Structure of the cornea of the eye
The cornea is the transparent, hemispherical part of the outer shell of the eye. Normally, the cornea is completely transparent. It consists of 5 layers:
- Epithelium is the outer smooth layer. Through it, nutrients are supplied to the deep layers from the tear fluid. The layer regenerates well.
- Bowman's membrane. The most durable layer, but highly permeable to bacteria.
- The stroma is the main substance.
- Descemet's membrane. The shell is easily damaged by mechanical objects, but when exposed to thermal, chemical or bacterial agents it retains its integrity for a long time. When this membrane shrinks, descemetitis occurs.
- The endothelium is the inner layer through which the cornea is nourished from the intraocular fluid.
Layers of the cornea.
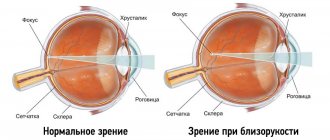
The cornea performs light-conducting and light-refracting functions. If its transparency or sphericity is impaired, a pronounced decrease in vision occurs.
Symptoms
This pathology begins in adolescence and affects both eyes equally.
The course of the disease is very slow, the patient does not notice the development of pathology in the initial stages. The first symptom of keratopathy is a decrease in the sensitivity of the cornea. There are no signs of eye inflammation, that is, no pain or redness is observed. When examining the visual analyzer of a teenager, the ophthalmologist may notice small linear opacities in the central part of the cornea, descemetitis. The epithelium of the cornea is not damaged, vision does not deteriorate. Depending on the form of opacities, the following types of primary keratopathies are distinguished:
- spotted;
- nodular;
- lattice;
- combined.
By the age of 40, opacities grow to the peripheral part. The patient may notice blurred vision and blurred vision. Ophthalmological examination reveals epithelial damage and more severe descemetitis. This is manifested by photophobia, reflexive squinting of the eyelids (blepharospasm).
Prevention
There are no specific preventive measures for keratopathy. The main thing you should do is maintain eye hygiene. If there is significant visual stress, use moisturizing drops, perform special gymnastics (blinking, alternately looking into the distance and at a nearby object, rotating the eyeballs).
Since keratopathy has a different etiology, preventive measures in each case are selected individually, but must be aimed at the causative factor. It is necessary to control the level of cholesterol and calcium in the blood, avoid microtrauma to the eyes, and avoid visual overload.
Keratopathy is a dangerous eye disease that can lead to irreparable consequences. At the first warning symptoms, you should contact an ophthalmologist and undergo an examination.
If you have any questions, contact an ophthalmologist or use the convenient search on our website.
Read more about degenerative changes in the cornea here: https://ofthalm.ru/distrofiya-rogovitsy.html
Treatment
For the treatment of primary dystrophies, regenerating drops and ointments and drugs that improve tissue trophism are used. Taking multivitamin complexes has a certain effect. If there is a significant decrease in visual acuity, plastic surgery (transplantation) of the cornea is performed. An important feature of primary keratopathies is the occurrence of repeated opacities and descemetitis on the donor cornea. In this regard, on average, after 15 years, such patients require re-transplantation of the cornea.
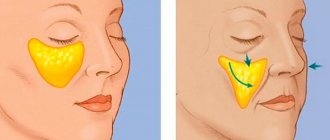
Primary form of edematous keratopathy
Edematous degeneration of the cornea is a special form of primary keratopathies. With this pathology, underdevelopment of the epithelium and endothelium of the cornea occurs. At the initial stages of the disease, the ophthalmologist determines changes in the inner layer. Microscopy reveals the phenomenon of the “drip” cornea. The appearance of such altered cells in the form of “drops” indicates the destruction of the inner layer. As a result, intraocular fluid begins to saturate the cornea, causing it to swell.
Stromal edema leads to a significant decrease in vision. In the later stages, intraocular fluid permeates the anterior epithelium, causing disruption of the integrity of the cornea and exposure of nerve endings. The patient develops a pronounced corneal syndrome: photophobia, blepharospasm, pain, and lacrimation appear.
