- Grayish rim around the edges of the cornea
- Flat nodules under the skin of the eyelids
- Dense nodules over tendons
- White rim around the edges of the cornea
Hypercholesterolemia is not an independent nosological entity, but a condition of the body in which the level of cholesterol in the bloodstream increases. Typically, the cause of the progression of such a pathological process is various chronic ailments in the human body. For example, diabetes.
- Etiology
- Varieties
- Symptoms
- Diagnostics
- Treatment
- Prevention
With a slight increase in cholesterol levels, hypercholesterolemia does not pose a threat to human health. If the level rises to critical levels, then this is already very dangerous, since there is a high risk of developing atherosclerosis.
Pure hypercholesterolemia according to ICD 10 has code E78.0. It is classified as a group of dysfunctions of the endocrine system and metabolism. Most often, this pathological condition is observed in middle-aged and older people. But such frameworks are not always clear-cut. Hypercholesterolemia can occur in any person whose diet contains large quantities of animal fats.
Causes of the disease
The main reasons for the progression of hypercholesterolemia are ailments already existing in the human body, such as:
- nephrotic syndrome;
- diabetes. This disease in most situations is the main cause of increased cholesterol concentrations in the bloodstream;
- hypothyroidism;
- liver pathologies, mainly of a chronic nature.
Risk factors for progression of hypercholesterolemia:
- hereditary predisposition. In this case, the sick person develops familial or hereditary hypercholesterolemia;
- frequent stressful situations;
- high blood pressure;
- large body weight, often caused by an unbalanced diet rather than a metabolic disorder;
- physical inactivity;
- regular consumption of alcoholic beverages in large quantities;
- poor nutrition and unhealthy food habits. For example, a person regularly eats eggs fried in lard. All this significantly contributes to an increase in cholesterol levels in the bloodstream.
Varieties
Depending on the etiological factors, clinicians divide hypercholesterolemia into:
- primary. It is also called familial hypercholesterolemia. The main reason for its development is a hereditary factor. Homozygous familial hypercholesterolemia is diagnosed if the abnormal genes are present in both parents at the same time. Heterozygous familial hypercholesterolemia occurs in 90% of patients. This form of primary hypercholesterolemia develops when only one parent has the abnormal gene;
- secondary hypercholesterolemia. It progresses only in the presence of factors that are catalysts for the disease. Usually develops against the background of chronic pathologies or metabolic disorders;
- nutritional. The reason for its progression is a person’s unhealthy lifestyle and harmful food addictions.
Familial hypercholesterolemia
Treatment
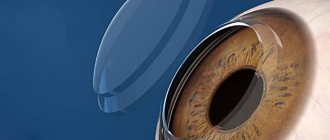
For mild and moderate severity of pellucid marginal degeneration, its correction is prescribed by wearing hard contact lenses - primarily scleral ones, which can be selected in our contact correction department.
In our clinic, we also perform implantation of intrastromal corneal segments (IRS), which also provide high vision and are comfortable for the patient.
In advanced stages of the disease, a layer-by-layer or penetrating keratoplasty operation with a large diameter and downward displacement can be performed. Sometimes semilunar lamellar keratoplasty is performed.
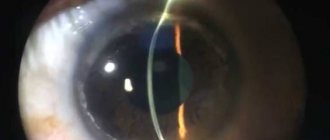
This is what the eye looks like after installation of intrastromal corneal segments (IRS)
Symptoms of the disease
Hypercholesterolemia is not a disease, but a specific laboratory indicator. It is possible to detect an increase in cholesterol levels in the bloodstream only through certain laboratory tests, a lipid profile in particular. Usually, in the case of a slight increase in cholesterol, a person does not experience any external symptoms. They begin to appear only when the pathological condition becomes more advanced. It is worth noting that the symptoms of hypercholesterolemia are quite specific, so it will not be difficult for a doctor to make an accurate diagnosis.
Main symptoms of the pathology:
- xanthomas. This symptom is characterized by the appearance of dense nodules on the human skin, which contain cholesterol inside. Usually localized above the human tendons, for example, on the hand;
- xanthelasma. In this case, there is a deposition of excess cholesterol under the skin of the eyelids. Visually they look like small flat nodules. They may have a yellow color, but in most cases they are difficult to distinguish from previous areas of the skin;
- lipoid arc of the cornea. A characteristic symptom of high cholesterol. Upon visual examination, the doctor can see that a pathological rim has formed along the edges of the cornea, having a white or grayish tint. This is excess cholesterol. This symptom usually occurs in patients over 50 years of age. But if a lipoid arc on the cornea appeared before this age, then this indicates the presence of a hereditary form of pathology in a person.
