The article talks about eye damage that occurs in patients with diabetes – retinopathy. Methods for diagnosing and treating the problem are described. Diabetic retinopathy is a common complication of diabetes, characterized by damage to the fundus of the eye. May lead to complete loss of vision. It is treated comprehensively along with diabetes therapy.
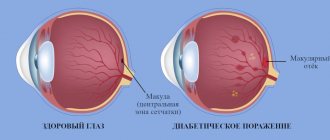
In diabetes, the vessels of the fundus of the eye are affected
General information
Diabetes mellitus is one of the most common diseases, affecting more than 5% of the world's population. With diabetes, the patient's blood sugar level increases, which affects the condition of all blood vessels in the body, as well as the vessels of the retina .
Retinal damage caused by diabetes is called diabetic retinopathy, which is the main cause of blindness and disability. The age of the patient plays an important role in the development of the disease. If diabetes mellitus was diagnosed before age 30, the incidence of retinopathy increases: after 10 years - by 50%, after 20 years - by 75%. If diabetes began after 30 years of age, then retinopathy develops faster and can appear after 5-7 years in 80% of patients. The disease affects patients with both insulin-dependent and non-insulin-dependent types of diabetes .
Retinopathy: what is it?
When incorrect or irregular correction of blood glucose levels in a patient with diabetes mellitus, vessels in different organs are primarily affected. Due to unstable glucose levels, it is in the walls of veins and arteries that disturbances in the metabolism of not only carbohydrates, but also proteins and fats begin.
This disorder is called diabetic angiopathy. Small-caliber vessels are most susceptible to it, and especially the microvessels of the retina, kidneys and lower extremities. Large vessels are affected less frequently. This condition is manifested by more pronounced atherosclerosis of the heart arteries and arteries of the lower extremities.
But the most common complications of diabetes are damage to the vessels of the retina of the eyeball and the vascular system of the kidneys, which are called retinopathy (from the Latin rete - network and from the Greek pathos - disease) and nephropathy (from the Greek nephros - kidney and pathos - disease) , respectively.
Now that we have figured out what retinopathy is in patients with diabetes, let's move on to its causes.
Reasons for the development of retinopathy
The main reason for the development of all diabetic angiopathy and retinopathy in particular is insufficient treatment of the underlying disease, that is, diabetes mellitus. This may be a deliberate violation of the patient’s regimen for taking glucose-lowering medications or an incorrectly prescribed dosage. Unstable blood glucose levels lead to metabolic disorders in blood vessels and hormonal balance.
Statistically, vision suffers more often in type II diabetes mellitus, especially in those patients who receive insulin therapy
Risk factors for the development of retinopathy are:
- age over 40 years,
- duration of diabetes (the longer the disease lasts, the higher the chance of developing retinopathy),
- arterial hypertension,
- concomitant kidney damage,
- concomitant atherosclerosis,
- pregnancy (during pregnancy, retinopathy progresses faster or may debut).
Stages of diabetic retinopathy
Diabetic retinopathy consists of several stages. The initial stage of retinopathy is called nonproliferative , and is characterized by the appearance of microaneurysms that dilate the arteries, pinpoint hemorrhages in the eye in the form of dark round spots or streak-like stripes, the appearance of ischemic zones of the retina, retinal edema in the macular area, as well as increased permeability and fragility of the vascular walls. In this case, the liquid part of the blood enters the retina through thinned vessels, leading to the formation of edema. And if the central part of the retina is also involved in this process, then a decrease in vision .
It should be noted that this form of diabetes can occur at any stage of the disease, and represents the initial stage of retinopathy. If it is not treated, then the transition to the second stage of the disease occurs.
The second stage of retinopathy is proliferative , which is accompanied by impaired blood circulation in the retina, which leads to oxygen deficiency in the retina ( oxygen starvation , ischemia ). To restore oxygen levels, the body creates new blood vessels (this process is called neovascularization ). The newly formed vessels are damaged and begin to bleed, causing blood to enter the vitreous body , the layers of the retina. As a result, floating clouds appear in the eyes against the background of decreased vision.
In the later stages of retinopathy, as new blood vessels and scar tissue continue to grow, it can lead to retinal detachment and the development of glaucoma .
The main reason for the development of diabetic retinopathy is an insufficient amount of insulin , which leads to the accumulation of fructose and sorbitol , which contribute to increased pressure, thickening of capillary walls and narrowing of their lumens.
What is diabetic retinopathy and how is it treated?
