General information
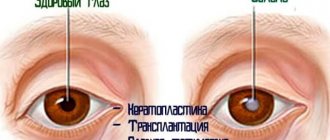
An eyesore , or so-called leukoma , is a persistent clouding of the ocular cornea with the formation of whitish vascularized spots.
According to ICD-10, the code is assigned: H17 Scars and opacities of the cornea, including adhesive leukoma (H17.0), other central opacities of the cornea (H17.1), other scars and opacities of the cornea (H17.8) and scars together with corneal opacities of unspecified etiology (H17.9). It is important to distinguish a cataract from a cataract , which is clouding of the structures of the lens - one of the parts, the superficial bag, or the whole. Spots that form a cataract - maculae corneae (translated as spots of the cornea) involve exclusively the cornea in the pathological process. It is impossible to overestimate its importance for vision and vital functions of the human body. The cornea is the lens of the eye that transmits and refracts light, helps in the supply of nutrients, protects from external negative influences - pollution, temperature and infections, therefore it is necessary to monitor its health and treat inflammation of any origin in a timely manner.
Structure of the cornea
Treatment protocols
TREATMENT AT THE INPATIENT LEVEL Treatment tactics Non-drug treatment: General regimen 3, table No. 15. Drug treatment (depending on the severity of the disease): List of essential medications
| Medicine (international nonproprietary name) | Pharmacological groups | Method of administration | Single dose | Frequency of application | Duration of treatment | Level of evidence | |
| Dexamethasone ophthalmic suspension 0.1% 5 ml [3] | Glucocorticoids for local use in ophthalmology | Instillation into the conjunctival cavity | 2 drops | 4-6 times a day after surgery and then in a decreasing pattern | 3 weeks | IN | |
| Levofloxacin eye drops 0.5% 5 ml [3] | Antimicrobial drug of the fluoroquinolone group for topical use in ophthalmology | Instillation into the conjunctival cavity | 2 drops | 6 times a day | 10 days | IN | |
| Sulfacetamide eye drops 20%, 30% 15 ml [3] | Antimicrobial bacteriostatic agent, sulfonamide | Instillation into the conjunctival cavity | 2 drops | 6 times a day | 5 days | IN | |
| Midrimax eye drops 5 ml (UD - B) [3] phenylephrine hydrochloride 50 mg, tropicamide 8 mg | M-anticholinergic | Instillation into the conjunctival cavity | 2 drops | 3 times a day | 5 days | IN | |
| Proximetacaine (Proparacaine) eye drops 15 ml (UD - B) [3] | Local anesthetic | Instillation into the conjunctival cavity | 2 drops | 1 time | 1 day | WITH | |
| Dexamethasone 0.4% 1 ml (UD - B) [3] | Glucocorticoids for systemic use | Parabulbar or subconjunctival injections | 0.5 – 1.0 ml | 1 time | 4 days | IN | |
| sodium hyaluronate (UD - B) [3] | tear film protector | Instillation into the conjunctival cavity | 2 drops | 3-4 times a day | 1-2 months | IN | |
List of additional medicines:
| Medicine (international nonproprietary name) | Pharmacological groups | Method of administration | Single dose | Frequency of application | Duration of treatment | Level of evidence |
| Tobramycin eye drops 5 ml (UD - B) [3] | Antimicrobial drug of the aminoglycoside group for topical use in ophthalmology | Instillation into the conjunctival cavity | 2 drops | 6-8 times a day | 10 days | IN |
| Ceftriaxone (UD - B) [3] | antibiotics cephalosporins | intramuscular injections | 1.0 g | 1-2 times a day | 5-7 days | IN |
| Gentamicin 2ml (UD - B) [3] | antibiotics aminoglycosides | intramuscular injections | 80 mg | 2 times a day | 5-7 days | IN |
| Timolol eye drops 0.5% | B-blocker | Locally into the conjunctival cavity | 2 drops | 2 times | Up to 7 days | IN |
| Atropine sulfate 1 ml 1 mg\ml | Belladonna alkaloid, tertiary amines | Intramuscularly | 1 ml | 1 time | 1 day | IN |
| Tramadol 1 ml | Opioid narcotic analgesics | Intramuscularly | 1 ml | 1 time | 1 day | IN |
| Diphenhydramine 1 ml | Antihistamine | Intramuscular - premedication Intravenous - ataralgesia | 0.3 ml 0.5 ml | 1 time 1 time | 1 day | IN |
| Fentanyl 0.005% 1 ml | Analgesic. Opioids. Phenylpiperidine derivatives | Intravenously | 1.0 ml | 1 time | 1 day | A |
