- Operation options
- Indications for surgery
- How to prepare
- How is the operation performed?
- Recovery period
- Complications
- Transplant price
- Clinics
Keratoplasty is a broad term that includes all ophthalmic surgical procedures performed on the cornea.
A healthy cornea should be clean, smooth and transparent for good vision. If there are scars, tumors or damaged areas, the light may not focus properly. As a result, your vision is blurred or you see glare.
In many cases, the cornea cannot be healed or restored naturally. In this case, vision can be restored by keratoplasty - an operation where the diseased cornea is replaced with a healthy one from a human donor or an artificial implant. https://ultrastom.shop/magazin/folder/sovmestimo-s-neobiotech
Indications for corneal transplantation
Replacement of the cornea of the eye is necessary if conservative and other treatment methods do not have the desired effect. Only a specialist can determine when surgery should be performed, based on many facts, since the process of eye restoration is a fairly lengthy procedure. In most situations, this procedure is the only way to deal with defects. Most often, tissue transplantation is needed:
- with congenital and acquired thinning of the cornea;
- with bullous keratopathy;
- with the formation of scars after surgery and burns;
- for adhesions that appear after an infection or viral disease;
- after a chemical burn with complications;
- if you have irregularly shaped eyes.
Contraindications
Like most other operations, keratoplasty has contraindications that prohibit its implementation. Problems with the cardiovascular system and lung disorders are considered relative prohibitions, in which the doctor weighs the possible risks and the expected effect. The reason for delaying the date of transplantation may be the presence of local foci of inflammation.
In this case, the disease is treated and only then can one think about keratoplasty.
A categorical prohibition for corneal transplantation is:
- inflammatory processes in the eyes;
- blockage of tear ducts;
- severe increase in pressure inside the eyes;
- hemophilia, the development of which began against the background of diabetes mellitus;
- the presence of a blood clot.
It is extremely rare that corneal transplantation is performed during pregnancy and breastfeeding. As a rule, if such an operation is necessary, it is postponed. Since for a certain period after surgery you should take medications, the effect of which on children has not been studied.
Types of keratoplasty
Complete transplant
It may be required if both the outer and inner layers of the cornea are damaged. This is called penetrating keratoplasty (PK) or full thickness grafting. The diseased or damaged cornea is removed. A clear donor cornea is then sutured in its place. Despite the greatest trauma of all options, this is the simplest version of keratoplasty.
PC has a longer recovery period than other types of corneal transplants. Restoring full vision after PC may take up to one year or longer.
There is a higher risk of graft failure with PC than with other types of corneal transplants.
Partial corneal graft transplantation
Sometimes only the anterior and middle layers are damaged. In this case, only these layers are deleted. The endothelial thin posterior layer remains in place. This graft is called deep anterior lamellar keratoplasty (DALK) or partial thickness corneal transplant. DALK is usually prescribed to treat keratoconus, or corneal bulge.
Healing time after DALK is shorter than after full corneal transplantation. There is also less risk of rejection of the new cornea. This operation is more complex, and is performed in only a limited number of clinics in the CIS.
All modern cornea transplant operations are performed in Belgium, including DALK. In some clinics, the intervention is performed using a femtosecond laser, which makes it safer.
Deep anterior lamellar keratoplasty (DALK) involves excision of the cornea down to the level of Descemet's membrane. A blind corneal disc is formed on the recipient's eye. A cut-out end-to-end donor disc without endothelium is placed on the recipient's Descemet's membrane, freed from the surface layers of the stroma, and fixed with sutures. The main advantage of the method is considered to be the minimal risk of graft rejection.
After DALK, the graft becomes transparent already 3-5 days after surgery. The operation provides better functional results: after engraftment of the graft, visual acuity of 0.7-0.9 is achieved, and some patients receive one hundred percent vision.
Corneal transplant operations are performed at the Saint-Jean Clinic by a team of doctors led by Dr. Jérôme Vryghem. This specialist performs more than 2 thousand ophthalmological interventions every year. Since 2007, he has been one of the first in Belgium to use the femtosecond laser. This technology makes it possible to make more precise cuts in the corneal tissue in any way. The femtosecond laser makes it possible to take an individual approach to the choice of surgical procedure.
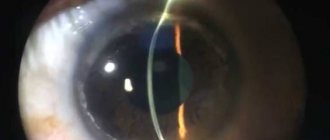
Endothelial keratoplasty
In some eye diseases, the innermost layer of the cornea, called the “endothelium,” is damaged. This causes swelling of the cornea, which affects your vision. Endothelial keratoplasty is a surgery to replace this layer of the cornea with healthy donor tissue.
The damaged layer of the cornea is removed through a small incision. The new fabric is then placed in place. Only a few stitches, if any, are required to close the incision. Most of the cornea remains intact. This reduces the risk of new corneal cells being rejected after surgery.
There are two types of endothelial keratoplasty.
- DSEK (or DSAEK) - endoscopic Descemet's membrane keratoplasty (automated). In DSEK/DSAEK surgery, the donor tissue is easier to graft and position because it is thicker than the donor tissue in DMEK surgery. Therefore, this operation is more common.