Diabetes mellitus is a dangerous disease that affects almost all organ systems. If you ignore its effect on vision, you may face complete blindness. Fortunately, timely diagnosis allows you to avoid many problems.
Elena Valerievna Burlakova, an ophthalmologist at the Expert Clinic Irkutsk, told us about such a complication of diabetes as diabetic retinopathy.
— Elena Valerievna, what kind of disease is diabetic retinopathy?
— This is the name of a nonspecific vascular complication of diabetes mellitus that affects the retina of the eye.
— What is the mechanism of its occurrence and development?
— As you know, diabetes can be type I (due to decreased insulin levels) and type II (due to decreased sensitivity of cells to insulin). In any case, the level of glucose in the blood increases, this leads to a pathological effect on the blood vessels. Swelling of the vascular walls occurs, which causes the lumen of the blood vessels to narrow. As a result, the retinal tissue experiences hypoxia (lack of oxygen). As a result, tissues deprived of a normal flow of oxygen produce an increased amount of vascular growth factor, and neovascularization occurs - a pathological proliferation of defective vessels. However, these new vessels do not improve blood supply to the tissue, but only aggravate the situation - they are very fragile. The permeability of the vascular walls also increases, so retinal edema and hemorrhages into the vitreous are possible. Due to frequent hemorrhages and chronic ischemia, tissue degeneration occurs.
— Is this a reversible process?
— The concept of reversibility here is very conditional. Timely treatment can preserve vision. However, changes that have already occurred cannot be “undone.” There will be no complete recovery or return to the original state.
— Tell us about the classification of diabetic retinopathy.
— There are several classifications. The most popular division of diabetic retinopathy into non-proliferative and proliferative. Nonproliferative retinopathy is characterized by hemorrhages and hard exudates in the retina. The main sign of the proliferative form is pathological proliferation of blood vessels. The prognosis for the nonproliferative form is usually more favorable. Each form of diabetic retinopathy has several stages.
The non-proliferative form has three stages. The first (initial) is characterized by local manifestations. During the second stage, changes occur in the entire fundus of the eye. In the third, severe stage, serious vascular anomalies and ischemic zones appear. Another name for the third stage, adopted in domestic practice, is preproliferative.
Proliferative diabetic retinopathy is divided into five stages. In the first (initial) neovascularization spreads only across the retina. At the second (moderate) and third (severe) stages, the area of pathologically formed vessels increases, the process of neovascularization affects the optic nerve head. The fourth (far advanced) are characterized by even greater proliferation of blood vessels, the appearance of severe complications (hemophthalmos, retinal detachment, neovascular glaucoma). The fifth stage is the outcome of the disease, blindness.
— Are all people with diabetes equally susceptible to retinopathy or are there separate risk groups?
— First of all, the likelihood of diabetic retinopathy is associated with the duration of diabetes mellitus. According to statistics, after 10 years from the onset of diabetes, retinopathy occurs in 60% of patients, after 15 years – in 80%. But there are additional provoking factors.
The main one is uncontrollably high glucose levels. It is not so much the glucose level itself that is important, but the glycated hemoglobin indicator. If it exceeds 10%, the risk of blindness becomes extremely high. Therefore, you should always monitor your glucose level, avoiding sudden changes. If the decrease is too rapid, transient diabetic retinopathy may occur. The safe rate of reduction in glycated hemoglobin levels is 2% over 6 months.
Another important factor is arterial hypertension. Again, uncontrolled hypertension is especially dangerous. For hypertension, a sustained reduction in blood pressure of 10 millimeters of mercury reduces the risk of retinopathy by 12%.
Smoking greatly influences the likelihood of vascular disorders in diabetes mellitus. It worsens hypoxia. In people who smoke, not only does the risk of developing proliferative retinopathy increase, but also the risk of diabetic foot.
— What are the symptoms of diabetic retinopathy?
— In the initial stages, it is characterized by an asymptomatic course. This is the insidiousness of the disease. When the pathological process has reached significant proportions, a persistent, progressive decrease in vision appears. Complications of diabetic retinopathy: hemophthalmos (vitreous hemorrhage), retinal detachment, neovascular glaucoma. Hemophthalmos is manifested by decreased vision and flickering of flies. With retinal detachment, these symptoms are accompanied by loss of visual fields. Neovascular glaucoma may be accompanied by pressing pain in the eyes.
— What examinations are needed for timely diagnosis of diabetic retinopathy?
