In ophthalmology, a separate (and special) group of diseases consists of the so-called retinopathy - organic degenerative lesions of the retina caused by acute or chronic deficiency of its blood supply. Accordingly, retinopathy is classified according to the etiopathogenetic criterion, i.e. depending on the causes and mechanisms leading to the failure of the choroid feeding the retina.
Thus, diabetic, hypertensive, traumatic and some other forms of retinopathy are distinguished.
Postthrombotic retinopathy, as the name suggests, is inextricably linked to thrombosis of intraocular blood vessels; in most cases it is a thrombus in the central retinal vein or one of its branches. The postthrombotic type of retinopathy is considered in this context - not as an independent, autonomously occurring disease, but as a secondary pathology, which is a complication and consequence of thrombosis.
What it is?
Postthrombotic retinopathy is a group of ophthalmological diseases that develop against the background of venous thrombosis directly in the retina. This pathology directly occurs approximately three months after the development of thrombosis directly on the central vein supplying the retina (happens in every third case) or on one of its small branches (usually the superotemporal vein is affected).
The development of thrombosis in the central artery causes rapid blindness in the eye that it supplies, and if the problem involves a branch, then a certain field is lost. The reduction in severity increases gradually over a couple of days, requiring prompt seeking of help. As a rule, if one of the branches is affected by thrombosis, then visual acuity is at the level of 0.1 or higher, and if the central vein is affected, then its quality is at the level of the ability to count fingers on a hand near the eyes or lower. Also, in every fifth case, thrombosis from the branch can progress to the central one with the risk of developing complete blindness.
Causes of postthrombotic retinopathy
The risk of retinal vascular thrombosis increases significantly with arterial hypertension, diabetes mellitus, atherosclerosis, heart rhythm disturbances, activation of chronic infections in the body, blood pathologies (increased coagulability), as well as autoimmune systemic diseases. In addition, very often thrombus formation occurs against the background of inflammatory processes, tumors and eye injuries, and glaucoma.
The main source of all pathological changes in the retina during arterial thrombosis is a state of acute hypoxia. When occlusion occurs at the level of the veins, the mechanism for the development of retinopathy is more complex. In this case, blood stagnation occurs, which leads to a change in vascular permeability. Blood leaves the bloodstream, hemorrhage and swelling of the retina occurs, which subsequently causes the growth of new pathological vessels.
Retinal vascular occlusion is a common cause of vision loss in elderly patients suffering from arterial hypertension, atherosclerosis or diabetes mellitus. As a rule, it manifests itself with sudden unilateral vision loss. In elderly patients, occlusion may not be detected immediately, but only after some time. During a detailed examination of the patient in order to detect concomitant pathology, clinically previously undetected vascular diseases of the brain or heart are often diagnosed.
Central artery thrombosis causes instant blindness in the affected eye. In case of thrombosis of a branch of the central artery, a certain field of vision may be lost.
A blood clot in the central retinal vein causes gradual loss of vision, which fades over several days. Venous occlusions have varying degrees of severity. At the same time, the prognosis for vision is always associated with the localization of the lesion and the extent of the zone of retinal ischemia.
With non-ischemic retinal occlusion, visual acuity is usually above 0.1. With ischemic, this is the ability to count fingers near the face or below. In 20% of cases of thrombosis, non-ischemic central vein occlusion may progress to ischemic occlusion.
Thrombosis development process
The clinical picture of the formation of postthrombotic retinopathy includes the following main stages:
- Pre-thrombosis stage, accompanied by dilation of the veins themselves and circulatory disorders with isolated hemorrhages directly throughout the fundus of the eye or venous stagnation.
- A slight drop in visual acuity and the regular appearance of a feeling of fog in the eyes.
- The thrombotic stage, at which the veins darken, the arteries narrow, and traces of blood effusions are found in the vitreous body and directly on the retina. At this stage, the border of the main optic nerve is blurred and persistent swelling of the macular zone is observed.
