
The primary purpose of the epithelium is twofold: to prevent the penetration of foreign objects or substances and to ensure the absorption of vital components from tears (for example, oxygen).
Bowman's membrane consists of thin, transparent collagen. Injury or disease can disrupt this collagen film and cause scarring, which impairs visual perception. It all depends on the location of the pathological focus and the degree of trauma.
The stroma is the thickest section. It consists of water and collagen, which is especially important for maintaining a spherical shape, which ensures the correct passage and refraction of light.
Descemet's membrane is another thin part, but quite strong due to the collagen fibers. This collagen is produced by endothelial cells. This structure is capable of repairing itself after injury and is critical for protecting internal microstructures from infection and injury.
The inner layer is the endothelium. It plays a vital role in maintaining transparency through the pumping action of endothelial cells when excess fluid emerges from the stroma. Endothelial parts practically do not regenerate, and their destruction can cause long-term dysfunction.
Because of the importance of transparency, corneal tissue does not contain blood vessels. It receives nutrients through the diffusion of tear fluid on the outside. The epithelium contains thousands of nerve endings, which make it highly sensitive to aggression or contact with foreign objects. Long ciliated nerve fibers arising from the trigeminal nerve (V1) provide sensory innervation. The average density of nociceptors in corneal tissue is 300-600 times higher than the density of skin. The ciliary nerves form the middle, subepithelial/subbasal and epithelial networks.
Cost of the operation
For an operation such as a cornea transplant, the cost largely depends on the type of intervention and the type of cornea being transplanted.
High-quality artificial implants, whose characteristics approximate the donor cornea, are very expensive. Therefore, this operation can be 2-2.5 times more expensive than with donor material.
As a result, for an operation such as eye keratoplasty, the price in Belgium will be approximately 20-25% lower than in Germany or Israel and approximately 40% lower than in the USA
The average price for corneal transplantation in Belgium is between 5000-7500 €.
Advantages of performing keratoplasty in our ophthalmology center
The equipment of our eye clinic meets international standards of modern medical technology. Tools and consumables meet all sanitary requirements and have quality guarantees confirmed by certificates and permits. The methods used have undergone clinical trials and confirmed their effectiveness and safety. Our patients have access to the most gentle technology for keratoplasty – using a femtosecond laser. The likelihood of complications and scar formation is an order of magnitude lower than after using a micro-tool.
Doctors at our center have constant access to a bank of biomaterial. There is no need to wait for a transplant, so the possibility of treatment depends only on medical indications and the patient’s readiness.
Keratoplasty is performed by experienced, highly qualified ophthalmic surgeons who are constantly improving their skill level. Doctors of our center take part in scientific conferences and practical seminars, supporting the work of our eye center at the high level of current world medicine.
The effectiveness of keratoplasty treatment performed in our eye clinic is always predictable. The risk of complications is minimized, since even junior medical personnel involved in preparing the patient for surgery and staying with the patient in the first hours after surgery have unique experience. Each employee is interested in the high reputation of the clinic, responsibly fulfills the duties assigned to him and is responsive to any comments from visitors. The qualified assistance and successful results are confirmed by numerous reviews from our grateful patients.