— Since the disease is often asymptomatic, diabetes mellitus requires regular examination by an ophthalmologist. During the examination, visual acuity is checked, intraocular pressure is measured, gonioscopy (examination of the angle of the anterior chamber of the eye), biomicroscopy, ophthalmoscopy (examination of the fundus). Ophthalmoscopy is performed only on a wide pupil: mydriatics (drops that dilate the pupil) are used, allowing a detailed examination of the internal structures of the eye.
The frequency of screening depends on the type of diabetes and the patient's condition. In type I diabetes mellitus, retinopathy usually does not occur in children under 12 years of age. Therefore, up to 12 years of age, a visit to an ophthalmologist is not required for this purpose.
But pregnancy can accelerate the course of diabetes and provoke the development of complications. Therefore, women with diabetes should be examined when planning pregnancy, then in each trimester, as well as in the third and sixth months after childbirth.
Other people over 12 years of age with uncomplicated diabetes should visit an ophthalmologist once a year. If stage 1 or 2 nonproliferative retinopathy is detected, a visit to the doctor is necessary once every 6 months. If the disease progresses, enters the preproliferative stage or becomes proliferative, specific treatment is started.
— What is the treatment for diabetic retinopathy?
— For stages 1 and 2 of nonproliferative retinopathy, compensation for the underlying disease—diabetes mellitus—is most effective. When identifying vascular abnormalities and neovascularization, the main treatment method is laser coagulation. During this operation, a person with diabetic retinopathy applies many microcoagulants (microcauteries) across the entire surface of the retina. This stops the growth of pathologically altered vessels. The operation is always carried out in several stages, the number of procedures depends on the degree of damage to the eye and the features of the device. The optic disc, macular area (the area of the retina with the best visual acuity) and blood vessels are not coagulated.
Now in ophthalmology the era of VEGF (Vascular endothelial growth factor) blockers has arrived. They cannot be an independent method of treating diabetic retinopathy, but are effective as additional therapy for laser coagulation. In addition to treating retinopathy, these drugs are used for macular edema and can reduce retinal edema and vascular wall permeability.
Complications also require treatment. If hemophthalmos has not resolved within a month, as well as in case of retinal detachment, a posterior vitrectomy is performed - an operation to remove the vitreous body. For neovascular glaucoma, the range of interventions may include transscleral cyclocoagulation (laser cauterization of the ciliary body) and implantation of various models of anti-glaucoma drainages.
In severe cases, with a strong persistent increase in intraocular pressure, cryodestruction of the ciliary body is performed. But this is more of a desperate operation: it is needed to combat pain and cosmetically preserve the eye, but it will not help restore vision.
— Tell us about measures to prevent diabetic retinopathy.
— With diabetes, it is important to control blood sugar levels, to avoid either a persistent increase or sudden changes. It is also necessary to monitor blood pressure, and if hypertension occurs, take medications to lower it. In addition, lipid metabolism must be under control: it is necessary to take into account both the total level of lipoproteins and the ratio of low- and high-density lipoproteins.
Be sure to avoid smoking.
You should follow a schedule of visits to the ophthalmologist.
You can make an appointment with an ophthalmologist here. ATTENTION: the service is not available in all cities
Interviewed by Daria Ushkova
For reference:
Burlakova Elena Valerievna
Graduated from the Faculty of General Medicine of Irkutsk State Medical University in 1998.
1998 – 1999 – internship, and 2002 – 2004 – residency in the specialty “Ophthalmology” at the Irkutsk State Institute for Advanced Medical Studies.
Currently, he is an ophthalmologist, a laser surgeon of the highest qualification category at the Expert Clinic, Irkutsk. Receives at the address: Kozhova street, 9A.
Symptoms of diabetic retinopathy
The main symptoms of retinopathy depend on the stage of the disease. Typically, patients complain of blurred vision, the appearance of dark floating clouds in the eye (gnats), and sudden loss of vision. It is important to note that the sharpness of vision depends on blood sugar levels. However, in the initial stages of retinopathy, visual disturbances are practically not observed, so patients with diabetes should undergo regular ophthalmological examinations to identify the first signs of the disease.
Diagnosis of diabetic retinopathy
People suffering from diabetes should undergo regular eye examinations, which makes it possible to detect the development of eye complications in the early stages and begin timely treatment. Diabetics should be under constant supervision not only of a therapist and endocrinologist, but also of an ophthalmologist.
