- Age up to 18 years.
- The thickness of the cornea is less than 400 microns.
- Systemic autoimmune diseases.
- Inflammatory processes of the eyes.
- Cicatricial changes in the cornea.
- Periods of pregnancy and lactation.
- Allergic conjunctivitis.
Stages of corneal crosslinking
Technically, the cornea crosslinking operation is carried out in two versions: classical and transepithelial methods.
Classic standard crosslinking is performed with mechanical removal of the surface epithelial layer from the cornea. The advantages of the technique include deep impregnation of the corneal layers with riboflavin, and, consequently, the result of the procedure is higher. Disadvantage: partial clouding of the central zone of the cornea and long-term vision recovery.
The transepithelial method takes place without damaging the cornea. Instillation of the riboflavin solution is carried out directly onto the surface of the cornea. This technique is more gentle and safe, but due to the fact that riboflavin is poorly absorbed through the intact cornea, the effect of the procedure is much less than with the classic version.
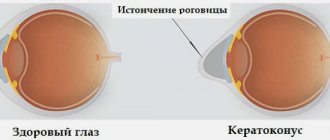
Keratoconus - why is a cone-shaped cornea dangerous for vision?
Keratoconus is a non-inflammatory eye disease in which structural changes occur in the cornea. As a result, it becomes thinner and takes the shape of a cone (normally the cornea is spherical).
The disease is caused by the fact that the fibers that form the structure of the cornea lose their strength properties. Under the influence of intraocular pressure, the organ protrudes. Typically, the characteristic changes in keratoconus affect both eyes. Against the background of pathology, due to uneven refraction of light rays, the acuity of visual function decreases, a person can see objects blurred and distorted. That is, visual impairments characteristic of myopia and astigmatism are observed.
Keratoconus must be treated, otherwise irreversible damage may occur, including complete loss of vision. One of the effective treatment methods is corneal crosslinking.
Indications and contraindications
Keratoconus is the main indication for cross-linking. With this pathology, the spherical part of the cornea of the eye changes and takes on a cone-shaped shape.
The issue of the appearance of keratoconus remains controversial in scientific circles. Recently, ophthalmologists are inclined to the hereditary-metabolic version of the origin of the disease. That is, the possibility of developing keratoconus is inherited, but the disease manifests itself under the influence of provoking factors (endocrine disorders, general diseases, etc.)
The need for treatment is justified by the fact that the deformation of the cornea is progressing all the time, and vision is deteriorating. An important factor is the fact that keratoconus most often develops in young people under the age of 30. If nothing is done, the patient faces loss of vision and disability.
There are other pathologies of the cornea, which are also indications for cross-linking.
List of indications for the procedure:
- Keratectasia after excimer laser refractive surgery (secondary keratoconus).
- Keratomalacia (softening of the cornea of the eye).
- Bullous keratopathy (pathology of the cornea, characterized by tissue swelling and accompanied by pain).
- Corneal marginal degeneration (a rare degenerative disease of the cornea characterized by thinning of the tissue along the edge).
- Ulcerative lesions of the cornea.
- Keratoglobus (hereditary, less commonly acquired disease, in which the anterior part of the cornea protrudes forward, acquiring a semicircular shape).
- Fuchs' dystrophy.
All these pathologies are indications for corneal crosslinking.
The list of contraindications is not long, but there are still circumstances in which cross-linking is not carried out:
- Significant thinning of the cornea (thinner than 400 microns).
- The presence of a large number of scars.
- Age up to 15 years.
- Acute inflammatory processes in the eye.
- Severe mental disorders in the patient (if the mental illness has an undulating course, then in some cases the procedure can be performed when the patient feels satisfactorily).
- Intolerance to local anesthetics.
- Riboflavin (vitamin B2) intolerance.
Not all contraindications are absolute. For example, when a child reaches the age of 15, he can undergo the procedure. Cross-linking can also be performed when the inflammatory process is eliminated.
Corneal collagen crosslinking - what is this operation?
The name “crosslinking” is derived from the corresponding English word cross-linking, which means “crossing connections.” This name reflects the essence of the procedure. During the operation, the ophthalmic surgeon, using special equipment, creates new chemical bonds between the collagen fibers of the cornea, strengthening its structure and increasing its density. A thickened cornea is better able to maintain its shape, which helps stop further protrusion and progression of keratoconus.
Previously, treatment of keratoconus was carried out only surgically - through a cornea transplant. The invention of a new technique made it possible to successfully treat this pathology using a minimally invasive method.