- A sharp drop in visual acuity with the appearance of a constant feeling of a white veil in the eyes, a reduction in the field of vision.
- Direct formation of postthrombatic retinopathy.
Thrombotic retinopathy of the eye
An increased risk of developing pathologies is observed in people suffering from the following diseases:
- atherosclerosis;
- hypertension;
- diabetes;
- arrhythmia;
- any systemic autoimmune pathologies;
- disturbances in hemostasis;
- glaucoma;
- eye injuries of any nature;
- infections.
People over 40 years of age are most susceptible to developing the disease. Low physical activity, excess weight, alcohol abuse, and smoking increase the risk of developing postthrombotic retinopathy.
Postthrombotic retinopathy. Features of diagnostics. Symptoms
The main danger of the pathology remains minimal or completely absent symptoms in the early stages of development. Over time, a clearly visible clinical picture appears in a short time, including the following symptoms:
- a sharp decrease in visual acuity;
- feeling of a foreign body in the affected eye;
- double vision or blurred vision in the affected eye.
Failure to promptly contact an ophthalmologist can lead to the development of hemorrhage or general hemophthalmos against the background of increased blood pressure in the damaged branch. The result is retinal atrophy with detachment, which leads to complete and irreversible blindness, so it is important to regularly consult an ophthalmologist for diagnosis. Upon examination, a specialist may detect the following precursors of postthrombotic retinopathy:
- Long-standing blood micro-effusions in the fundus in the form of red dots or spots (usually traces in the form of smears or flames resolve over time).
- The presence of arteriovenous veins, vascular arcades, collaterals that connect parts of veins affected by thrombosis, allowing blood to flow out of the affected area.
- Venous vessels affected by microaneurysms that have slight tortuosity (these symptoms are most typical already at the stage of developed pathology);
- Macular edema, which develops against the background of a chronic lack of blood supply and leads to a deterioration in central vision.
Symptoms of acute thrombosis of retinal vessels
In the early stages, the process of thrombus formation progresses quite slowly and asymptomatically. Then the pathology accelerates, at a certain point manifesting itself with a pronounced clinical picture: the sharpness and clarity of vision drops sharply, a sensation of a foreign body in the eye occurs (this symptom cannot be considered specific, since it is inherent in almost any ophthalmological pathology). Many patients complain of double vision or blurring in the affected eye; due to a sharp increase in pressure in the thrombosed vascular branch, retinal hemorrhages of varying intensity or general hemophthalmos are likely.
The mechanisms of organic degeneration of retinal tissue in the case of acute ischemia (cessation of blood supply) are akin to the processes that occur during a heart attack or ischemic stroke - and just as catastrophic. In this case, the situation is complicated by the fact that the retinal tissue is a highly specialized and very vulnerable formation of several microscopic cell layers (photosensitive rods and cones, known from school). The outcome of retinal dystrophy/atrophy is its detachment, resulting in irreversible blindness, and neither the transplantation of a donor retina nor the implantation of an artificial one are currently among the methods developed and practiced in ophthalmology: in the last 3-4 years, only the first relatively successful experiments in this area.
Therefore, the following are extremely important:
- regular preventive examinations with an ophthalmologist (for people at risk such periodic consultations are mandatory);
- preventing the thrombosis process from becoming chronic: contacting an ophthalmologist and the measures taken should be immediate, since chronic forms of thrombosis of the retinal vessels are practically untreatable and result in the most detrimental consequences for the retina;
- measures to prevent the long-term consequences of thrombosis as much as possible, i.e. progression of postthrombotic retinopathy itself.
It should be especially emphasized that conditions of acute thrombosis and occlusion of the central retinal vein must be treated in a hospital setting; the period of constant observation, intensive treatment and monitoring of dynamics usually takes at least 8-10 days.
