Keratitis is considered one of the most serious forms of corneal infection. Fortunately, it does not occur very often: this diagnosis is made in only 4.2% of cases of the total number of inflammatory diseases of the eye membranes.
However, inflammation of the cornea must be taken seriously. If you suspect you have this disease, you should immediately consult a specialist, and then carefully follow the prescribed treatment. The consequences of trying to cope with the disease on your own can be its transition to a chronic form, the appearance of complications (from the appearance of ulcers, scars, scars up to a cataract and loss of vision.
So, keratitis is an inflammatory disease of the cornea of infectious or traumatic origin, which can lead to partial or complete loss of vision. Let's take a closer look at its symptoms and manifestations, the reasons why it occurs, as well as methods of treatment and prevention.
General structure
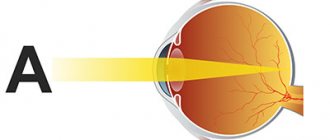
The cornea consists of five layers:
- Integumentary – responsible for protection, moisture and gas exchange;
- Bowman's membrane is a sensitive front plate that becomes cloudy when cells are damaged;
- Stroma – maintains the strength of the organ;
- Descemental part - provides material for the formation of all corneal cells;
- The endothelial layer protects the stroma from ocular moisture.
Early diagnosis of ocular corneal disease helps to promptly identify problems and promptly neutralize them.
Treatment of the cornea of the eye
- Erosion processes
. If the damage is shallow, they can be treated on an outpatient basis - instilling local anesthetics, using healing gels and ointments, drops based on hyaluronic acid or natural tears. Elimination of defects is usually carried out quickly, epithelization occurs without complications. - Entry of foreign bodies
. In this case, the cornea can be restored by removing objects. If they are in the superficial layers, do this with a cotton swab, if in deeper layers, remove them with tools. The patient is also prescribed medications based on natural tears, ointments and drops with antibiotics. - Wounds, scratches on the cornea
. Eye microsurgery is used here. Such operations are performed in specialized ophthalmology departments. In parallel with surgical procedures, antibiotics, systemic treatment with enzymes, and local medications - drops, ointments - are prescribed. - Burns
. Corneal correction is performed by excision of the affected tissue. In parallel with this, antibacterial, healing, enzyme therapy and therapy aimed at relieving inflammation are used. - Retinal disinsertion
. Recovery is possible thanks to laser correction of the cornea, cryopexy, and pneumoretinopexy. If there is a rupture, a vitrectomy is performed - the vitreous body is removed and replaced with a synthetic analogue.
Priority actions should be aimed at getting rid of the damaging factor, then begin restoration measures. Therapy is prescribed to help restore integrity to tissues and stimulate their further regeneration. Preventive measures to prevent the development of infections are also of great importance.
Mechanical injury
Wooden or metal chips, chemicals and sand entering the eye damage the organ and get stuck in the superficial and deep layers of the cornea. Against this background, patients often develop erosion.
Symptoms:
- Severe pain in the eyeball;
- Tearing and sensitivity to light;
- Burning, itching;
- Visible areas of clouding in the cornea.
If you notice any of the manifestations, it is advisable to immediately contact an ophthalmologist. He will diagnose the type of corneal disease and choose the appropriate treatment method.
Causes of corneal keratitis
Reasons that can lead to inflammation of the cornea include:
- damage to the eyes by viruses (for example, of the herpetic group - in more than a third of all cases, adenoviruses. Viral herpetic keratitis of the eye is also called dendritic);
- bacterial flora (often the appearance of keratitis is caused by streptococci and staphylococci, pale spirochete, Haemophilus influenzae and Pseudomonas aeruginosa, etc.);
- mycotic infection by candida and other fungi (most often develops with long-term use of penicillin antibiotics);
- damage by amoebas, more common in contact lens wearers;
- getting particles of dirt, dust and other foreign bodies into the eye;
- development of complications in dry eye syndrome of various etiologies (neurological, hormonal nature, vitamin deficiency, physiological features of the structure of the eye);
- long-term use of certain medications: for example, ointments with corticosteroids, etc.;
- allergies, the manifestations of which affect the organ of vision;
- traumatic effects of bright light: direct sunlight, welding, etc.;
- improper use of contact lenses.
It happens that even a specialist cannot determine the cause of the disease.