The procedure for strengthening the cornea, cross-linking, allows you to achieve several positive effects at once:
- compacts the base substance;
- slows down or stops the thinning of the cornea;
- stops the progression of pathology;
- improves vision: according to statistics, half of the patients who underwent a similar procedure began to see one line more in the ophthalmological table, 30% of people - two lines more and about 10% - three lines more;
- postpone or completely avoid corneal transplant surgery.
It should be noted that today this procedure is suitable for the treatment of not only keratoconus, but also ulcerative lesions and corneal dystrophy, keratomalacia and other corneal pathologies.
Crosslinking of the eye - the history of the method's creation
Professor Theodor Seiler is considered the creator of the method of treating keratoconus using cross-linking. At the end of the 20th century, he proposed using this method to treat a number of eye diseases, including stopping the progression of keratoconus. Initially, research on the technique was carried out on animals, then on donor cornea, and only after successful experiments the method was tested on patients with cone-shaped corneas.
In the photo: Professor Theodor Seiler
It is worth noting that the first attempts to “glue the fibers together” of the cornea during an oxidation reaction were made even before Professor Seiler’s research. So, in the 90s of the 20th century, a group of researchers tried to glue collagen fibers together under the influence of thermal radiation, different types of waves and enzymes. At the same time, scientists developed a device that could produce UV radiation.
All these studies served as the basis for the creation of one of the most effective and safe methods for treating keratoconus.
How is corneal restoration performed using the crosslinking method?
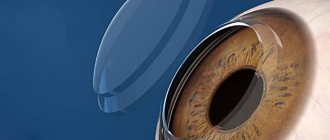
The operation is performed under local anesthesia - eye anesthetic drops are used for this purpose. Today, two cross-linking techniques are widely used in clinics: traditional and transepithelial. Both are carried out in two stages. The first stage of traditional cross-linking involves the complete removal of the upper layer of the cornea mechanically and the application of a vitamin solution of riboflavin. It is necessary in order, on the one hand, to increase the sensitivity of tissues to light, and on the other, to protect the deep layers of the eye from damage by ultraviolet radiation during the procedure. 15 minutes after adding vitamin B2, using a slit lamp, the doctor checks how well the corneal tissue is hydrated with the vitamin solution.
At the first stage of transepithelial cross-linking, the top layer of the cornea is not removed, since the drug that protects the eye tissue penetrates well through the outer layers. For this reason, this surgical technique is considered more gentle and safe for the patient.
The second stage of the procedure in the traditional and transepithelial methods is identical. Using a special UV lamp, the doctor acts on the corneal collagen for half an hour (modern techniques and equipment can reduce this stage to 10 minutes) - cross-linking ensures the gluing of fibers inside the cornea. After the procedure, an antibiotic is dripped into the eyes to prevent possible complications, and the operated cornea is covered with a soft lens. Typically, contact lenses are worn for no more than three days, during which you must continue to use antibacterial drops. Once the lens is removed, your doctor will likely prescribe an anti-inflammatory medication. Usually on the fifth day the superficial layers of the cornea are completely restored. Restoring visual acuity can take up to six months.
Symptoms of keratoconus
Symptoms of keratoconus include:
- split image or multiple images of one object
- image smearing
- the image of the object is visible as if through glass flooded with rain
- nebula image
- photophobia
- vagueness of the text
- eye fatigue
- strong halos from the light source
The insidiousness of keratoconus lies in the non-inflammatory nature of the disease; the development of keratoconus affects vision deterioration with virtually no pain in the eyes.
Testing for keratoconus
A simple test for keratoconus is available at home; to do this, covering one eye, you need to look at a white dot on a black background of a sheet; if you see several images of the dot or its blurriness, you should visit an ophthalmologist. The other eye is checked in the same way. Such a test gives only an approximate result; the best option is a diagnosis of keratoconus by an eye doctor.
Diagnosis of keratoconus
Testing for keratoconus with a keratoconus test or the presence of symptoms cannot definitively diagnose keratoconus, so timely referral to an eye clinic is important.
Diagnosing the disease with keratoconus, depending on the stage, is possible during examination by an ophthalmologist, conducting primary vision diagnostics and additional examination methods using a slit lamp, biomicroscopy, skiascopy, keratotopography, keratopachymetry, computer keratometry.
Treatment of keratoconus
The success and methods of treatment for keratoconus strongly depend on the stage of keratoconus at which the doctor is treated. The following methods are currently used to treat keratoconus.