Development of the disease in the absence of therapy
In case of untimely diagnosis and unfavorable course of the disease, within 3 months after the development of the pathology, the following changes quickly increase in the retina of the eye:
- the appearance of vascular local protrusions (aneurysms);
- hyperpigmentation;
- degeneration at the cellular level;
- swelling;
- accumulation of exudate;
- splicing according to the principle of forming ties.
With prolonged blocking of normal blood supply, a new network of vessels is formed, the purpose of which lies in the desire to restore normal tissue nutrition. This occurs due to the growth of blood vessels directly into the vitreous body of the eye, which puts serious pressure on nearby tissues, and this leads to an additional deterioration of the situation. The end result of postthrombotic retinopathy without adequate treatment is retinal detachment and irreversible vision loss.
Postthrombotic retinopathy – relevance of the disease
The World Health Organization predicts an increase in diseases associated with blood microcirculation disorders in people who suffer from various cardiovascular pathologies. This is confirmed by Russian doctors, according to whose statistics the share of retinopathy of various types accounts for up to 55% of the total number of diseases of the optic nerve and retina in this category of patients. It is postthrombotic retinopathy that becomes one of the causes of optic nerve atrophy, and in 40-64% of cases it completely affects both eyes.
Postthrombotic retinopathy. Signs of the disease upon examination
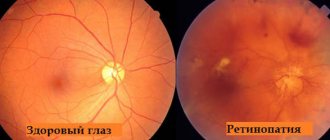
The first universal diagnostic method for suspected development of postthrombotic retinopathy remains ophthalmoscopy. If pathology is present, it reveals the following signs:
- severely narrowed arteries in the form of thin threads with segmental blood flow;
- pale color of the retina and the presence of edema on it;
- the presence of a bright red spot directly on the retina;
- the presence of new pathological blood vessels;
- formation of microaneurysms and hard exudates.
If there is a suspicion of progression of postthrombotic retinopathy, additional studies are prescribed. Fluorescein angiography remains a universal option here, allowing us to examine any changes in microscopic vessels and evaluate the process of capillary filling using a special contrast agent injected into a vein on the elbow through a catheter. With its help, you can assess the stage of the disease, clarify the diagnosis, and determine the presence of functional disorders in the fundus. This is the most reliable and effective way to assess the condition of the fundus and is carried out only for additional indications due to the relative complexity and lack of specialized equipment in ordinary medical institutions.
Another method of in-depth diagnostics is the use of optical coherence tomography, which allows you to effectively and with a high degree of reliability see the central zone of the retina of the eye, allowing you to assess the degree of damage to the optic nerve.
In addition to specialized diagnostic methods, during the examination, general visual acuity is assessed and the boundaries of the visual field are determined. Additional consultations with specialists on the treatment of concomitant diseases are also required, and general diagnostics are performed. This allows not only to determine the presence of the disease, but also to identify concomitant pathologies that cause the progression of postthrombotic retinopathy of the eye.
Treatment of retinopathy
The main thing in the treatment of secondary retinopathy is compensation for the disease that caused it. In parallel, direct treatment of retinal vascular changes is carried out using conservative and surgical methods. Their choice remains at the discretion of the doctor after diagnostic studies, in accordance with the type and stage of the identified disease.
In conservative treatment of retinopathy, treatment consists of instilling certain eye drops. These are, as a rule, solutions of vitamin complexes and hormonal preparations.
Widely used surgical treatment methods are laser and cryosurgical coagulation of the retina. If necessary, vitrectomy surgery may be prescribed.
In the case of retinopathy of prematurity, spontaneous recovery is possible in the early stages of the disease, which does not negate the mandatory observation of an ophthalmologist and pediatrician. In the absence of a spontaneous positive outcome of the disease, young patients may undergo laser photocoagulation of the retina, cryoretinopexy, scleroplasty or vitrectomy.