CORNEA – CONGENITAL AND DYSTROPHIC CHANGES IN THE CORNEA
Ichilov Hospital / OPHTHALMOLOGY / Cornea – Congenital and dystrophic changes in the cornea
Cornea,
cornea (lat. cornea) is the anterior most convex transparent part of the eyeball, one of the light-refracting media of the eye.
Changes in the cornea can be congenital or acquired.
Congenital developmental anomalies include abnormalities in the size and shape of the cornea.
Microcornea
Microcornea or small cornea is an anomaly of the cornea characterized by a decrease in its size. Usually this anomaly is combined with underdevelopment of the entire eye.
If vision function can be restored, surgical treatment is performed. If the eye is completely underdeveloped, treatment is impossible.
Macrocornea
Macrocornea or megalocornea is a congenital anomaly in which the size of the cornea is increased. A giant cornea can reach sizes of more than 1.5 cm. In this case, the size of the entire eye is also increased. Sometimes a large cornea is a sign of congenital glaucoma.
Treatment is surgical.
Keratoconus, keratoglobus
A congenital change in the shape of the cornea, in which the cornea has the shape of a cone or a convex hemisphere. Typically, these changes are associated with a disruption in the structure of the proteins that make up the corneal tissue and appear by the age of 14-18. The wearing of hard contact lenses is prescribed; if there is no effect, a corneal transplant is performed.
Dystrophic keratitis is primary, which occurs as a result of metabolic disorders. Such dystrophies are often hereditary. They are usually bilateral. Primary keratitis affects both individual layers and the entire cornea. The course of primary dystrophic keratitis is slowly progressive. Ultimately, one or another degree of visual impairment occurs.
Drug treatment usually does not produce results. Surgical treatment is carried out - layer-by-layer or through corneal transplantation.
Secondary keratitis develops as an outcome of keratitis arising for various reasons:
due to infection,
injuries.
Senile arc
A senile arc is a circular opacification of the cornea along its periphery. It develops in old age and occurs as a result of metabolic disorders, mainly fat metabolism and cholesterol metabolism. The senile arch usually does not affect the state of vision, so treatment is not prescribed, but observation by an ophthalmologist is recommended.
Ribbon-shaped corneal opacities
Ribbon-like opacification of the cornea is a consequence of a disruption of the structure of the connective tissue and the deposition of calcium salts in the cornea along its center, often in the horizontal direction. Usually this condition occurs in blind eyes, after suffering an inflammatory disease of the entire eyeball (panophthalmitis) with death of the eye.
Kaiser-Fleischner ring
A Kayser-Fleischner ring is a ring-shaped deposit of a brown-green pigment dye around the periphery of the cornea. It occurs when there is a violation of copper metabolism, which occurs during hepatolenticular degeneration, accompanied by dysfunction of the liver and nervous system.
The ring itself does not impair visual acuity and does not require treatment.
Bullous keratitis
This disease occurs in old age in blind eyes with glaucoma. It is accompanied by the formation of blisters on the cornea, which easily open, heal and appear again.
The underlying disease must be treated.