Treatment methods for keratoconus
The optimal treatment method is determined by the doctor and depends on the stage of development of keratoconus. In the initial stages of keratoconus, conservative treatment is used. Methods of conservative treatment of keratoconus include:
Wearing Contact Lenses - The hardness of contact lenses prevents the progression of corneal deformation in the earliest stages of keratoconus. When treating keratoconus, it is possible to wear combined hard and soft lenses, hydrophilic, and scleral lenses. However, this method does not cure keratoconus, but slows down the rate of its development.
UV crosslinking – currently, corneal collagen crosslinking is one of the modern conservative methods of treating keratoconus. The effectiveness and safety of this treatment is based on the thickening of the cornea under the influence of ultraviolet light on riboflavin.
Surgical treatment of keratoconus is used depending on individual characteristics and in the last stages of development of keratoconus. Surgical treatments for keratoconus include:
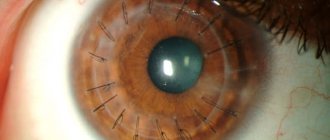
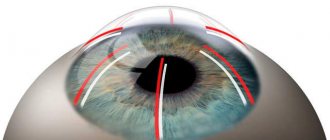
Implantation of stromal rings (segments ) with this method of surgical treatment of keratoconus, hardness is increased due to implants - polymer stromal half-rings. Such segmental ring implants take root and are not visible to the naked eye. After implantation of intrastromal rings, it is necessary to instill anti-inflammatory drops for about a month.
Keratoplasty is a cornea transplant from a donor; keratoplasty can be penetrating or layer-by-layer. Such surgical treatment is highly effective up to 90%, but the process of restoring vision after surgery can be lengthy (up to a year).
Excimer laser surgery for early keratoconus
The prescribed treatment methods for keratoconus depend on the stage of development of the disease.
Stages of keratoconus
The following stages of development of keratoconus are distinguished::
The initial stages of I-II keratoconus are characterized by minor morphological deviations of the cornea with visible nerve endings, also irregular astigmatism and visual acuity of 1.0 - 0.5 for stage I and 0.4 - 0.1 for stage II of keratoconus.
When the disease develops into stage III, clouding of the cornea at the apex of the cone is clearly visible, cracks in Descemet's membrane are observed, and visual acuity decreases to 0.12-0.02.
Cloudiness with thinning of most of the cornea characterizes the course of the disease already in stage IV of keratoconus with a decrease in visual acuity to 0.02-0.01, which without treatment of keratoconus leads to almost complete clouding of the cornea of the eye - transition to stage V of keratoconus.
Acute keratoconus is identified separately. Keratoconus is also classified as primary or secondary and stationary or progressive.
Causes of keratoconus
Despite the advanced age of the disease, the causes of keratotonus have not been identified. One of the main hypotheses for the occurrence of keratoconus is considered to be a failure in the endocrine system and metabolic disorders due to heredity and environmental deterioration in the form of radiation and ultraviolet background.
Contraindications to surgery and possible complications
Corneal crosslinking is performed only at the early stage of keratoconus. In addition to the later stages of the disease, contraindications include the following:
- too thin cornea (less than 400 microns);
- minor age;
- inflammatory diseases and conditions of the visual organs in the acute phase;
- general pathologies affecting the respiratory and cardiovascular systems;
- neuropsychic pathologies.
If surgery is required on two eyes, the procedures are performed at least three months apart.
Sometimes after surgery the patient may experience complications, most often temporary and reversible. So, after the procedure, vision may temporarily decrease or the cornea may become cloudy. In some cases, eye irritation occurs or the process of tissue regeneration is delayed during the recovery period. A serious but extremely rare complication can be corneal melting.
In any case, with keratoconus it is important to make a timely diagnosis and select adequate treatment. Only an ophthalmologist can do this, so do not delay your visit to the clinic.
If a specialist recommends going through the cross-linking procedure, then this method seems to him to be the most effective and appropriate in a particular case. Choose a trusted clinic, reliable specialists, and the likelihood of complications will be minimized.
Possible complications
Corneal crosslinking is considered a safe procedure, as most complications resolve on their own after some time.
Consequences that arise after cross-linking:
- Cloudiness of the cornea, expressed to varying degrees. Most often, vision is not affected. Disappears within six months.
- Eye irritation. Disappears within half a month after the procedure.
- Slow restoration of the epithelial layer, compared with normal values.
- Attachment of infection, reactivation of herpes.
- Melting of the cornea.
- Temporary deterioration in visual acuity (restores after 1-12 months).
The number and severity of complications depend on the general condition of the patient. Those patients who have disorders in the body’s immune system take longer to recover. The consequences can go away within a day, or can persist for up to a year.