Treatment of the edematous form of degeneration in the initial stages consists of the use of decongestants and drugs that improve trophism. When pathology affects the anterior epithelium, it is necessary to use protective therapeutic contact lenses, ointments based on vitamin A, and regenerating ointments. Therapeutic contact lenses and ointment-based preparations help protect the highly sensitive nerve endings of the cornea from the traumatic effects of the environment.
A radical treatment method is corneal transplantation. Laser stimulation is used among physiotherapeutic methods.
Central toxic keratopathy
Central toxic keratopathy (CTK) is a rare, acute, non-infectious condition characterized by clouding and thinning of the corneal stroma in the laser-treated area (following refractive surgery). A similar complication occurs in 0.0076–0.016% of cases with the development of the main clinical manifestations on days 3–9 after surgery.
With biomicroscopy, fine-grained infiltration of the interface is observed, as in diffuse lamellar keratitis (DLK) stage II and striae. The opacification is usually central and extends posteriorly into the corneal stroma. The hypermetropic shift (2 diopters or more) is determined by refraction.
The causes of this condition remain unknown. According to confocal microscopy, apoptosis of keratocytes in the laser irradiation zone with their gradual restoration is determined. There are suggestions that such a reaction may be due to photoactivation after laser exposure to certain substances from tears that trigger apoptosis. It has been shown that the method of flap creation does not affect the development of TKA, as cases of this complication have been described after PRK and FemtoLASIK. Among the causes of TCA, the pathology of the eyelid margin is also considered, indicating the possible influence of the secretion of the meibomian glands, a large number of bacteria from the edge of the eyelid, proteolytic enzymes and inflammatory cells.
The issue of prescribing corticosteroids in the treatment of TCA is also discussed in the literature. Due to the fact that the number of patients with this pathology is very small, no randomized studies have been conducted that would clearly define management tactics, but all researchers indicate a favorable course of this condition with resorption of opacities after 2-18 months. Some researchers agree that recovery occurs gradually without any treatment, and such patients only need careful monitoring.
Although, if we take into account that the development of central toxic keratopathy is preceded by DLK, then the use of steroids in the first few weeks after surgery is absolutely justified. Long-term courses of topical steroids are not recommended because TCA is a non-inflammatory disease and additional complications due to side effects (eg, glaucoma or cataracts) may occur.
Another pharmacological approach is to use vitamin E to inhibit apoptosis by blocking the proinflammatory cytokine cascade. it can also be supplemented with vitamin A, well known for its antioxidant and reparative properties.
Secondary dystrophies
Secondary dystrophies include degeneration of the cornea of the eye resulting from any disease of the visual analyzer. These include bullous and band keratopathy.
Read in a separate article: Corneal dystrophy: types and methods of treatment
Bullous dystrophy
Bullous or epithelial endothelial dystrophy (EDD) occurs after trauma to the cornea, burn or surgical treatment. In this case, degeneration can occur both as a result of surgical treatment itself, and as a result of periodic contact of the posterior layers of the cornea with the supporting elements of the intraocular lens (after cataract extraction).
In EED, local damage to the endothelium occurs as a result of trauma. Through the resulting defect, aqueous humor penetrates into the surface layers, causing swelling and thickening of the cornea. If the damage is in the periphery, vision loss does not occur. Corneal syndrome (blepharospasm, pain, lacrimation, photophobia) occurs in advanced stages, when swelling reaches the surface layer and becomes visible to the naked eye. Blisters (bullas) form on the epithelium; when they burst, the nerve endings of the cornea are exposed.
A distinctive feature of EED is the possibility of complete recovery. Treatment of bullous keratopathy is similar to the treatment of the edematous form of primary degeneration. If corneal keratopathy occurs after cataract surgery, repeated surgery is required to fix the intraocular lens. Donor corneal transplantation is rarely used as a treatment for bullous keratopathy.
