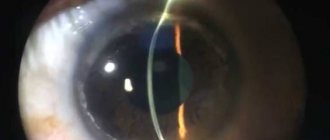
The cornea (or cornea) - which is more often called simply the cornea - in the optical system of the eye performs the functions of mechanical protection and, in addition, plays the role of the first focusing lens on the path of the light beam to the central macula of the retina. This natural lens should normally be transparent, of course. Its diameter practically does not vary and is about 1 cm, the thickness in different areas is from 0.5 to 1.2 mm. At the edges, the corneal lens is diffusely “embedded” in the scleral tissue. The cornea consists of several layers: anterior and posterior epithelial layers, Bowman's and Descemet's membranes, stroma (the main functional substance).
Like any other tissue or organ, the cornea is susceptible to numerous diseases, injuries, and pathological transformations. Infectious-inflammatory and degenerative processes, injuries, drying out, etc. - all of them, taking into account the exceptional place and significance of the corneal outpost of the eye, are to one degree or another dangerous for vision as a whole: any, even slight distortion of shape, decreased transparency or changes in the refractive index (refraction) inevitably affect visual functions and, as a rule, cannot be corrected with glasses or contact optical correction. Therefore, in some cases, the only way to preserve or restore vision is transplantation - a cornea transplant.
Cornea transplant operations, penetrating keratoplasty, have long been firmly established in the arsenal of modern ophthalmology. Since the beginning of the last century, a variety of transplantation algorithms and techniques have been developed, which are successfully used depending on the specific indications and goals of the intervention.
Thus, the scale of replacement varies: the entire cornea, or a certain part of it, or individual layers can be transplanted. According to the objectives of keratoplasty, the following types are distinguished:
- optical, designed to restore shape and/or transparency (for keratoconus, dystrophies, scar changes due to injuries, keratitis, etc.);
- reconstructive (for thinning, ruptures, perforations of the cornea);
- therapeutic (for burns, infectious or trophic ulcerations of the cornea, tumors, abscesses, perforations, etc., if there is no effect from conservative therapy, for example, antibiotic);
- cosmetic (to eliminate pronounced cosmetic defects - cataracts, scars, deformations, etc.).
In practice, keratoplasty can, as a rule, solve several problems, for example, the operation is both optical and cosmetic. This is especially true for total or subtotal corneal transplantation with the replacement of all its layers, i.e. throughout the entire thickness, which is called penetrating keratoplasty.
Video of penetrating keratoplasty surgery
Such intervention is usually performed for several indications: optical, reconstructive, therapeutic, and less often only cosmetic. According to accumulated medical statistics, keratoplasty has the greatest effect and the best prognosis for dystrophic diseases, cicatricial deformities and keratoconus (anatomically abnormal anterior extension of the cornea). Factors that significantly worsen the prospects and should be taken into account as much as possible when preparing for surgery include inflammatory processes of the eyelids, conjunctiva, ocular vessels (respectively, blepharitis, conjunctivitis, uveitis of various etiologies), glaucoma, the presence of adhesions, cords, etc.
The transplanted keratobioimplant must be selected within 24 hours from the moment of the donor’s death, and the material undergoes a series of strictly mandatory studies and is not applicable in the following cases:
- unknown cause of death;
- infectious diseases, including systemic viral and neuroinfections;
- leukemia, lymphoma;
- oncological diseases of the eyes, incl. previously operated;
- infant or old age (over 70 years) of the donor.
Specialist doctors
Professor Anat Kasler
Serves as head of the ophthalmology department at Ichilov Hospital
Professor of Ophthalmology in the Department of Vision Correction at Sourasky Hospital (Ichilov Medical Center)
Specialization
Specialization
- Laser therapy for corneal detachment.
- Correction of insufficient visual fields.
- Diagnosis of ophthalmological and neuro-ophthalmological diseases.
- Elimination of high intraocular pressure.
- Elimination of glaucoma.
Work experience:
more than 35 years.
- Surgical treatment of uveitis.
- Surgical neuro-ophthalmology.
- Ophthalmic neurology.
- Treatment of retinal detachment.
Knowledge of languages:
English, Italian, Hebrew.