| Propofol emulsion 20 ml | Anesthetics | Intravenously | 200 mg | 1 time | 1 day | A |
| Lidocaine 2% | Local anesthetic | For parabulbar and subconjunctival injections | 0.5 ml | 1 time per day | 4 days | IN |
| Prednisolone 30 mg/ml | Glucocorticosteroids | Intramuscularly | 60 mg | 1 time per day | 5 days | IN |
| Promedol 1 ml | Anesthetics | Intramuscularly | 1.0 ml | 1 time | 1 day | IN |
Surgical intervention provided in an inpatient setting (UD - B) [3,5,6,7,8]: Corneal transplantation (penetrating keratoplasty, lamellar keratoplasty) Purpose: optical. Indications: corneal scars, corneal opacities. Contraindications: · high risk of rejection of the donor cornea due to autoimmune diseases; · inflammatory diseases of the eyeball; · gross pathology of the posterior segment according to ultrasound (subatrophy of the eyeball, retinal detachment); · lack of indicative VIS, optic nerve conduction according to EPI data. Penetrating keratoplasty Local anesthesia, premedication. General anesthesia is used in children and adult patients with increased nervous excitability. Treatment of the surgical field 3 times with a 5% chlorhexidine solution. Retrobulbar anesthesia is performed with a 2% solution of novocaine 2.5 ml, akinesia with a 2% solution of lidocaine 4.0 ml, epibulbar anesthesia (proximetacaine, oxybuprocaine) 3 times. A stay suture is placed on the episclera at 12 o'clock. A through graft is cut out from the donor material using a BARRON Vacuum Donor Cornea Punch trephine with a diameter of 5 to 10 mm (depending on the diameter of the corneal opacification). A Radial Vacuum Trephine with a diameter of 5 to 10 mm (depending on the diameter of the corneal opacities) is used to cut out a disc of the recipient's cornea. The donor's graft is sutured with 4 provisional knots and fixed to the prepared bed with a continuous 10/00 suture. Antibacterial drops are instilled into the conjunctival cavity. Monocular aseptic dressing. Layer keratoplasty Local anesthesia, premedication. General anesthesia is used in children and adult patients with increased nervous excitability. Treatment of the surgical field 3 times with a 5% betadine solution. Retrobulbar anesthesia is performed with a 2% lidocaine solution 2.5 ml, akinesia with a 2% lidocaine solution 4.0 ml, epibulbar anesthesia (proximetacaine, oxybuprocaine) 3 times. A stay suture is placed on the episclera at 12 o'clock. A graft covering 2/3 of the corneal thickness is cut out from the donor material using a trephine with a diameter of 5 to 10 mm (depending on the diameter of the corneal opacification). Using a trephine with a diameter of 5 to 10 mm (depending on the diameter of the corneal opacities), a disc of the recipient's cornea is cut out to 2/3 of its thickness. The donor's graft is sutured with 4 provisional knots and fixed to the prepared bed with a continuous suture. Antibacterial drops are instilled into the conjunctival cavity. An aseptic monocular dressing is applied. Indications for consultation with specialists [2,3]: · consultation with a therapist – no exacerbation of chronic diseases, contraindications to surgical treatment; · consultation with an otorhinolaryngologist – no exacerbation of chronic diseases, contraindications to surgical treatment; · consultation with a dentist – no exacerbation of chronic diseases, no contraindications to surgical treatment; · consultation with an infectious disease specialist - in case of positive tests for specific infections or an indication of the infectious etiology of the origin of the cataract. An infectious disease specialist’s conclusion about the absence of an active process at the moment, the absence of contraindications to surgical treatment; · consultation with a rheumatologist - if the patient has a concomitant pathology (systemic diseases, collagenosis) - a conclusion about the absence of an active process at the moment, the absence of contraindications to surgical treatment. Indications for transfer to the intensive care unit: none. Indicators of treatment effectiveness (UD - B) [5,6,7,8]: transparent engraftment of the corneal graft; · improvement of visual functions.