In addition, there are factors that may contribute to the development of the disease. This:
- decreased immunity, fatigue;
- endocrinological pathologies;
- autoimmune diseases;
- vitamin deficiency (especially B vitamins, vitamins A and C).
- uncontrolled use of certain eye drops, for example, hormonal ones.
How does dystrophy manifest?
Dystrophy can be congenital or acquired. The primary form of corneal disease affects both visual organs. Secondary affects one eye and develops against the background of such events as:
- Past injuries;
- Ophthalmic diseases;
- Operations on the organs of vision.
Diseases of the ocular cornea associated with dystrophy are detected only in the clinic with a thorough instrumental examination.
During this period, patients complain of:
- Decreased visual acuity;
- Severe dryness.
A case of corneal disease that appears in a child by the age of 40 provokes the development of blepharospasms, myopia and photophobia.
Diagnosis and treatment of corneal diseases
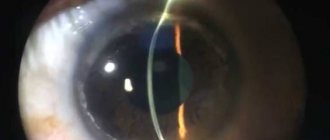
To diagnose corneal diseases, ophthalmologists at Dr. Belikova's Eye Clinic perform biomicroscopy - a non-contact examination of eye structures using a slit lamp.
If changes in the shape or refractive power of the cornea are detected, the Patient is prescribed vision correction using glasses, contact lenses, or surgical treatment.
In some complex cases, we use keratoplasty to treat corneal pathologies.
If the cause of the corneal disease is an infection, the attending physician prescribes antibacterial, antifungal or antiviral drugs to the Patient.
Forecast
The prognosis for treatment of the disease depends on the severity of its course, the patient’s health status, as well as the cause that caused it.
Small areas of clouding located on the periphery of the eye and affecting vision require only supportive care and medical supervision.
Progressive cataracts that were caused by syphilis, tuberculosis or other diseases respond well to conservative treatment after eliminating the root cause of the problem.
The prognosis of surgical treatment (tissue transplantation) for significant opacities is usually also favorable.
The cornea does not have its own vessels, so the antibodies that are formed in the body to reject foreign tissues do not pass through its cells, due to which the donor cornea takes root well.
The most difficult to treat are cataracts that were caused by mechanical trauma to the eye or a burn. In this case, everything depends on the scale of tissue damage - if there is massive damage, it is only possible to eliminate the symptoms of the pathology (photophobia, tearing), but it will not be possible to completely restore vision.
Structural features
The cornea consists of several tissues:
- anterior epithelial;
- anterior limiting membrane;
- stroma;
- Dua layer;
- posterior limiting membrane;
- endothelial tissue.
The epithelial layer has a high regeneration rate and promotes rapid tissue restoration after various injuries. The intrinsic substance or stroma occupies a larger volume.
The protective role is played by the posterior border plate, which is highly durable. It prevents the ingrowth of small capillaries, infection and the negative effects of purulent exudate when ulcerative defects and other disorders appear.
Treatment of inflammatory diseases of the cornea and sclera
Keratitis of various origins
Adenoviral keratitis and keratoconjunctivitis
- The use of drugs that are used to treat patients with adenoviral conjunctivitis is indicated.
- Subconjunctival injections of anti-measles gammaglobulin and deoxyribonuclease are useful. It is advisable to administer the first drug 0.3 ml 1 time for 2-3 days, the second - 0.5 ml for 2 weeks.
Bacterial keratitis
Take smears from the affected surface of the cornea and conjunctiva to determine the causative agent of the disease and its sensitivity to antibiotics.
- Dilate the pupil of the affected eye by installing a few drops of one or another mydriatic into it (in an age-appropriate dosage).
- Start frequent instillation (up to 6-8 times a day) of drops containing antibiotics and/or antiseptics into the eye. When choosing drugs, you need to take into account the results of bacteriological studies.
- In resistant cases, subconjunctival injections (1-2 times a day) of broad or targeted antibiotics - gentamicin (10-20 mg per day) or netromycin - are also indicated.
- Dry heat (sollux) on the eye area.
Fungal keratitis
Determine the causative agent of the disease (smear and scraping from the conjunctiva).
- For candidiasis, the most effective are nystatin (1% solution in drops and 1.0-2.5% solutions for subconjunctival injections) and levorin (1.0-2.5% solutions in drops and 2.5% eye ointment).