- Ophthalmology in Israel
- Eye – Structure of the eye
- Eye – Functions of the eye
- Eye diseases
- Causes of poor vision
- Eyeball – Exophthalmos
- Eyeball – Injuries
- Eye burns
- Sclera – Diseases of the sclera
- Eye – Refraction of the eye
- Cornea
- Cornea – Congenital and dystrophic changes in the cornea
- Cornea – Inflammatory diseases of the cornea of exogenous origin
- Cornea – Inflammatory diseases of the cornea of endogenous origin
- Cornea – Herpetic keratitis
- Eye - choroid
- Choroid of the eye - Developmental anomalies
- Uveitis - Uveitis
- Uveitis of the eye – Anterior uveitis
- Uveitis of the eye – Posterior uveitis
- Uvea of the eye – Peripheral uveitis
- Eye - Retina
- Retina – Retinal diseases
- Retina – Retinal detachment
- Retinal detachment - Treatment
- Myopia (Myopia)
- Farsightedness (Hypermetropia)
- Presbyopia (Age-related farsightedness)
- Astigmatism
- Spasm of accommodation
- Amblyopia (Lazy Eye)
- Asthenopia
- Hemeralopia
- Retinopathy
- Diabetic retinopathy
- Hypertensive retinopathy
- Atherosclerotic retinopathy
- Binocular vision
- Strabismus
- Strabismus – Paralytic strabismus
- Strabismus – Concomitant strabismus
- Optic Nerve – Developmental Anomalies
- Optic Nerve – Stagnant optic disc
- Optic nerve – Inflammatory diseases
- Optic Nerve – Optic Nerve Atrophy
- Optic nerve – Vascular lesions
- Optic nerve - Toxic lesions
- Optic Nerve – Optic Nerve Tumors
- Optic nerve – Tumors of the optic chiasm
- Eye - Lens
- Lens – Anomalies of lens development
- Lens – Lens luxation
- Lens – Cataract
- Cataract – Types of cataracts
- Cataract – Acquired cataract
- Cataract – Cataract Treatment
- Eye - Vitreous
- Vitreous – Vitreous diseases
- Eye – Conjunctiva
- Conjunctiva – Inflammatory diseases
- Conjunctivitis – Acute banal
- Conjunctivitis – Pneumococcal
- Conjunctivitis – Acute epidemic Koch-Wicks
- Conjunctivitis – Gonococcal
- Conjunctivitis – Diphtheria
- Conjunctivitis – Angular
- Conjunctivitis - Viral conjunctivitis
- Conjunctivitis – Chlamydial conjunctivitis
- Conjunctivitis – Autoimmune and allergic conjunctivitis
- Conjunctivitis – Chronic conjunctivitis
- Conjunctiva – Dystrophic diseases
- Lacrimal organs
- Lacrimal organs – Developmental anomalies
- Lacrimal glands – Inflammatory diseases
- Lacrimal drainage apparatus – Inflammatory diseases
- Eye - Eyelids
- Eyelids – Anomalies of the eyelids
- Eyelids – Blepharitis
- Eyelids – Stye
- Eyelids – Abscess, Cellulitis
- Eyelids – Chalazion
- Eyelids – Viral lesions
- Eyelids – Congenital benign neoplasms of the eyelids
- Eyelids – Acquired benign neoplasms of the eyelids
- Eyelids – Malignant neoplasms of the eyelids
- Glaucoma
- Glaucoma – Types of Glaucoma
- Glaucoma – Classification of glaucoma
- Glaucoma – Diagnosis of glaucoma
- Glaucoma – Glaucoma Treatment Methods
- Glaucoma – Drug treatment
- Glaucoma – Laser treatment method
- Glaucoma – Surgical treatment method
- Glaucoma - Recommendations
- Glaucoma - Prevention
- Keratoconus
- Sympathetic ophthalmia
- Light ophthalmia
- Endophthalmitis
- Panophthalmitis
- Colorblindness
- Nystagmus
- Computer vision syndrome
- Vision correction – Glasses
- Glasses – A little about glasses
- Vision correction – Contact lenses
- Contact lenses – A little about contact lenses
- Vision correction – Laser correction
- Laser vision correction – Laser operating principle
- Laser vision correction – LASIK
- Laser vision correction – Epi-Lasik
- PRK – Photorefractive keratectomy (PRK)
- Laser vision correction – Choice of surgery
- Conductive keratoplasty
- Department of Ophthalmology MC Ichilov (Souraski)
- Professor Anat Levinshtein – Ophthalmologist
- Professor Anat Kesler – Ophthalmologist
- Professor Yuval Yasur – Ophthalmologist
Diagnostics
An increase in blood cholesterol levels can only be detected through laboratory research methods. Most often, a person does not even suspect that this substance accumulates in large quantities in his body. Usually, an increase in its concentration is detected by chance, for example, during a preventive examination.
The standard diagnostic plan for this pathological condition includes:
- collecting anamnesis of the disease and patient complaints. Sometimes the patient complains of the appearance of pathological formations on the skin - xanthoma and xanthelasma;
- analysis of the patient's life;
- physical examination;
- blood and urine tests;
- blood biochemistry;
- lipid profile;
- immunological blood test;
- genetic analysis.