Of the physiotherapeutic methods of influence, the greatest effect in the treatment of certain types of retinopathy (diabetic, including) is shown by hyperbaric oxygenation - the effect of oxygen under high pressure on retinal tissue.
Features of the treatment of postthrombotic retinopathy
Therapy is aimed at solving three problems:
- elimination of existing hemorrhage;
- ensuring restoration of normal blood supply to the retina and normalization of its nutrition;
- relieving swelling to prevent the formation of new blood clots.
Treatment is prescribed depending on the specific situation, including drug therapy, laser coagulation and massage. To restore normal retinal trophism and prevent the development of thrombosis, the following types of drugs are used:
- anticoagulants;
- angioprotectors;
- antispasmodics;
- corticosteroids;
- drops to reduce intraocular pressure;
- antihypertensive drugs to normalize blood pressure;
- vitamin complexes.
Massage remains an effective way to restore blood supply to the eye, relieve swelling and accelerate the resorption of hemorrhage. In the first 6 hours after blockage of a vessel, it can be used to stimulate blood flow through small arteries, which will reduce the severity of the damage. It works like this:
- the patient lowers his head and closes his eyes;
- the eyeball is slightly pressed three times with a sharp separation;
- After 5-10 seconds, repeat pressing a little harder.
If during the development of retinopathy a larger number of new blood vessels have formed, then laser coagulation is performed to reduce the degree of edema, fluid penetration under the retina and removal of ischemic zones.
Typically, therapy is performed in a hospital setting and lasts 1.5-2 weeks, followed by regular visits (every 2 weeks) to an ophthalmologist for six months to assess the quality of pathology relief and prevent relapse.
Treatment
Therapeutic measures for occlusion of the central vein are aimed at restoring blood circulation in the retinal vessels and preventing new formation of blood clots. For this purpose, thrombolytics, drugs to reduce retinal edema, antiplatelet agents, agents that activate microcirculation (pentoxifylline), steroids and agents that help strengthen the walls of blood vessels, vitamins, and antispasmodics are prescribed.
To stop the growth of newly formed pathological vessels, laser coagulation is performed. Elimination of retinal edema and restoration of ischemic areas is ensured by intravitreal administration of anti-VEGF drugs, which are aimed at suppressing the growth factor of dysfunctional vessels. If retinal vein thrombosis is still fresh (up to 3-4 months), an excellent effect can be achieved by intravitreal administration of the hormonal implant Ozurdex (dexamethasone).
With thrombosis of the central retinal vein, in the future, patients need to monitor the condition of the retina and the level of intraocular pressure on a regular basis. This is caused by the risk of reappearance of pathological newly formed vessels on the retina, as well as in other ocular structures. If neovascularization affects the angle of the anterior chamber, the outflow of intraocular fluid is hampered, which can cause an increase in intraocular pressure - the development of glaucoma.
The specialists of our clinic have enough knowledge and practical experience to restore partial vision even in the most complex cases of retinal vascular occlusions. Thanks to the technical equipment of the center and the availability of all necessary drugs, patients have the opportunity to receive a full range of therapy that meets high international standards without the need for treatment abroad. Also, we accept patients for dispensary services and make every effort to ensure that such an eye catastrophe does not happen again, and other ophthalmological diseases are detected and eliminated as soon as possible.
Macular edema
Macular edema is a syndrome characterized by swelling of the central part of the retina, which is accompanied by visual impairment. This is not a separate pathology, as it develops against the background of one of the following diseases:
- central vein thrombosis;
- diabetes;
- consequence of a number of ophthalmological operations;
- retinal detachment;
- neoplasms in the eyes;
- glaucoma and so on.
The following symptoms indicate the development of macular edema:
- blurry image in the central visual area;
- increased photosensitivity and pain to bright light;
- pinkishness image;
- visual deformation of straight lines.
