Tumors of the conjunctiva
| Benign | Intermediate | Malignant |
| Coming from the epithelium | ||
|
|
|
| Originating from subepithelial layers | ||
| — | — |
Polyp
Usually occurs due to improper treatment of chalazion or meibomitis. It looks like a fleshy formation with a wide or narrow base. Treatment is surgical. True papillomas are rare. In children they are represented by red-pink nodules on a thin stalk, in adults - by keratinizing outgrowths localized near the limbus.
Krause's gland cyst
It is localized in the conjunctival fornix, most often the lower one. Can reach large sizes, the contents are transparent. Treatment is surgical (puncture of the cyst wall).
Nevus stationary
Often found in children. Makes up ~20% of all benign neoplasms of the conjunctiva. It is predominantly localized at the edge of the cornea (at the level of the open palpebral fissure), in the area of the lacrimal caruncle and the semilunar fold. It has a yellow-brown color, a well-developed vascular network and a smooth surface. In almost 30% of cases, nevi are devoid of pigment.
Progressive nevus
Signs: increase in size, increased pigmentation, blurred boundaries, expansion and increase in the number of blood vessels. Surgical treatment is excision of the nevus.
Dermoid (lipodermoid)
Accounts for ~20% of all benign conjunctival tumors in children. The congenital formation is yellowish in color, elastic in consistency, sometimes bilateral. It is usually located at the outer or lower outer edge of the cornea, but often grows into its deeper layers. This part of the dermoid already has a smooth, shiny white surface. Treatment is surgical.
Hemangioma
Congenital vascular tumor. The most common capillary hemangioma is localized in the inner corner of the palpebral fissure. Usually, convoluted bluish-colored vessels are clearly visible. Treatment: submersible electrocoagulation.
Lymphangioma
A rare tumor localized in the conjunctiva of the eyeball or its fornix. It consists of dilated thin-walled channels with endothelial coating, filled with serous fluid mixed with red blood cells. Externally, the tumor looks like a translucent, finely lobulated thickening of the conjunctiva. Treatment: surgical or radiation (brachytherapy using a strontium applicator).
Epithelioma of Bowen (Bowen J. T., 1912). A tumor that usually develops in mature people in the epithelium of the limbal part of the conjunctiva of the eyeball. It looks like a flat or raised cellular structure with clear boundaries. Tends to spread to the cornea, but never invades its Bowman's plate. Treatment is surgical (with preliminary treatment of the tumor and then the surgical wound with a 0.04% mitomycin C solution).
Primary acquired melanosis
The tumor occurs in middle-aged people. It can be localized in any part of the conjunctiva of the eyelids and eyeball, and also spread to the cornea. It looks like flat spots of dark color with clear boundaries. Treatment: cryodestruction, laser coagulation or electroexcision of the tumor with preliminary application of a 0.04% solution of mitomycin C.
Squamous cell carcinoma
A rare tumor in older people. It can develop in any part of the conjunctiva. It grows slowly, but is prone to germinating into deeper tissues and into the eye cavity. Usually has the appearance of a pinkish papillomatous node. Treatment: excision of the tumor in combination with cryodestruction or laser coagulation, radiation therapy.
Melanoma
Develops in mature people from primary acquired melanosis (~ 75% of cases), previous nevi (20%) and as a primary pathology (5%). It is usually localized on the conjunctiva of the eyeball and quickly grows along its surface, including in the form of a node. Surrounded by a network of dilated and full-blooded vessels. It can be pigmented or non-pigmented. Slit-lamp examination using a blue light filter helps to identify scattered pigments extending in the form of “paths” from the visible boundaries of the tumor. Later, macroscopic screenings may appear around the tumor node. The prognosis for the patient is unfavorable. Treatment: local excision of the tumor in combination with radiation brachytherapy, removal of the tumor en bloc with surrounding healthy tissue in combination with chemotherapy, irradiation of the affected area with a narrow medical proton beam.
Choroidal hemangioma
- Clinical picture
- Diagnostics
- Treatment
Choroidal hemangioma is a rare congenital benign tumor with torpid growth, often leading to retinal detachment, and therefore requires dynamic monitoring and OCT monitoring of the condition of the retina, the level of detachment, and tumor thickness. The rationale for prescribing treatment should be considered to be a progressive decrease in vision and an increase in retinal detachment.
Occurs with a frequency of 1 case in 15 malignant melanomas of the choroid. Among eyes removed due to intraocular tumors, it is 0.76%. The age of patients is 10-60 years. The diagnosis of cavernous hemangioma is difficult. Clinical and histological discrepancies reach 18.5%.
Clinical picture
Complaints of decreased vision are an early symptom of hemangioma in adults, and strabismus in children. Visual disturbances in WHC are characterized by a hypermetropic shift without changes in the overlying retina, or gradual blurring of vision, or sudden loss of vision, which is associated with secondary changes in the retina.