Features of the development of hypercholesterolemia
Discovery of a new anatomical structure in the structure of the human cornea: the Dua layer.
In Ophthalmology, scientists from the University of Nottingham, UK, published the results of a study leading to the discovery of a new layer of the human cornea. The work was led by Harminder Dua, MD, PhD, after whom the new anatomical structure was named. Until recently, it was believed that the cornea consists of 5 layers: epithelium, Bowman's membrane, corneal stroma, Descemet's membrane and endothelial layer.
The purpose of this study was to discover and characterize a new layer of the human cornea located in front of Descemet's membrane. The study included 31 sclerocorneal transplants, including 6 controls (average donor age 77.7 years).
During the study, air was injected into the corneal stroma in the same way as during deep anterior lamellar keratoplasty - using the “big bubble” (BB) method. The experiment was carried out as follows: (1) conducting an IV, leading to detachment of Descemet's membrane; (2) removal of Descemet's membrane; (3) gradual introduction of an air bubble until the maximum pressure is created, leading to rupture. Then histology of the tissue obtained during the experiment was carried out.
As a result of detailed histological studies, a new layer of the human cornea was discovered, called Dua's layer.
During the study, 3 different air injection techniques were used. Type 1 – well-demarcated central hemispherical elevation of layers up to 8.5 mm in diameter (n=14). Type 2 – thin-walled EV, maximum diameter 10.5 mm, bubble formation began from the periphery and spread centrally (n=5). Type 3 – mixed. When performing IV type 1, in contrast to IV type 2, it was possible to separate the DM completely without additional introduction of an air bubble, this indicated the presence of an additional layer of tissue. Histologically it was confirmed that in all cases the cleavage occurred after the last row of stromal keratocytes. The layer in front of Descemet's membrane was histologically determined to be acellular, 10.15±3.6 µm thick, consisting of 5-8 plates of predominantly type 1 collagen, orderedly located in the transverse, longitudinal and oblique directions.
During the experimental work, scientists discovered a new, well-defined, acellular, durable layer of the cornea, located between the stromal layer and Descemet's membrane. The discovery of the Dua layer will have a significant impact on a more complete understanding of corneal biomechanics and the pathogenesis of diseases such as keratoconus, descemetoceles, corneal dystrophies, corneal bullous keratopathy, etc. Also, a more detailed study of the functions of the Dua layer can help in preventing the occurrence of complications of laser refractive surgery, in the treatment and prevention of pathological conditions of the cornea.
Therapeutic measures
All treatment methods for this pathological condition can be divided into the following groups:
- non-drug treatment;
- drug treatment;
- genetic engineering methods;
- extracorporeal treatment methods;
- folk remedies.
Non-drug therapy includes the following activities:
- weight normalization;
- to give up smoking;
- limiting the consumption of drinks containing high doses of alcohol;
- physical activity (moderate). The lesson plan for each patient is drawn up strictly individually;
- Diet for hypercholesterolemia is also very important. It is necessary to reduce the consumption of animal fats, but at the same time enrich your diet with dietary fiber and vitamins. You should also completely avoid eating fried and fatty foods.
Medicines for the treatment of pathology:
- statins;
- inhibitors of cholesterol absorption in the human intestine. The main task of these drugs is to reduce the absorption of cholesterol in the intestine;
- bile acid sequestrants;
- fibrates;
- omega-3 polyunsaturated fatty acids. These treatment agents are necessary because they significantly reduce the risk of heart rhythm disturbances and also prolong the life of patients who have previously suffered a myocardial infarction.
Extracorporeal methods of therapy are used only in severe forms of pathology. Their essence is that with the help of special innovative devices, the composition of the blood changes, as well as its properties (outside the human body).
Folk remedies for the treatment of pathology should be used only with the permission of your attending physician and in tandem with the methods of official medicine. The most effective folk recipes are from:
- Dioscorea nipponensis root;
- rose hips;
- sandy immortelle;
- leaves of watch trifoliate;
- milk thistle seed powder (an effective folk remedy);
- blue cyanosis roots;
- grass Tribulus creeping;
- celandine;
- prickly artichoke.