Operation technique
In the vast majority of cases, penetrating keratoplasty is performed under general anesthesia. The main reason is that keeping the eye completely still is critical to a successful outcome.
Specific indications, objectives, anamnestic and clinical characteristics determine the choice of one or another option of penetrating keratoplasty; The standard is considered to be transplantation of 2/3 of the central volume of the cornea. We use a variety of microsurgical instruments that have evolved over the course of a hundred years to almost perfection.
It is important to note that the cornea does not have its own blood network, which further facilitates the intervention and improves the prognosis; and yet, today the use of femtosecond lasers of the latest generation is considered more promising and safer (in terms of intra- and postoperative complications) for ultra-precise excision and removal of the affected cornea with the formation of a slice of the desired shape. In all cases where this is possible, laser intervention should be considered as the preferred choice.
The corneal biotransplant is attached with very thin (much thinner than a hair) suture material. The duration of the rehabilitation period can in some cases reach 10-12 months or even more - only then the stitches are removed.
Laser keratoplasty of the cornea
Corneal transplantation (penetrating keratoplasty) is a microsurgical operation during which a damaged area of the patient's cornea is replaced with a donor graft. The transplant can significantly improve vision in diseases affecting the cornea and restore damage caused by eye injuries.
The operation is usually performed under general anesthesia. The cornea is a relatively simple tissue and does not contain blood vessels, so in the vast majority of cases the donor site survives well. At an early stage of engraftment, antimicrobial therapy is prescribed, and glucocorticoids are instilled to prevent a possible rejection reaction.
Corneal pathologies requiring keratoplasty include:
Keratoconus
- Various types of corneal cataracts - burn and dystrophic;
- Congenital and acquired corneal dystrophies;
- Corneal scars after trauma, surgery and inflammation;
- Traumatic corneal defects.
Preparation for surgery begins with a complete examination of the visual system, which allows doctors to identify the disease at the earliest stages, determine the indications for surgery, and also predict its outcome.
During the operation, the surgeon creates a corneal flap and separates the damaged part of the cornea. In its place, a “corneal graft” is implanted, which exactly matches the size of the previously formed flap. Using a special suture material, it is attached to the peripheral part of the patient's cornea. After the operation is completed, a bandage or a special protective contact lens is applied to the patient's eye.
Keratoplasty is performed on an outpatient basis, under anesthesia or under local (parabulbar) anesthesia using modern drugs that do not put a strain on the cardiovascular system and are well tolerated by patients of all ages. After the operation and examination by a doctor, the patient returns home, which certainly contributes to the most comfortable recovery.
The rehabilitation period after keratoplasty lasts up to a year, due to the structural features of the cornea. Suture removal usually occurs 6-12 months after surgery.
Cost of services
| Treatment of corneal diseases with riboflavin (crosslinking) | 27000 |
| Implantation of stromal corneal half-rings (without the cost of consumables) | 40000 |
| An operation performed using Femto Laser increases the cost of the operation by | 35000 |
| Consumables: | |
| 1 half ring | 22000 |
| 2 half rings | 42000 |
| Keratoplasty (including prepayment for consumables per eye 100,000) | 190000 |
| Keratoplasty using a femtosecond laser (including prepayment for consumables per eye 100,000) | 215000 |
All prices
Fill out a request on the website, we will contact you as soon as possible and answer all your questions.
Make an appointment
Postoperative period (rehabilitation)
As an immunosuppressive support for engraftment (i.e., to locally suppress the immune system and reduce the likelihood of transplant rejection), steroid hormonal drugs are prescribed locally, usually in small doses. In some cases, mydriatics are indicated - means of dilating the pupil. In the presence of a chronic viral neuroinfection (primarily herpes), preventive treatment is necessary, for example, acyclovir, to prevent exacerbation. Rigid contact lenses are sometimes required to correct residual astigmatism, but these are prescribed only after suture removal.
Possible complications in the immediate postoperative period include infection, increased intraocular pressure, and mechanical irritation from sutures. To the remote - the spread of the pathological process, which was supposed to be interrupted by keratoplasty, to the keratobioimplant itself; glaucoma; swelling of the retina, etc. And, of course, the ineffectiveness of the operation may be due to failure (rejection) of the implant.