- For other fungal infections, you need to use amphotericin B (0.25-0.5% drops in a 5% glucose solution) and/or a 2.5% natamycin suspension (synonym: pimafucin).
Acanthamoeba keratitis
- Hourly installations of 0.5% dioxidine solution into the affected eye.
Herpetic keratitis
Superficial forms (dendritic keratitis):
- The use of drugs with selective antiherpetic activity is frequent (up to 8 times a day) installation of a 0.1% solution of idoxyuridine (IDU, Oftan IDU, herplex, stoksil, kerecid) into the eye for 10-14 days (further it has a pronounced toxic effect). effect on the corneal epithelium) or, even more effective, placing 3% acyclovir ointment (Zovirax, Virolex) behind the eyelids 3-5 times a day.
- For IDU-resistant forms of keratitis, frequent installations into the eye of leukocyte alpha-interferon (200 IU/ml) or related drugs - interlock (10,000 IU in 0.1 ml of phosphate buffer), reaferon (5000-100,000 IU in 1 ml) are indicated distilled water) or berophor. The installation regimen for the latter drug is special - 2 drops once a day. The interval between drops is 5-10 minutes. The course of therapy is 6 days.
Human beta interferon (fibroblastic) is also offered for use. The drug called “Fron” needs to be instilled 2 drops 6 times a day for 7 days. Poludan, a biosynthetic polyribonucleotide complex that ensures the production of α, β and γ-interferons in the tissues of the eye and blood, has proven itself well as an interferon inducer. It can be used in the form of eye drops (100 IU in 5.0 ml of distilled water) or subconjunctival injections (50-100 IU of the drug in 1 ml of solvent).
- The use of immunomodulators, in particular lycopid, is indicated.
- A course of intramuscular injections of vitamins B1 and B2; ingestion of ascorbic acid and vitamin A.
Deep forms (discoid keratitis):
- Place 3% Zovirax ointment (acyclovir, virolex) behind the eyelids 4-5 times a day.
- Subconjunctival injections of leukocyte alpha-interferon with an activity of 200 IU/ml (0.3-0.5 ml No. 15-20) and/or its analogues, for example reaferon (PO 60,000 IU in 0.5 ml of solvent). Subconjunctival injections of interferon inducers, in particular Poludan (100 U in 1.0 ml of solution), are also useful.
- Use of immunomodulators. Ingestion of B vitamins and their intramuscular injections.
Tuberculous keratitis
- General course therapy for 10-12 months with the simultaneous use of 2-3 anti-tuberculosis drugs of the first and second line (main and reserve drugs). The first include: isoniazid (daily dose 5-15 mg/kg), rifampicin (8-10 mg/kg) and streptomycin (15-20 mg/kg), the second - pyrazinamide (15-20 mg/kg), kanamycin (1 g per day for adults, children - up to 20 mg/kg), PAS.
- Local therapy: instillation of a 5% solution of saluzide into the eye or its introduction under the conjunctiva, as well as by electrophoresis. Some other drugs can also be used - PAS (5-10% solution or ointment of the same concentration), tubazid (3% solution), streptomycin (diluted 50,000 units/ml).
- Constant monitoring of drug tolerance.
- Desensitizing therapy.
Parenchymal syphilitic keratitis
- General specific therapy.
- Local therapy: anti-inflammatory using corticosteroid drugs in the form of eye drops and subconjunctival injections, as well as mydriatics. To resolve corneal opacity, it is advisable to use a solution of dionin in increasing concentrations and 1% yellow mercury ointment.
Next »
Congenital corneal abnormalities
- Megalocornea
Megalocornea is a congenital defect in which the diameter of the outer eye membrane is more than 11 mm (the norm is about 9 mm). The disease is detected in infants in the first days of life after examination by an ophthalmologist. If the baby maintains normal vision, then treatment is not carried out. It is required only in cases of refractive error (myopia, farsightedness, astigmatism). To correct vision, wearing glasses or contact lenses is prescribed.
- Microcornea
Microcornea also refers to congenital diseases. This diagnosis is made if the cornea of the newborn's eye is less than 9 mm in diameter. Often with this pathology, the child subsequently develops myopia, and therefore vision deteriorates. If the baby does not have other congenital anomalies of the visual organ, then the prognosis is favorable. A child’s vision can usually be maintained normal with timely correction with glasses.