Anatomy of the cornea
- Function
- Composition of the cornea
- Structure of the cornea
- Physiology of the cornea
The cornea, or cornea, is convex in front and concave in back, a transparent, avascular plate of the eyeball, which is a direct continuation of the sclera. The human cornea occupies approximately 1/6 of the outer layer of the eye. It looks like a convex-concave lens, the place where it transitions into the sclera (limb) looks like a translucent ring up to 1 mm wide. Its presence is explained by the fact that the deep layers of the cornea extend posteriorly somewhat further than the anterior ones.
The diameter of the cornea is 11-12 mm in the horizontal plane and 9-11 in the vertical plane. In the center its thickness is 450-600 microns, and at the periphery - 650-750 microns. This indicator also correlates with age: for example, at 20-30 years old, the thickness of the cornea is 0.534 and 0.707 mm, and at 71-80 years old - 0.518 and 0.618 mm.
Distinctive qualities of the cornea:
- Spherical (radius of curvature of the front surface ~7.7 mm, rear surface 6.8 mm)
- Mirror shiny
- Lacking blood vessels
- Has high tactile and pain, but low temperature sensitivity
- Refracts light rays with a power of 40-43 diopters.
Function
The cornea is the optical structure of the eye; its refractive power is, on average, 45D (diopters) in children in the first year of life, and by the age of 7, as in adults, it is about 40D. The refractive power of the cornea in the vertical meridian is slightly greater than in the horizontal one (physiological astigmatism).
Dimensions
- The horizontal diameter in adults is 11 mm (in newborns - 9 mm).
- Vertical diameter - 10 mm, in newborns - 8 mm.
- The thickness in the center is 0.4-0.6 mm, in the peripheral part - 0.8-1.2 mm.
- The radius of curvature of the anterior surface of the cornea in adults is 7.5 mm, in newborns - 7 mm.
The cornea grows by thinning and stretching the tissue.
Composition of the cornea
The corneal epithelium develops from the ectoderm, all other elements of the cornea - from the neuroectoderm (neural crest). After invagination of the lens, the corneal stroma is formed in the form of a layer of loose collagenous substance between the ectoderm and the lens. At approximately 6 weeks of intrauterine development, mesenzymal cells from the perilimbal cell mass begin to form endothelium, and the stroma is populated by perilimbic fibroblasts (future keratocytes). By the time of birth, the cornea is relatively enlarged relative to other structures of the eyeball; corneal growth ends by 2 years of age.
The cornea contains water, collagen of mesenchymal origin, mucopolysaccharides, proteins (albumin, globulin), lipids, and vitamins. The transparency of the cornea depends on the correct location of the structural elements and the same refractive indices, as well as the water content in it (normally up to 75%; an increase in water above 86% leads to clouding of the cornea).
Changes in the cornea in old age
- the amount of moisture and vitamins decreases,
- globulin fractions of proteins predominate over albumin fractions,
- calcium salts and lipids are deposited.
In this regard, the area of transition of the cornea into the sclera, the limbus, changes first of all: the surface layers of the sclera seem to move onto the cornea, and the internal ones lag behind somewhat; the cornea becomes like glass inserted into a watch bezel. Due to metabolic disorders, a so-called senile arch is formed, and the sensitivity of the cornea decreases.
Structure of the cornea
- The surface layer of the cornea is squamous stratified epithelium, which is a continuation of the connective membrane of the eye (conjunctiva). The thickness of the epithelium is 0.04 mm. This layer regenerates well and quickly when damaged, without leaving cloudiness. The epithelium performs a protective function and is a regulator of water content in the cornea. The corneal epithelium, in turn, is protected from the external environment by the so-called liquid, or basal, layer.
- The anterior limiting plate - Bowman's membrane is loosely connected to the epithelium, so in case of pathology the epithelium can easily be torn off. It is structureless, inelastic, homogeneous, has a low level of metabolism, and is not capable of regeneration, so when it is damaged, opacities remain. The thickness in the center is 0.02 mm, and less at the periphery.
- The cornea's own substance (stroma) is a thick, transparent middle layer consisting of thin connective tissue, regularly located plates containing collagen fibrils, in which single wandering cells are located - fibroblasts and lymphoid elements that perform a protective function. They are parallel and overlap each other like the pages of a book. To better connect them, mucoprotein is located in the spaces between the layers. The stroma is up to 0.5 mm thick, nonvascular, and composed of approximately 200 layers of mostly type I collagen fibrils.