- DMEK - Descemet's membrane endothelial. In DMEK surgery, the donor tissue is thin and may be more difficult to graft. But recovery is faster and the long-term results of the operation are better because the graft tissue is thinner. But this operation is performed abroad only in ophthalmological centers with the highest level of technical equipment and training of surgeons. In Belgium, this method has been introduced since 2012.
Artificial corneal implant
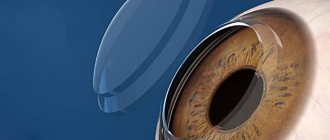
In this type of surgery, an artificial flexible keratoprosthesis is implanted into the corneal pocket using a minimally invasive procedure.
There is a large discrepancy between the availability of corneal tissue for transplantation and the number of patients requiring corneal transplantation. Artificial implants can solve this problem. But only in the last few years have they been able to provide levels of vision restoration comparable to donor corneas.
Nowadays, in patients at high risk of rejection with a human donor, a keratoprosthesis can provide good visual results with a good risk-benefit ratio.
Bionic corneal implant
This is an innovative method that is just entering the practice of leading ophthalmological clinics in Europe. A corneal prosthesis is created by 3D printing from decellularized corneal stroma and stem cells.
This cornea is completely biocompatible, and 3D cell printing technology allows the microenvironment of the cornea to be reproduced. As a result, the transparency of the implant is similar to that of the human cornea.
Preparation for keratoplasty
When the decision is made to transplant the cornea, the patient undergoes a full examination. If any health problems are identified, he is referred for consultation to specialized specialists who prescribe treatment. Thus, the development of problems with the functioning of vital organs is excluded.
If there are eye diseases that may have a negative impact on the transplant, they also need to be cured. Such diseases include:
- eyelid pathologies;
- inflammatory process of the conjunctiva and sclera;
- inflammation of the blood vessels of the eye;
- the presence of uncompensated glaucoma.
It is necessary to undergo a full course of treatment for eye diseases, since existing inflammation can spread to the transplanted cornea. Immediately before surgery, a culture is taken from the conjunctival membrane to identify the pathogen and sensitivity to antibacterial agents. A broad-spectrum antibiotic is initially used, and therapy is subsequently adjusted based on culture results.
How does the transplant take place?
Cornea transplantation can only be done in a hospital setting. One day is allocated for the operation without subsequent hospitalization. The specialist carries out preoperative diagnostics, after which the exact size of the membrane that needs to be removed is known. Also, donor material is additionally prepared, which fully corresponds to the size of the membrane being removed. The operation is performed under a microscope.
The eyelid must be fixed using an eyelid expander. Using a laser, the specialist removes a portion of the corneal tissue and replaces it with a donor cornea. The transplanted material is fixed with sutures along the entire contour.
If the anterior part of the cornea is removed, the operation is considered easier. With a complete corneal replacement, the risk of tissue rejection increases. The stitches are removed by a specialist no earlier than after 4 months. The healing process can last more than a year depending on the depth of the operation.
Eye after surgery
For several days after keratoplasty, the patient is under strict medical supervision. During this time, it is important to take hormone therapy, antibiotics and agents to accelerate wound healing. All this time, the operated eye is kept under sterile bandages.
After discharge, the patient continues recovery on his own, following the recommendations of specialists regarding instillation of the conjunctival cavity. For this use:
- hormonal solution to reduce the likelihood of rejection of the transplanted material;
- antibiotics;
- drugs that replace natural tears;
- Dexpanthenol gel.
It usually takes at least a year to restore normal functioning of the cornea. But even in the absence of complications, it is not possible to restore vision immediately. For an indefinite period of time, patients may see distorted images and suffer from photophobia. On average, it takes several months to restore vision; in some cases, this period may be delayed.
All this time, the specialist helps you choose temporary optics that help you perceive the world around you normally. There are also some recommendations that must be followed throughout the entire period:
- Strong physical activity should be avoided;
- limit exposure to bright light by protecting your eyes with sunglasses;
- try not to get colds;
- avoid visiting places with high temperatures;
- do not touch the eyes to rub, avoid pressure;
- sleep on the opposite side of the transplanted cornea;
- prevent dust and other contaminants from getting into your eyes;
- use all prescribed medications.
Bionic eye
As already mentioned, retinal transplantation at this stage of medical development is impossible due to the special functions of this membrane of the eye and its close connection with the brain. However, research in this area is being actively carried out, since the success of such an operation will restore vision to many patients with severe diseases and even those who are blind from birth.
Retinal detachment
An event that occurred in 2015 in England can be considered a breakthrough in this area of ophthalmology. Experts implanted a bionic eye into 80-year-old patient Roy Flynn, who lived in Audenshaw, Greater Manchester. The man had been suffering for many years from age-related macular degeneration (retinal damage), which is one of the most common causes of blindness in people over 55 years of age.
A unique experimental procedure was performed on June 18, 2015 by specialists from the Royal Eye Hospital in Manchester, which is one of the leading ophthalmological centers in the world.