Endothelial keratoplasty
Indications:
- Hereditary corneal dystrophies with damage to the posterior layers
- Secondary endothelial corneal dystrophies
- Endothelial decompensation of corneal graft after keratoplasty
Even before the 21st century, the main method of treating corneal endothelial dysfunction was penetrating keratoplasty
, but with the development of technology, it has become possible to perform selective transplantation
of only the posterior layers of the cornea
, which are involved in the
pathological process
.
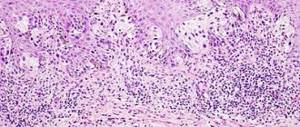
Posterior lamellar keratoplasty involves replacing a damaged layer of endothelial cells with a thin disc of donor cornea.
At the first stage
The operation removes the patient's endothelial layer and Descemet's membrane through a small incision in the cornea.
Further
A transplant is cut out from the prepared donor material, which is a thin disk of corneal tissue - endothelium (a layer of endothelial cells), Descemet's membrane and a small layer of corneal stroma.
After implantation
graft into the anterior chamber of the eye, it is fixed with air or a gas-air mixture. Upon completion of the operation, only a few interrupted sutures are placed on the corneal incision.
The time frame for removing corneal sutures is 3-5 months.
The advantages of performing posterior lamellar keratoplasty are:
- faster visual rehabilitation of the patient
- achieving higher visual acuity
- minimal induced postoperative astigmatism
- reducing the risk of corneal graft rejection
- reduced risk of intra- and postoperative complications compared to penetrating corneal transplantation.
In 2006, Dr. Melles GR proposed the technology of endothelial keratoplasty, during which only the layer of endothelial cells and Descemet's membrane is transplanted - Descemet's membrane transplantation.
This type of surgical treatment has attracted the attention of corneal surgeons, and thanks to the development of technology and the acquisition of experience, Descemet's membrane transplantation has become an effective and most physiological method for treating endothelial dysfunctions.
Considering that the donor graft does not contain the stromal corneal layer, the patient achieves maximum potential visual acuity, faster visual rehabilitation and an even lower percentage of graft rejection.
In our clinic, each patient undergoes a complete diagnosis using the latest modern equipment, after which the tactics of further surgical treatment are individually determined.
Performance Statistics
As mentioned above, it is not possible to talk about some kind of universal probability of success guaranteed for all cases. The prognosis depends on many factors: the patient’s age, the intensity of vascularization (the degree of development of the ocular circulatory system), the presence and nature of concomitant diseases, the very nature of the corneal lesion, and many others.
However, it cannot be denied that ophthalmic surgery is one of the most developed and effective branches of medicine today. Most serious sources cautiously provide data that the predictive probability of successful penetrating keratoplasty exceeds 90% (up to 95%).
Methods of artificial cornea transplantation in Israeli clinics
Synthetic keratoprostheses are perfectly compatible with the patient’s tissues and have all the capabilities of a living cornea, completely restoring vision.
Implantation of acrylic keratoprosthesis - often used in patients with donor tissue rejection.
The combined implantation of an artificial implant and donor tissue is a unique technique that allows you to accurately predict the result and improve biocompatibility.
Implantation of a prosthesis with an epithelial coating - rapid fusion and ideal compatibility.
Collagen implantation is the restoration of the superficial corneal layer with collagen (a product of yeast fungi).
Implantation of a hydrogel keratoprosthesis means the possibility of glucose accumulation.
Cornea
- Donor cornea transplant
- Treatment of keratoconus
- Laser vision correction
- Treatment of astigmatism
Diagnostics
- Electroretinogram (ECG) of the eye
Cost of the operation
Penetrating keratoplasty is carried out on the basis of the main division of the organization - the Moscow Eye Clinic (MGK) - a leading ophthalmological center among commercial clinics specializing in this type of operation.
Our own bank of biotransplants and the vast experience of our doctors allow us to quickly and successfully perform keratoprosthesis even in the most difficult cases.
The price of the operation consists of two components - the cost of keratoplasty itself ( 90,000 rubles) and the biomaterial “corneal transplant” ( 98,000 rubles). Thus, the final figure is 188,000 rubles.