In the choroid, hemangioma is represented by two clinical forms.
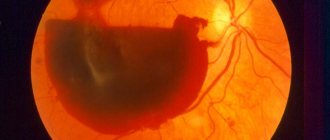
- A limited hemangioma is represented by a single node with clear boundaries, round or oval in shape, the maximum diameter of the tumor is 3-15 mm. The thickness of the tumor is 1-6 mm. The color of the tumor is often light, the color ranges from whitish-gray to pink-red. In a third of cases, the tumor has a dark red color with a slate tint, which is caused by proliferation of the RPE. Secondary retinal detachment is observed in almost all patients; with large, long-standing tumors, it becomes vesicular. The caliber of retinal vessels, unlike choroidal melanoma, does not change; there may be small hemorrhages on the surface of the tumor. With mild subretinal exudate, cystic degeneration of the retina creates a picture of the “openwork” of the tumor. Subretinal exudate can sometimes be significantly thicker than the thickness of the tumor itself. Cases of ossification of hemangiomas have been described.
- Diffuse hemangioma is often combined with Sturge-Weber syndrome (encephalofacial angiomatosis). Characteristic features are red-orange staining of the entire surface of the fundus to the equator, retinal detachment with secondary dystrophic changes, diffuse thickening of the choroid detected by ultrasound, and a bright red glow of the pupil on the affected side.
Diagnostics
The tumor can be detected during a routine fundus examination. Complaints of decreased visual acuity appear with the development of the most common complication - serous macular retinal detachment.
Ophthalmoscopically, a red-orange formation is determined, most often located near the optic nerve head, less often - at a distance from it, in the region of the posterior pole of the eye.
Typical for hemangioma is its transillumination or the “Japanese lantern” phenomenon - the glow of the tumor mass when its edge is illuminated using a slit lamp or an indirect ophthalmoscope. The edges of the tumor are usually indistinct. Serous retinal detachment and lipid exudates can be detected in the fundus.
Fluorescein angiograms It increases unevenly. In the late phase of angiography, fluorescein staining of tumor tissue without diffusion of the dye is determined. In the center of the hyperfluorescent zone there are small foci of hypofluorescence, the presence of which is associated with pigment migrations and the screening effect that they produce.
Angiography can clarify the area of concomitant serous retinal detachment. Angiography with indocyanine gives a characteristic picture of hemangioma - the early appearance of high-intensity hyperfluorescence, starting from the first minute of the study. Hyperfluorescence in this case is homogeneous. It weakens from the 3rd minute of the study and in the late phase is replaced by hypofluorescence of the tumor in combination with hyperfluorescence of the zone of serous retinal detachment.
Echography-B reveals the formation of hyperechoic density, giving rise to thickening of the choroid. There is no choroidal excavation in the projection of the neoplasm.
Differential diagnosis: it is necessary to exclude apigmented and weakly pigmented choroidal melanoma, metastatic cancer, posterior scleritis, serous chorioretinopathy, disciform macular degeneration, central serous retinopathy and rhegmatogenous retinal detachment, and in young people - retinoblastoma.
Choroidal metastases are usually multiple. Choroidal osteoma is usually flat and heavily calcified, giving the characteristic cone-shaped echo pattern of this tumor.
Treatment
Tumor elimination is necessary to prevent total retinal detachment.
Photocoagulation does not lead to tumor regression, but can significantly reduce the severity of exudative retinal detachment. It is carried out with separated coagulates with a size of 500 microns, an exposure time of 0.5-1.0 seconds at medium power. Recurrence of serous retinal detachment occurs in 40% of cases.
Radiation therapy is the treatment of choice for choroidal hemangiomas. It can be carried out with cobalt plates, external irradiation with electrons or protons. Typically a dose of 20-30 Gy is used in 4-5 sessions.
Evolution and forecast:
Hemangiomas are benign neoplasms with slow growth. Their main complication is associated with exudative retinal detachment, which can cause irreversible changes in the macula.
Diagnosis of ocular hemangioma
When the formation affects the eyelids or eyeball, diagnosis is not difficult. To begin, the ophthalmologist performs a visual examination of the hemangioma using a slit lamp. The patient is then sent for additional examinations, which include an ultrasound examination of the eyeball, showing the consistency and depth of the growth, and computed tomography of the eye orbit. Sometimes they resort to magnetic resonance imaging when the results of ultrasound are not enough. MRI allows you to accurately determine the size of the ocular hemangioma and determine whether nearby tissues are damaged.
If the doctor decides to treat the formation through surgery, the patient is sent for angiography in order to thoroughly determine the edges of the hemangioma. When the formation changes shape, color, increases in size or bleeds, a biopsy is used to determine the nature of the growth (malignant or benign). In addition, sometimes the patient is additionally sent to a dermatologist, oncologist and infectious disease specialist.