Band keratopathy
This type of corneal atrophy occurs in blind eyes. With prolonged loss of vision (most often as a result of injury or glaucoma), a violation of the trophism of the eyeball develops, hypotonia of the extraocular muscles, and the composition of the intraocular fluid changes. Years after vision loss, atrophy of the cornea (its superficial layers) begins. A horizontal visible clouding is detected on the cornea, and the cornea itself becomes rough. The turbidity grows from the periphery to the central part.
Blind eyes with corneal atrophy are subject to removal and subsequent prosthetics.
Symptoms of the disease
A disease of the cornea, accompanied by swelling and the appearance of bubbles (so-called bullae) on the epithelial layer, is called bullous keratopathy. The main symptoms are manifested precisely by external changes in the structure and shape of the cornea, but, in addition to this, the disease is often accompanied by other signs:
- acute, unbearable pain in the eyeballs;
- decreased clarity of vision;
- foreign body sensation;
- a feeling that “sand” has been poured into the eyes;
- severe lacrimation;
- intolerance to bright light.
The onset of the disease is often characterized by photophobia and slight discomfort in the visual area. In the next stage, the conjunctival membrane becomes inflamed and the eyes appear red. Patients often complain that their vision has become worse. By the third stage, the severity of all symptoms increases, and additionally, stabbing pain in the eyes occurs. At the next stage, the pain syndrome is already so strong that it affects other areas of the head. Vision is very blurred, the person sees worse and worse. The last stage is characterized by partial or complete loss of vision and deformation of the eyeball.
Surgical treatment of pathology
The only radical treatment for corneal degeneration is surgery. Depending on the type of dystrophy, keratoplasty and keratoprosthesis can be performed.
Keratoplasty
Keratoplasty is a corneal transplant. It can be layer-by-layer and end-to-end. Layer keratoplasty is used when atrophy of the cornea of the eye affects only the superficial layers. The operation is performed under local anesthesia. The surgeon removes the clouded surface layers of the cornea, and installs a donor graft in place of the resulting defect. Corneas from cadaveric eyes are used as donor material. The graft is secured with interrupted sutures.
Penetrating keratoplasty can be performed under either local or general anesthesia. All layers of the cornea are completely removed. Donor tissue is transplanted in their place. The danger is the loss of the lens and other structures of the eyeball into the wound.
The success of the operation depends on the engraftment of the graft. Since there are no blood vessels in the cornea, the donor and recipient may not match in blood type and Rh factor. With lamellar keratoplasty, engraftment usually goes well, graft rejection reactions are rare.
The prognosis of penetrating keratoplasty depends on the preservation of the posterior endothelium of the donor cornea.
Keratoprosthetics
If keratoplasty is not possible, keratoprosthesis is performed. Instead of a donor cornea, a plastic keratoprosthesis is installed at the site of the defect. The operation is carried out in two stages. At the first stage, the prosthesis attachments are placed between the layers of the corneal cataract. After they have fused with their own tissues (usually within a month), the second stage is performed - removal of the cataract. Complete restoration of vision does not occur as a result of keratoprosthesis; keratoplasty is preferable.
Causes
It is possible to find out the cause of the development of the disease only after its type is determined. Why is this diagnosis most often made:
- Surgical intervention in the treatment of cataracts, glaucoma and other serious diseases.
- Congenital pathology in the presence of a similar problem in one or both parents.
- Trauma can stimulate the development of the band-like form.
- Also, a ribbon-like form with calcium deposits develops against the background of the development of viral diseases. For example, as lupus progresses, the cornea may become damaged.
- Influence of climatic conditions.
- Conjunctivitis, dry eye syndrome, entropion and blepharitis can eventually cause the development of a superficial pinpoint form of the problem.
The development of the disease can be affected by constant exposure to bright light or foreign objects entering the eye. Each case is examined separately, and the diagnosis directly depends on the overall clinical picture.
It was mentioned above that the aphakic form of keratopathy develops against the background of natural changes in the ocular apparatus with age. In general, the patient’s age, gender and developmental characteristics cannot be discounted, since all these important nuances can prompt the correct diagnosis.
Stages of development of the bullous form
Find out how Iridina moisturizing eye drops work here.