If detected early, macular edema does not lead to complete loss of vision, but recovery can take up to one year. If the problem has become chronic, persisting for more than 6 months, then irreversible changes in the receptors on the retina and their replacement with fibrous tissue occur, which leads to an irreversible decrease in vision in the central zone of the field. Against this background, it is important to timely contact an ophthalmologist for diagnosis and treatment of the disease.
Depending on the specific symptoms and the degree of development of the disease, macular edema is treated in one of the following ways:
- conservative;
- laser;
- surgical.
If the pathology is detected at the earliest stages and dystrophic changes in the trophism of the retina are still poorly expressed, then treatment may be limited to the use of the hormonal implant Ozurdex, administered intravitreally, for three to four months. The method involves injecting the drug directly into the vitreous, which provides the following advantages:
- targeted delivery of the active substance;
- minimal risk of systemic side effects;
- rapid achievement of the required therapeutic effect;
- minimum discomfort for the patient (local anesthesia with lidocaine drops is sufficient).
At the same time, such administration of the drug requires strict implementation of aseptic measures and procedure technology due to the risk of a number of side effects. This procedure itself can be performed on an outpatient basis without referral to a hospital (at the initial stage of thrombosis development, hospitalization is not necessary). After the injection, the patient is under short-term observation.
If the pathological process is already quite severe, then a complex of anti-inflammatory drugs, the introduction of endothelial growth factor inhibitors and long-acting glucocorticosteroids are prescribed. If this does not work or the swelling has already developed sufficiently, then laser coagulation of the retina may be prescribed, which improves blood circulation in the central part, strengthening it and improving overall vision. The procedure is performed as an outpatient appointment, and the process itself does not take more than 20 minutes. During coagulation, point cauterizations are performed, which are placed in a horseshoe shape around the central fossa.
Surgical treatment of macular edema is effective when the results of conservative or laser treatment are weak or temporary.
The prognosis for treatment of macular edema (as well as any other ophthalmological disease) is determined by the timeliness of seeking medical help, when complications have not yet developed. If this condition is met, it is possible to improve vision and return to a physically active healthy lifestyle. In advanced cases, the formation of retinal dystrophy, its ruptures, and the death of photoreceptors is possible, which leads to irreversible changes up to complete blindness.
Reasons for development
Thrombosis of retinal vessels can be caused by arterial hypertension, diabetes mellitus, atherosclerosis, heart disease, relapse of chronic systemic diseases, blood diseases (including increased blood clotting), and autoimmune diseases. Often thrombosis becomes a consequence of inflammatory processes, tumors, eye injuries, and glaucoma.
All pathological changes caused by arterial thrombosis occur due to acute hypoxia (oxygen starvation) of the retina. The occlusion observed at the level of veins has a more complex mechanism. Due to stagnation of blood, a violation of the permeability of the vascular wall occurs, blood leaves the bloodstream, hemorrhages occur in the retina, and its swelling, which ultimately leads to the formation and growth of new pathological vessels.
A common cause of vision loss, especially in elderly patients with hypertension, diabetes, and atherosclerosis, is occlusion of retinal vessels. It develops suddenly and, as a rule, in one eye. In very elderly people, it may not be detected immediately. Diagnosis requires a thorough examination to identify concomitant diseases. Usually, previously undetected pathologies of the heart and blood vessels, and in some cases of the brain, are discovered.
Thrombosis of the central retinal artery results in complete blindness, which occurs in the affected eye within minutes. If thrombosis occurs in one of the branches of the central retinal artery, a certain part of the visual field disappears.
If the central retinal vein is affected by thrombosis, vision disappears gradually (over several days). The severity of venous occlusions varies significantly. The prognosis for vision is directly related to the location of the lesion and the volume of the retina subjected to ischemia.
When non-ischemic occlusion is observed, the patient has slightly higher visual acuity (more than 0.1). With ischemic occlusion, this is the discrimination of fingers near the face or even lower. In approximately 20% of cases, a transition from non-ischemic occlusion to an ischemic form occurs.