Pathogenesis
The formation of a cataract is always preceded by some kind of damage: a wound, ulceration, thinning or inflammation of the cornea of various origins, which leaves behind a scar . During the scarring process, the transparency of the membrane and its ability to transmit light rays are impaired. Most often, the spot forms a dense and thick porcelain-white color, which can change color over time due to the growth of a network of blood vessels - pannus of the eye , which is an abnormal transition of inflammation from the conjunctiva as a result of trachoma , tuberculous or allergic keratitis, most often in childhood. Vascular ingrowth (pannus), with varying degrees of vascularization and infiltration, can be thin, vascular or fleshy.
In the end, the thorn disrupts the permeability of the shell, fatty (hyaline) degeneration occurs and a yellowish tint appears.
The most severe course is considered to occur with the formation of central opacities of the cornea opposite the lens. It leads to a sharp decrease in visual acuity and even blindness.
Treatment of corneal opacities
Treatment of corneal opacities is complex and may consist of the following areas:
- Anti-inflammatory drugs.
- Subconjunctival injections to accelerate the resorption of cloudiness.
- Hormonal eye drops and ointments.
- Physiotherapeutic treatment (for example, electrophoresis with aloe extract).
- Surgical treatment (phototherapeutic keratectomy, layer-by-layer or penetrating keratoplasty).
Phototherapeutic keratectomy
— evaporation of the surface layer of the cornea with clouding using a laser device.
Keratoplasty
— partial (layer-by-layer) or complete (end-to-end) transplantation of the donor cornea to remove deep opacities. The method is the only treatment option for corneal thorn.
Read us on Yandex. Zen
Classification
A cataract can be congenital or acquired and vary significantly depending on shape, size, and color. The reason for this is the characteristics and localization of previous inflammatory processes, and transitions from completely opaque to transparent occur quite often. Leukoma can be complicated by fusion with the iris, protrusion (ectasia), lens opacification, secondary cataracts, glaucoma , astigmatism , macular edema, retinal detachment, and eye atrophy.
Depending on the scale of pathogenesis, the cataract looks like a small speck, a cloud, or a complete and total lesion. They come in different categories:
- I – through cataract, central location, no vascular network, intensity and etiology may be different, the sphericity of the cornea is not impaired, and the radius size does not exceed 3 mm;
- II – spots may have a central or paracentral location, pannus or synechiae are not formed, correct sphericity is maintained, the radius size is more than 3 mm;
- III – vascular cataract (pannus of the eye is revealed), it can be fused or unfused, with keratoconus , of various sizes, sphericity is preserved, intraocular pressure is normal;
- IV – large-scale damage, occupying more than 80% of the surface, developing as a result of burns , neutrophic keratitis and other reasons;
- V – pathology leads to deep amblyopia , can be combined with glaucoma, most often these are scars after chemical burns, xerosis, size 6-7 mm, dystrophic processes can lead to significant changes in the fundus, conjunctival growths, vascularized adhesions, development of fistulas, staphyloma, buphthalmos.
In addition, it is customary to classify albugo spots as a separate variety. They are distinguished by a special pearl color and some limitedness.