Causes
Local or systemic diseases can lead to the formation of conjunctival edema. Often the nature of chemosis is endocrine or allergic.
Local causes of swelling include:
- Inflammatory processes affecting the conjunctiva (gonoblenorrhea, conjunctivitis), as well as the adjacent area (phlegmon of the orbit, barley, panophthalmitis);
- Stagnation;
- Swelling of the eyelid tissue;
- Instillation of certain medications;
- Retrobulbar neoplasms.
Chemosis can affect the entire conjunctiva or occur only in a limited area.
In case of inflammation, pus and bacteria can accumulate under the edematous layer of the mucous membrane. As a result, the surface of the cornea becomes ulcerated.
With panophthalmitis or retrobulbar neoplasm, chemosis also often occurs. This is due to stagnation. In some cases, the cause of edema is malignant exophthalmos.
If the formation of chemosis is associated with a complication of lower blepharoplasty, then it is accompanied by swelling of the bulbar conjunctiva. In this case, the swelling goes away without additional intervention within a month and a half.
Diagnostics
Diagnosing hemangioma is not difficult; to do this, you only need to correctly assess the appearance of the neoplasm. To accurately determine the type of pathology, there are various manuals, which consist of numerous images of various forms of tumor processes in the eye.
Thanks to such reference books, it is possible to accurately determine the nature of the growths present and the location of the lesion.
When diagnosing an eye hemangioma, the child must be registered at the dispensary, since the doctor must monitor the course of the disease. Adequate treatment is also determined, which can be either conservative or surgical.
Medical practice sometimes encounters difficult cases when the lesion is localized in the deep layers of the orbit. In such situations, a visual examination does not make it possible to make an accurate diagnosis, so the specialist prescribes the following additional measures:
- X-ray of the eye.
- CT scan.
- Arteriography.
- Venography.
On this topic
- Organs of vision
All about ocular sarcoidosis
- Natalya Gennadievna Butsyk
- September 3, 2021
Arteriography and venography make it possible to assess the condition of blood vessels.
During the examination, visual acuity is assessed, the presence of strabismus is determined, as well as the presence of other concomitant diseases. Only after carrying out such measures can the doctor determine the most suitable treatment.
In the presence of superficial lesions that do not affect visual acuity, special therapy is not prescribed, but the child should be constantly monitored by a doctor in order to monitor the progression of the pathology.
More often (in 70% of cases), by the age of 7-8 years of life, the neoplasms disappear on their own; in other situations, the use of steroid medications is required or cosmetic surgery is prescribed.
If the presence of the disease negatively affects visual acuity, then removal of the lesion is required. To eliminate the tumor, laser treatment or liquid nitrogen can be used.
The measure of influence is selected depending on the age category of the patient. Often, after removal of the lesion, the doctor prescribes hormonal medications or radiation exposure (prescribed only as a last resort).
Reasons for appearance
The reasons why hemangioma appears on the eyelid or conjunctiva are not fully understood. Since the formation often occurs in infants, doctors agree that it is caused by disorders of the cells of the vascular wall. Such processes are observed starting from the 7th week of pregnancy. Based on the fact that the process of vascular development in the fetus has not been fully studied, doctors cannot accurately determine the factors that influence the appearance of hemangioma. However, any disturbances in the process of formation of blood vessels can contribute to their excessive growth, which provokes the formation of hemangioma of the choroid and conjunctiva.
Treatment
Diagnosis of eye hemangioma is not difficult, but the specialist must take into account that the tumor may be predisposed to rapid growth.
For this reason, even the smallest hemangioma requires an examination by an ophthalmologist, who will determine the need for treatment and will be able to prescribe the most appropriate therapeutic measures in each individual case.
If the tumor does not interfere with the small patient, then treatment is not prescribed during the first few months. As the process progresses, the question of removing the tumor is raised, since the risk of complications increases.
Several effective measures have been identified:
- Ligation – when the lesion grows, the specialist ligates the vessel that feeds the tumor. In this case, a rapid decrease in the size of the formation is observed.
- Peeling is carried out using ethyl alcohol, and a decrease in size is also observed.
- Hormonal therapy is indicated for small lesions.
- Electrocoagulation - a similar measure is characterized by the effect of a small current on the affected area. It can be prescribed as a primary or additional measure of therapy.
- Exposure to a laser beam is prescribed when the formation is localized close to the eyeball.
- Cryodestruction is the use of liquid nitrogen to freeze the affected area. As a result of the procedure, a crust appears, which subsequently disappears on its own, and healthy skin forms in its place.
- Surgical intervention is prescribed only if other measures are impossible or ineffective. After removal, a scar remains on the eyelid.
The prescription of effective measures depends on the patient’s age, the size and growth rate of the tumor, and general health.