The Argus II bionic prosthesis was developed by the American company Second Sight. It consists of 2 main parts. The first is a mesh implant that is implanted into the patient. The second is an external system, which contains a mini-camera with a processor, built into seemingly ordinary glasses. The camera records what is happening around in real time, then the received information is processed by the processor and transmitted to the implant. The latter stimulates those healthy retinal cells that remain in the patient. As a result, information is sent to the optic nerve and the brain begins to distinguish objects, their shapes and light again.
Roy Flynn is a patient who managed to regain his sight after a bionic eye transplant
Interesting! The bionic eye was implanted into another 130 patients, but Roy's case was particularly successful. Already after 1 week after the experimental procedure, the man was able not only to see everything around again, but even to read text on the monitor screen, even with his eyes closed.
The cost of the Argus II bionic prosthesis is 150 thousand euros. But researchers intend to continue to implant such implants free of charge to patients, as in the case of Roy Flynn, since such a result can be called an event that gives hope to millions of blind people to see the world around them and loved ones again.
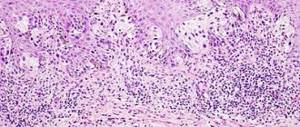
Possible complications
Patients are warned before the transplant that various complications may occur after surgery. Negative manifestations can also occur during keratoplasty.
The most dangerous complication is the body's rejection of the donor cornea. In this case, there is a need for additional surgery. That is, the first transplant is considered useless, and any delay in re-operation can cause a severe deterioration in the quality of vision.
It should be understood that the body can reject the transplanted material regardless of the recovery period. Symptoms of complications that should be alarming are:
- pain manifestations;
- itching;
- sudden onset of photophobia;
- discomfort;
- opening of bleeding;
- sudden change in intraocular pressure;
- swelling;
- astigmatism;
- the appearance of inflammation.
Risks of Corneal Transplant
Keratoplasty, like all surgical procedures, involves certain risks and complications for the patient. Some of them:
- Reazo del nuevo tejido.
- Eye infections.
- Cataract.
- Postoperative astigmatism.
- bleeding.
- Glaucoma.
- Loss of vision.
- Inflammation of the cornea.
Which doctor performs the operation
Keratoplasty is performed by a surgeon. General or local anesthesia is used for the operation. It is best to use general anesthesia, which will help immobilize the patient and prevent the risks of possible corneal injuries.
Immediately before surgery, the cornea is examined using the biomicroscopic method. By viewing the cornea through a slit lamp, the nature, size and depth of the disease are determined. The layers of the cornea are also studied. Additionally, special research methods are used:
- corneal thickness is measured using pachymetry;
- videokeratoscopy is performed;
- a corneal scraping is taken for microbiological examination;
- Corneal biopsy material is taken.
Keratoplasty price
The price of a corneal transplant surgery may vary depending on the type of keratoplasty, the level of the center where the operation is performed, the equipment and the complexity of the procedure. Since the operation is a high-tech medical care, there is an option to receive a quota for free implantation. This card is issued by the regional Ministry of Health.
There is also the option of a paid donor cornea transplant. In this case, you will have to pay for the operation, the average cost of which is at least 100 thousand rubles. Additionally, you should pay for a donor organ with approximately the same cost.
How is an iris transplant surgery performed? Story from Cheboksary
During its existence, the branch of Eye Microsurgery named after Svyatoslav Fedorov in Cheboksary has repeatedly confirmed its status as one of the progressive medical institutions not only in Russia, but also in the world. The ophthalmological surgeons of this center have performed many unique operations, one of which is artificial iris transplantation.
Nadezhda Pozdeeva, professor:
In fact, patients do not get this kind of surgery very often, and in our clinic we perform about 30-40 operations per year, but these operations are very rare, they are unique, and are performed in single clinics not only in Russia, but all over the world.
There are 2 options when a person may find himself without an iris: the first is a congenital pathology, the second is a consequence of a serious injury. Many people read that the iris only determines the color of a person's eyes, however, it is a very important part of the eye.
Nadezhda Pozdeeva, professor:
This is the same as the aperture in a camera: in order to have a clear image, we must adjust the size of the aperture, in the same way the iris functions as an aperture.
When a person loses their iris, it simply needs to be restored, first of all, in order to clearly see the world around them, as well as to eliminate an aesthetic defect.
Nadezhda Pozdeeva, professor:
The artificial iris, which we use to restore the function of a lost iris, can only be used for post-traumatic so-called aniridia, aniridia is the absence of the iris, we use an artificial iris prosthesis, which has a very small thickness - about 200 microns. Artificial irises can be of very different colors and completely different patterns.
As a rule, due to injury, a person loses the iris along with the lens, so during the operation a combined replacement of both the iris and the lens of the eye is performed.
Nadezhda Pozdeeva, professor
: A person operating an artificial iris must be able to simultaneously operate on glaucoma, operate on the retina, operate on the vitreous body, and perform a cornea transplant at the same time, that is, he must be a generalist who can get out of the most difficult situation.
Russian-made artificial irises are made of flexible polymer; they are absolutely inert and safe for the eye and have no analogues in the world. Already today, the largest clinics in Europe, Canada and America have begun to use them for transplantation.