- The posterior limiting elastic lamina (Descemet's membrane) is a thin acellular layer that serves as the basement membrane of the corneal endothelium, from which all cells develop. This layer consists mainly of type IV collagen fibers, which are more elastic than type I collagen. The thickness of this layer is about 5-20 microns, depending on the age of the patient. Anterior to the Descimet membrane is a very thin but quite strong Dua layer, the thickness of which is only 15 microns, and the load capacity is from 1.5 to 2 bar of pressure, according to research.
- The endothelium is the inner part of the cornea, facing the anterior chamber of the eye and washed by the intraocular fluid. It consists of a single-layer squamous or cubic epithelium, the cells are rich in mitochondria, the thickness of the layer is about 0.05 mm. This layer protects the stroma from the direct effects of aqueous humor, simultaneously ensuring metabolic processes between it and the cornea, and has a pronounced barrier function (unlike the epithelium of the surface layer of the cornea, the endothelium does not regenerate; instead, there is a continuous division process that compensates for dead cells); participates in the formation of the trabecular apparatus of the iridocorneal angle.
Physiology of the cornea
The temperature of the cornea is approximately 10°C lower than body temperature, which is due to direct contact of the moist surface of the cornea with the external environment, as well as the absence of blood vessels in it. With closed eyelids, the temperature of the cornea at the limbus is 35.4 °C, and in the center 35.1 °C (with open eyelids ~30 °C).
In this regard, the growth of mold fungi with the development of specific keratitis is possible.
Since there are no lymphatic and blood vessels, nutrition and metabolism in the cornea occurs by osmosis and diffusion (due to tear fluid, anterior chamber moisture and pericorneal blood vessels).
The absence of blood vessels in the cornea is compensated by abundant innervation, which is represented by trophic, sensory and autonomic nerve fibers. Metabolic processes in the cornea are regulated by trophic nerves arising from the trigeminal and facial nerves.
The high sensitivity of the cornea is provided by a system of long ciliary nerves (from the ophthalmic branch of the trigeminal nerve), which form the perilimbal nerve plexus around the cornea. As they enter the cornea, they lose their myelin sheath and become invisible. Three tiers of nerve plexuses are formed in the cornea - in the stroma, under the basal (Bowman's) membrane and subepithelial. The closer to the surface of the cornea, the thinner the nerve endings become and the denser their interweaving. Almost every cell of the anterior corneal epithelium is provided with a separate nerve ending. This explains the high tactile sensitivity of the cornea and the pronounced pain syndrome when the sensitive endings are exposed (epithelial erosion).
The high sensitivity of the cornea underlies its protective function: when you lightly touch the surface of the cornea and even when the wind blows, an unconditioned corneal reflex occurs - the eyelids close, the eyeball turns upward, moving the cornea away from danger, and a tear fluid appears, washing away dust particles.
The afferent part of the corneal reflex arc is carried by the trigeminal nerve, and the efferent part is carried by the facial nerve. Loss of the corneal reflex occurs with severe brain damage (shock, coma). The disappearance of the corneal reflex is an indicator of the depth of anesthesia. The reflex disappears with some lesions of the cornea and upper cervical spinal cord.
The rapid direct response of the vessels of the marginal lemniscus to any irritation of the cornea occurs due to the fibers of the sympathetic and parasympathetic nerves present in the perilimbal nerve plexus. They are divided into 2 endings, one of which passes to the walls of the vessel, and the other penetrates the cornea and contacts the branched network of the trigeminal nerve.
Prevention
Prevention of hypercholesterolemia can be divided into primary and secondary. Primary prevention is the methods that should be used to prevent cholesterol levels in the bloodstream from increasing. Such events include:
- normalization of body weight;
- blood pressure control;
- do not drink alcoholic beverages and do not smoke;
- follow a special diet low in salt and fat;
- regular physical activity;
- avoid stressful situations;
- normalize blood sugar levels;
- timely and adequate treatment of pathologies that can provoke dyslipidemia.
Secondary prevention of hypercholesterolemia:
- the use of pharmaceuticals to normalize cholesterol levels;
- balanced diet;
- physical activity.
What to do?
If you think you have hypercholesterolemia
and symptoms characteristic of this disease, then doctors can help you: therapist, endocrinologist.
Source
Did you like the article? Share with friends on social networks: