Advantages of installing corneal segments
- The progression of keratoconus is stabilizing.
- There are no restrictions in physical activity.
- After implantation, a quick return to your normal lifestyle is possible.
- The rings can be adjusted and removed.
- The material from which the rings are made is absolutely biocompatible with eye tissue.
- It is possible to use contact lenses.
- There are no age restrictions for the installation of intrastromal rings.
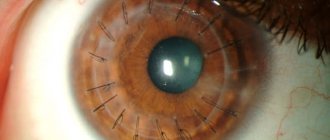
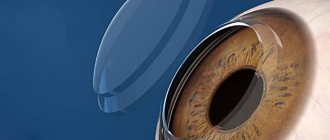
Fig. 1 Appearance of segments installed in the cornea (enlarged)
Advantages of using implantation of intrastromal segments
The operation of intrastromal keratoplasty has a number of significant advantages over other types of surgical vision correction:
All this gives the operation of implantation of intrastromal rings wide popularity and makes it increasingly in demand.
Types of intrastromal rings
There are two types of intrastromal rings available today:
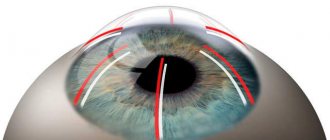
- Intacs (Intax) , having a hexagonal cross-section, which are implanted along the periphery of the cornea
- Ferrara (Ferrara) and Keraring (Keraring) , which have the shape of a triangular prism and are installed in the central zone.
- MyoRing (Mayoring) is a complete ring.
Fig. 2 Intacts and Keraring intrastromal corneal segments - position in the eye
The difference between Ferrara and Keraring intrastromal corneal rings and Intacs is that they have a smaller radius of curvature (for the latter it varies from 2.5 to 3.5 mm, and for the former it is strictly 2.5 mm), and is also less likely to the occurrence of glare after their installation due to their prismatic shape. Any ray of light that hits the ring is reflected in the opposite direction so that it does not fall into the field of view. Ferrara Rings are located closer to the center of the cornea, and due to their smaller size, they can provide a more significant effect - correcting myopia down to -12 D. It is impossible to achieve such a large effect using Intacs rings. Although it should be noted that with a large pupil diameter, some patients experienced glare. In these cases, implantation of Intacs rings is recommended.
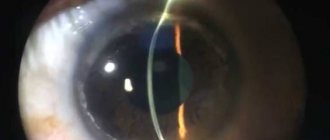
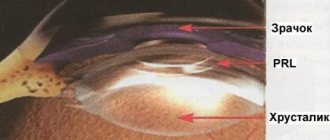
Fig. 3 Appearance of a rigid contact lens (RCL) and the corneal ring MyoRing
How vision correction occurs when installing intrastromal rings
The desired effect from implantation of intrastromal segments is achieved due to the pressure they exert, which is directed from the center of the cornea outward. This pressure causes the conical shape of the apex of the cornea to flatten, and it takes on a shape close to natural, which has a positive effect on visual functions.
When the cornea is abnormally curved, light rays passing through it are unable to focus on the retina, which makes vision unclear and blurry. Implantation of intrastromal segments makes it possible to gently correct the shape of the cornea, and light rays begin to converge on the retina. As a result, vision becomes clear and crisp.
Corneal segments for myopia and astigmatism
Implantation of intrastromal rings is indicated for people with mild to moderate myopia. It is a gentle option for vision correction that preserves corneal tissue. In addition, the technique is completely reversible: if necessary, the implants can be replaced or completely removed in the future. The significant advantages of intrastromal keratoplasty include a short period of postoperative recovery and an immediate significant improvement in vision.
This method can be offered to patients with myopia up to – 3D, as well as astigmatism not exceeding 1.0D. However, it should be taken into account that before the operation the patient’s vision must be stable for a year.
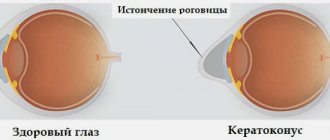
Corneal segments in keratoconus
The most common indication for intrastromal keratoplasty is keratoconus. Intrastromal keratoplasty is necessary to strengthen the cornea and improve visual function. With keratoconus, the cornea weakens and thins, losing its natural shape, which leads to loss of visual acuity. Implantation of corneal rings helps prevent the progression of this disease, preventing it from reaching a stage at which an invasive and complex corneal transplant surgery is necessary.
Contraindications for surgery
Intrastromal keratoplasty is a minimally invasive, practically safe operation. However, there are some contraindications to its implementation, such as:
- The patient is a minor.
- Infectious and inflammatory eye diseases in the acute period.
- Insufficient thickness of the central zone of the cornea (up to 370 microns).
- Cloudiness of the cornea.
- The last stage of keratoconus.
Progress of corneal segment implantation surgery
Before the procedure for implantation of corneal rings, the patient must undergo a comprehensive ophthalmological examination with computer keratotopography. A week before surgery, you need to stop wearing soft contact lenses and switch to glasses (for users of hard contact lenses, this period is 2 weeks).
Intrastromal keratoplasty is performed on an outpatient basis using local anesthesia. The average operation time for one eye is 15 minutes.
After the anesthetic is instilled, an eyelid dilator (blepharostat) is applied to the eye, which will prevent the patient from blinking. A very small incision is made along the surface of the cornea. Using a surgical instrument or a femtosecond laser, two microtunnels for semicircular implants are made in the corneal layers.
To better understand the process, it is worth imagining multilayer corneal tissue as a stack of sheets of paper that will be pulled apart. When installing an implant, these ultra-thin arcs are introduced between the stroma layers into the formed tunnels. The operation is completed by applying anti-inflammatory and antibacterial drops to the eye. The patient will have to use these same drops for another 2-3 weeks after surgery.
IRS installation video
Benefits of the operation
- Segments can be reimplanted (removed), after which the cornea returns to its preoperative state or replaced with more suitable ones (implantation is possible 3 months after the first procedure).
- Rapid restoration of visual functions in the postoperative period.
- Postponement of penetrating keratoplasty for keratoconus or its complete exclusion.
- There is no removal of corneal tissue in the optical zone, unlike excimer laser vision correction.
- The natural shape of the cornea and its integrity are preserved.
- Implants are almost imperceptible and unnoticeable.
- No special care is required for intrastromal segments.
Possible complications
Implantation of corneal segments is a generally safe operation, with a minimum of possible complications. And yet, such complications exist, these include:
- Development of infection.
- Fluctuations in visual acuity.
- Deterioration of dark adaptation.
- The appearance of glare and halos.
- Displacement of segments, their exit outside.
In the case of treatment of keratoconus using intrastromal keratoplasty, additional vision correction may be necessary in the postoperative period. In complex forms of the disease, surgery does not provide a 100% guarantee of absolute improvement in vision.
Progress of the operation
Implantation of intrastromal rings and corneal segments into the thickness of the corneal tissue is the most modern and optimal method of treatment for keratoconus. The shape of the rings, which is measured in degrees of circumference, and in addition - their thickness in microns, localization and relative position are strictly individually determined by the shape of the cone, the size and position of its apex.
The operation is performed on an outpatient basis and takes about 20–30 minutes. Anesthesia is performed locally by instillation, which avoids stress on the heart, blood vessels and other internal organs.
Implantation of rings is carried out deep into the thickness of the corneal tissue (stroma), so the thickness of the cornea must be sufficient (at least 400 microns). This operation takes place quickly, on an outpatient basis, with the instillation of an anesthetic drug.
To carry out implantation, a special device can be used - a vacuum layer-by-layer dissector, which creates arcuate tunnels for the rings. In the case of MyoRing, this is a pocket.
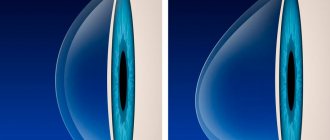
According to the latest technology, a femtosecond laser is used for this purpose, which forms channels or a pocket of the desired size and position.
Patient reviews
Dmitry: I suffered from astigmatism for a long time. Not a single treatment method helped me. Doctors suggested using intrastromal rings. At first I was scared, but I agreed. After installing them, the effect appeared immediately. Two years have passed since then, the disease has not returned.
Alena: I had keratoconus, it took a long time to treat, but it progressed. The ophthalmologist recommended that I get intrastromal rings. Immediately after the operation I felt some discomfort, but it went away quickly. Now I’m fine, there are no sensations in my eyes, the keratoconus is completely gone.
Videos of operations
Video 1. Implantation of corneal segments with femtosecond assistance.
Video 1. Implantation of corneal segments with femtosecond assistance.
Video 2. Installation of the complete Mayoring ring.
The ophthalmic surgeon uses tweezers to place plastic half-rings (segments) into the formed canals. Doctors monitor the patient for some time after the operation, and then he returns home the same day.
The rehabilitation period is minimal (you can return to visual stress the next day), but the patient is required to instill anti-inflammatory and antibacterial drops for two weeks. To ensure a faster recovery, a schedule is drawn up according to which he visits the doctor for a preventive examination.
Preparing for surgery
The following diagnostic tests are performed before surgery:
- laboratory tests to detect abnormalities in the body’s condition and identify infections;
- measuring the degree of impairment, decreased visual acuity, astigmatism, keratoconus;
- consultation with an anesthesiologist to identify the presence of allergies to any components of the medications, selection of an anesthetic drug.
The operation is considered minimally invasive, therefore it is available to almost every patient who has no contraindications.
Stopping the progression of keratoconus
The mechanism by which stromal rings act to arrest keratoconus is not clearly understood, but their action is thought to be a buoyant pressure that is directed outward from the curvature of the cornea. Thus, the apex of the cone is flattened, and the cornea takes on a more natural shape.
According to earlier studies, an important role in this process belongs to the thickening of the overlying epithelium adjacent to the segments, which produces a significant leveling effect.
Results of the operation
In most cases, as a rule, the results of the operation are positive - after surgery, the degree of astigmatism significantly decreases, visual acuity increases (with and without correction with glasses). To date, small groups of patients have been studied, but with follow-up, favorable surgical outcomes are observed within 24–36 months. The best results of keraring were observed in mild and moderate forms of keratoconus.
Fig.4 VisuMax laser for femtosecond support of segment installation
Contraindications and risks of surgery
The operation of intrastromal keratoplasty is very effective and quite safe, but, like any surgical intervention, it has its limitations and contraindications. Among them:
- Age up to 18 years.
- Inflammatory and infectious processes of the eyes.
- Advanced stages of keratoconus.
- Cloudiness of the corneal media.
- Insufficient thickness of the cornea in the central part up to 425 microns.
Among the risks of possible complications of intrastromal keratoplasty surgery, experts name the following:
- Development of an infectious lesion.
- Deterioration of twilight and night vision.
- Displacement of intrastromal segments and their exit to the outside.
- The appearance of halos, glare and fluctuations in visual acuity (in rare cases).
- If surgery is performed on patients with keratoconus, additional visual correction may be required in the future, similar to cases of corneal transplantation. In the case of complex forms of keratoconus, this operation does not provide a guarantee of complete improvement of vision.
Complications after implantation of segments
Complications include perforation of the anterior chamber of the eye during surgery, infection, aseptic keratitis, postoperative extrusion of the stromal ring and lack of the expected effect from the operation. If necessary, problematic segments can be easily removed, which will allow the cornea to return to its original state before surgery. According to studies, removal of stromal rings for any of the above reasons is necessary in approximately 10% of cases. However, this is not an obstacle to subsequently performing layer-by-layer or penetrating keratoplasty.
For what pathologies is treatment with intrastromal rings used?
Intrastromal rings are being created as a treatment option for keratoconus.
El keratoconus This is a condition that occurs when the cornea begins to peel and bulge until it loses its round property and takes on a cone shape.
The arrangement of the rings helps to flatten the convex area that forms the cone to reduce visual impairment caused by keratoconus and ultimately prevent corneal transplantation.
Intrastromal rings may also be indicated to treat refractive errors, especially astigmatism, a condition in which the irregular curvature of the cornea causes images to focus on different points on the retina causing blurred vision of objects at any distance.
Other conditions that can be corrected with an intrastromal ring include postoperative ectasia, radial postkeratotomy ectasia, and postoperative ectasia.keratoplasty or corneal transplant.
Prices for implantation of corneal rings (intrastromal segments)
The cost of the operation consists of the price of the rings themselves (consumables) and the work of the ophthalmic surgeon to directly install them in the operating room.
- Implantation of corneal segments with femto-assistance of the 1st category of complexity - 100,000 rubles.
- Implantation of corneal segments with femto-assistance of category 2 complexity - 130,000 rubles.
The material was prepared by an ophthalmologist: Sagonenko Dmitry Alekseevich
You can ask clarifying questions and make an appointment at our clinic online or by phone in Moscow: Diagnosis and surgical treatment of keratoconus Selection of hard scleral contact lenses.
Intrastromal keratoplasty
Intrastromal keratoplasty is a technique in which special intrastromal segments are implanted into the stroma of the patient's cornea.
They look like two half rings with a triangular cross-section and an arc of 150°-160°. The height of the segments ranges from 150 to 350 microns, the internal diameter is 4 - 6 mm, they are made of medical plastic (polymethyl methacrylate). To implant corneal segments, the patient’s personal data, eye refraction and keratotopography are required. Half rings of the required height are selected strictly individually, because the expected refractive effect directly depends on the height of the implant. The segments are implanted into a special tunnel formed in the middle peripheral zone of the cornea. Such tunnels are usually created using a special surgical knife or femtosecond laser. The use of a femtosecond laser in intrastromal keratoplasty is a fairly new technique that provides the most accurate parameters of the tunnel being formed and minimizes the risk of possible complications associated with mechanically created incisions.