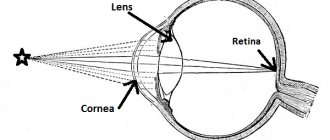
The diagnosis of diabetic retinopathy is made based on the patient's complaints of decreased vision and examination of the fundus using an ophthalmoscope . Ophthalmoscopy allows you to identify pathological changes in the fundus. Ophthalmological examinations include determination of the level of intraocular pressure, biomicroscopy of the anterior part of the eye.
In addition, photographing of the fundus is carried out using a fundus camera , which allows you to document changes in the retina, as well as fluorescein angiography to determine the location of the vessels from which fluid is released and causes macular edema . Biomicroscopy of the lens is performed using a slit lamp.
Treatment
Treatment of diabetic retinopathy should be carried out against the background of adequate therapy for diabetes mellitus. Improvement in the condition can only be achieved by maintaining optimal blood sugar levels.
Treatment methods for pathology include the use of medications and surgical interventions.
Drug therapy
Drug treatment of pathology is carried out jointly by endocrinologists and ophthalmologists. The endocrinologist prescribes adequate therapy for diabetes. An ophthalmologist deals directly with vascular disorders.
Table. Treatment of non-proliferative diabetic retinopathy with medications:
| Group of drugs | Therapeutic effect | Mode of application |
| Antioxidants – Mexiprim | Improve microcirculation and oxygen supply to tissues | Orally or by injection |
| Vitamins A and B | Helps preserve rods and cones in the retina | Orally or eye drops |
| Angioprotectors - Ascorutin | Reduces the permeability of the vascular wall | Inside |
| Immunostimulants – Cycloferon | Improves the body's protective properties | Orally or a course of injections |
| Biogenic stimulants - aloe extract | Protects tissues from damage, promotes regeneration | Course of injections |
Taking medications can last for a long time.
Surgical treatment
Treatment of diabetic retinopathy with progression of vascular changes is carried out using surgical intervention. The main method of treatment is laser coagulation of the retina.
There are several types of it:
- barrier – used for macular edema, involves laser cauterization around the macula;
- focal – changes detected during angiography are cauterized in a point;
- panretinal - used at the preproliferative stage, cauterization is performed along the entire perimeter of the retina.
At a pronounced proliferative stage, accompanied by severe bleeding, vitrectomy is performed. During this operation, the vitreous body and spilled blood are removed and the bleeding vessels are cauterized.
Laser coagulation is carried out at different stages
Prevention of diabetic retinopathy
Prevention of retinopathy is maintaining normal blood sugar levels in diabetics, optimal compensation of carbohydrate metabolism, blood pressure control, and correction of lipid metabolism. This helps reduce possible eye complications.
Proper nutrition and regular exercise have a positive effect on the general condition of patients with diabetes. It is also important to have regular checkups with your eye doctor. Timely prevention of diabetic retinopathy and eye damage in diabetes mellitus is very important. Since in the later stages of the disease treatment is not effective. However, due to the fact that visual disturbances are not observed in the initial stages of retinopathy, patients seek help when extensive hemorrhages and changes in the central zone of the retina already occur.
Diagnostics
At the first sign of visual impairment, you should consult a doctor. An ophthalmologist will perform a series of diagnostic procedures to identify the cause of the disease and the severity of the condition.
These include:
- consultations with an ophthalmologist and doctors treating concomitant diseases (endocrinologist, cardiologist, etc.);
- laboratory tests (CBC, blood glucose levels, etc.);
- fluorescein angiography of the retina;
- ophthalmoscopy (direct and indirect);
- biomicroscopy;
- visometry;
- perimetry;
- Ultrasound;
- electroretinography;
- laser tomography.
Diagnosis can also be carried out based on the concomitant underlying pathology to more fully collect information and adjust the chosen course of therapy.
List of sources
- Vorobyova I.V., Merkushenkova D.A., Estrin L.G., Kalinina N.I., Ivanova D.P. Molecular mechanisms of the pathogenesis of diabetic retinopathy and maculopathy. // XI All-Russian School of Ophthalmology: collection of scientific papers. - M., 2012;
- Balashevich L.I. Ocular manifestations of diabetes / L.I. Balashevich, V.V. Brzhesky, A.S. Izmailov and others; Ed. L.I. Balashevich. - St. Petersburg: Publishing House St. Petersburg MAPO, 2004;
- Astakhov Yu.S., Shadrichev F.E., Lisochkina A.B. Diabetic retinopathy (patient management tactics) // Clinical ophthalmology. - M., 2004.