Treatment
To understand how to treat leukoma, it is necessary to determine the degree of its localization:
- If the clouding does not affect the clarity of the eyeball, and the ability to see has not deteriorated, then drug treatment is not resorted to. In this case, the cloudiness is removed surgically.
- If the inflammatory process is moderate, then therapy is aimed at eliminating it. For the treatment of keratitis, an individual program is selected, which necessarily includes anti-inflammatory drugs. Inflammation is relieved by corticosteroid drugs, such as hydrocortisone or Dexamethasone.
In the treatment of cataracts, absorbable drugs are often used, for example, yellow mercury ointment or dionin. Lidaza is effective for resorption - used for electrophoresis. If there is a trophic lesion of the epithelium, then Solcoseryl (eye gel) is prescribed.
- If the clouding is significant, drastic intervention is required - keratoplasty . This operation involves transplanting clear areas of the cornea from a donor. After transplantation, antimicrobial therapy is carried out and glucocorticoids are prescribed. This is necessary for better engraftment. If transplantation is not possible, the affected area is replaced with a corneal implant. This process is called keratoprosthesis.
Keratoplasty: before and after photos
- Physiotherapeutic methods are often used in the treatment of leukoma. One of them is diathermy . During this procedure, the tissue is exposed to high current and high frequency alternating current. Diathermy produces a complex effect, including the resorption of infiltrates, scar tissue, and swelling. This therapy promotes the resorption of blood in the vitreous body and its clearing.
Diathermy of the eye
- Another physiotherapeutic method used in the treatment of leukoma is iontophoresis (electrophoresis). With the help of various electrical currents, medications enter the body, penetrating the skin and mucous membranes. The features of the method ensure uniform distribution of the drug while maintaining maximum concentration in the desired area. Iodine solutions are usually used in the treatment of leukoma.
Iontophoresis
Causes of eyesore in humans
Cloudiness of the cornea in humans usually occurs as a result of inflammation of the cornea of the eye - deep or superficial keratitis. In this case, the reasons for the appearance of eyesores can be:
- mechanical (burn, superficial injuries caused by foreign bodies, chemicals or rays);
- infectious - caused by the influenza virus, Koch's bacillus, Pseudomonas aeruginosa, Staphylococcus aureus, fungi, amoebae;
- as a complication of conjunctivitis and any other diseases that can affect the layers of the cornea (for example, trachoma);
- In addition, there are known cases of cataract formation after suffering from syphilis and chlamydia , the fundamental factor being their inadequate or ineffective treatment.
Stages of formation of an eyesore as a result of keratitis
People at risk of developing eyesores include:
- using lenses , especially if hygiene rules are not followed;
- having problems with intraocular pressure ;
- staying for a long time in the scorching bright sun;
- those who have undergone eye surgery, for example, removal of pterygium , cataracts, etc.;
- working with welding equipment;
- visiting saunas and bath complexes where high temperatures are used;
- genetic predisposition and congenital diseases that provoke clouding of the cornea, for example, blenorrhea .
Prevention
In order to prevent leukoma, it is important to promptly contact an ophthalmologist in case of any symptoms or external changes.
- It is important to observe safety precautions in production, and to use protective equipment when working with active chemicals (acids, alkalis).
- It is necessary to promptly and completely treat any infectious and inflammatory diseases.
With timely treatment and compliance with preventive measures, treatment of leukoma is possible and very effective.
Related articles:
- Dry eye syndrome: symptoms and treatment
- Ophthalmoplegia
- Demodicosis of the eye (eyelid) in humans: symptoms and treatment, photo, massage
- Watery eyes: causes and treatment in adults, children
Symptoms
Leukoma can begin with inflammation of the cornea - keratitis, injury or inflammation that causes symptoms such as:
- lacrimation;
- blepharospasm and spasm of accommodation ;
- photophobia;
- pain;
- nystagmus;
- sensation of the presence of a foreign body or a veil before the eyes;
- blurred vision;
- decrease in transparency, loss of shine and acquisition of a porcelain-white color by the cornea, which can be visually seen with the naked eye.
Subsequent ulcerations and scarring cause clouding of the cornea and can lead to serious complications, even partial or complete loss of vision. In general, the quality of vision directly depends on the location and extent of corneal damage. If the spots and scars are small in size and located on the periphery, then a person may not notice the development of a cataract for a long time. At the same time, in addition to discomfort and deterioration of vision, people are more concerned about cosmetic defects.
Tests and diagnostics
A routine examination by an ophthalmologist begins with an examination of the patient and a full study of his medical history, complaints and existing symptoms. During an external examination, if it is possible to identify roughness or unevenness, a whitish lesion, then visometry, tonometry, ophthalmoscopy, biomicroscopy and check the reflexes of the fundus should be performed. Research makes it possible to assess the pressure, size and transparency of the spot, depth and scale of the lesion.
If there is a suspicion that other structures of the eye or nervous system are involved in the pathogenesis, then additional ultrasound and computed tomography may be advisable.
Treatment with folk remedies
Traditional medicine offers its own ways to combat leukoma (eyesore). Most often they are infusions for washing, eye drops or applying compresses. In this case, it is very important to prepare sterile solutions, use pharmaceutical herbal raw materials, clean dishes and gauze for filtering, and store infusions, if necessary, in a cool, dark place. Most popular recipes:
- take the dried herbs of blue cornflower, arnica, eyebright and black elderberry - mix in equal proportions and pour 200 ml of boiling water, filter after 2 hours;
- take 1 teaspoon each of plantain and cumin - pour 200 ml of boiling water, filter after a couple of hours;
- instillation of resin (resin from coniferous trees), pike bile, red onion juice with May honey - no more than 1 drop per day;
- washing the eyes with freshly brewed tea leaves, it is best to use natural loose leaf tea.
In children
The cause of the development of cataracts in newborn children may be blenorrhea - purulent or other inflammation of the conjunctiva of the eye and cornea, suffered in the womb. Most often, the disease is initiated by gonococci, infection occurs from a mother with gonorrhea , at the stage of the baby passing through the birth canal. Already on the 2-3rd day, children experience severe swelling of the eyelids, then on the 6-7th day of life, a large amount of pus begins to be released. If the cornea is involved in pathogenesis, then ulcers form on it, the healing of which leaves behind scars and clouding of the cornea, that is, it provokes the development of a cataract. Most often combined with eye pathologies such as glaucoma , cataracts and microphthalmos .
Definition of disease
A cataract (another name for the disease is leukoma) is an ophthalmological pathology associated with discoloration and clouding of the cornea. A thorn is formed as a result of foreign bodies (especially frequent) entering the eye, trauma, or inflammation of the cornea. The main cause of clouding is tissue scarring. First, the cornea acquires a porcelain tint, then turns yellow, becomes cloudy, and light transmission is impaired.
The thorn does not always affect the quality of vision - the patient may see objects the same as before, distorted, or not see anything at all.
Depending on the location of the leukoma, it either affects visual function or not. If the leukoma grows significantly, the person may no longer see in the affected eye at all.
Congenital cataracts are much less common than acquired ones.
Types of cataracts – congenital and acquired. The second type of leukoma is more common. The form of formation can also be different and take the form of a spot, a cloud, a total lesion, and so on.
Eye with leukoma (cataract)
Diet for eyesores
Diet for eyes, nutrition to improve vision
- Efficacy: therapeutic effect after 2 months
- Timing: constantly
- Cost of products: 1800-1900 rubles. in Week
Since catarrh is characterized by fatty degeneration, during its treatment it is recommended to reduce the consumption of animal products to a minimum. In addition, the diet practically excludes animal fats and cholesterol-containing dishes and, to maintain vision, recommends enriching the diet with fruit and vegetable salads with carrots, blueberries, and eating more seafood.