The inflammatory process in the retina of the eye is called retinitis. It is not uncommon for inflammation of the retina to be combined with inflammation of the choroid (choroid). In this case, the disease is called chorioretinitis or retinochoiditis. The localization of the inflammatory process can be in various areas of the retina: in its center, around the vessels, and it can also spread widely. As a result of the pathological process, the elements of the retina are destroyed in the area of the inflammatory focus (the affected area) up to the development of tissue necrosis, and lymphocytic infiltration develops with the formation of scar tissue. This causes vision deterioration, which is not always possible to restore even after treatment. Patients often experience hemorrhage in the tissues of the retina and choroid.
Reasons for the development of the disease
Typically, inflammation of the retina develops as a result of endogenous or exogenous infection. Exogenous infection occurs as a result of injuries or burns to the eye, and endogenous infection penetrates through the blood vessels.
Retinitis is classified based on the development of pathology.
Endogenous retinitis includes:
- developing against the background of infectious diseases: syphilis, tuberculosis, toxoplasmosis, sepsis, etc.;
- caused by pathologies of the circulatory system or metabolic disorders: leukemia, diabetes, etc.;
- resulting from a viral infection: cytomegalovirus infection (CMV), herpes, influenza, lichen, measles, etc.;
- having an unclear etiology (exudative and shingles);
- hereditary genesis - this includes all types of retinitis pigmentosa, which are sometimes classified as retinopathy and degenerative processes of the retina.
Exogenous retinitis includes:
- traumatic,
- postoperative,
- solar, etc.
Often, retinitis is diagnosed as a concomitant disease caused by one of the above pathological processes. Treatment in such cases should be carried out in both directions.
Classification of retinitis
The main classification of pathology is divided into endogenous and exogenous retinitis. Each of them has certain types of manifestation. The following endogenous forms of the disease are divided:
- against the background of severe infectious diseases: tuberculosis, syphilis, toxoplasma, brucellosis, sepsis;
- retinitis, which occurs due to metabolic disorders and blood diseases: diabetes, leukemia;
- exudative, herpes zoster retinitis of unknown etiology;
- hereditary retinitis pigmentosa and its forms (in ophthalmology this type is defined as retinal degeneration).
Exogenous species are divided into: solar, traumatic. They can also be identified by location. There are widespread, localized and disseminated retinitis. Inflammation affects the destruction of the retina and choroid. Scar tissue may form at the site of infection
Retinitis is accompanied by destruction of the nerve elements of the retina. The vascular reaction leads to the manifestation of vasculitis. There may be blockage of blood vessels and severe hemorrhages.
Symptoms of retinitis
The inflammatory process in the retina is not accompanied by pain, so patients usually complain of disturbances in the quality of visual function:
- visual acuity decreases;
- defects in the visual field are observed: some areas may fall out, and “tunnel vision” may occur;
- in rare cases, color perception is impaired;
- vision adaptation decreases in the dark (“night blindness”);
- photopsia appears - the appearance of light phenomena before the eyes: lightning, flashes and sparks;
- metamorphopsia occurs - distortion or blurriness of images of objects.
With further progression of the pathology, extensive chorioretinal scars are formed, persistent deterioration of vision continues, hemorrhages in the vitreous body and retina may occur, there is a risk of retinal detachment and the development of optic nerve atrophy. In addition, the possibility of an inflammatory process in other eye tissues poses a danger. Inattention to the manifestations of the disease is fraught with very serious consequences.
Toxoplasmosis retinitis
Toxoplasmosis retinitis (chorioretinitis) occupies a significant place among inflammatory lesions of the fundus. Toxoplasmosis R. is divided into congenital and acquired.
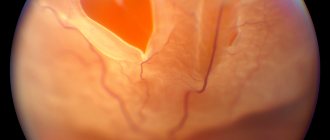
Congenital toxoplasmosis R. occurs as bilateral chorioretinitis and is detected against the background of hydrocephalus (see) or microcephaly (see). X-ray reveals intracranial calcifications. Usually this disease is diagnosed in the absence of inflammatory phenomena, when cicatricial changes are found in the fundus of the eye that developed after intrauterine chorioretinitis (see color table to the article Fundus, Fig. 55). Scar changes in shape may resemble macular coloboma (pseudocoloboma).
Acquired toxoplasmosis R. is diverse in its forms of manifestation. Along with exudative and proliferating chorioretinitis, there are iridocyclitis (see), episcleritis (see Scleritis).
The classic picture of toxoplasmosis R. is the formation of a central fresh, round-shaped, loose focus of gray-yellow and greenish-yellow color, surrounded by perifocal edema and often hemorrhages (color. Fig. 2). Old toxoplasmosis lesions are cicatricial or atrophic foci, sometimes with the formation of a subretinal neovascular membrane (tsvetn. Fig. 3). Vitreous opacification with the presence of inflammatory cells is often observed.
When the lesion is localized near the optic nerve head (in the peripapillary zone), a picture of neuroretinitis appears. Sometimes the process has a picture of disseminated chorioretinitis. With significant exudation, exudative retinal detachment may develop.
Treatment is complex and must be coordinated with therapists and doctors of other specialties; includes specific therapy (see Toxoplasmosis), sulfonamides, vasodilators and agents that increase retinal metabolism.
The prognosis is serious.
Prevention consists of active identification of patients with toxoplasmosis and their timely treatment.
Leprosy retinitis
Leprosy retinitis is rare, mainly in the lepromatous type of leprosy (see) and is associated with infiltration of the tissues of the eyeball by mycobacteria of leprosy. When the choroid itself is involved in the process in the fundus of the eye, round, yellow nodules resembling a pearl appear closer to the periphery. These changes are not always observable, because in most cases they are combined with iridocyclitis (see Iridocyclitis) and posterior synechiae (adhesions between the iris and the lens), making it difficult to dilate the pupil.
Treatment necessarily includes specific therapy.
The prognosis is serious.
In the prevention of leprosy R., identification and treatment of patients at the earliest possible time is of great importance.
Metastatic (septic) retinitis
Metastatic (septic) retinitis is characterized by signs of intraocular infection associated with hron. recurrent diseases of various organs (heart, kidneys, liver, brain, etc.). Eye damage in these diseases is observed in approximately 50% of cases. The causative agent of the infection is most often streptococcus (Streptococcus viridans). Changes in the retina occur in the form of flame-shaped hemorrhages resembling Roth spots (see Retinopathy), white lesions located under the retinal vessels, edema of the retina and optic nerve head.
Treatment is carried out jointly with therapists and doctors of other specialties. Anti-inflammatory therapy is indicated, including local and general use of antibiotics and corticosteroids. Antispasmodics and drugs that increase retinal metabolism are also used.
The prognosis is serious.
Prevention consists of the earliest possible detection and timely treatment of the underlying disease.
Diagnostics
Diagnosis of retinal inflammation occurs using various ophthalmological tests. It includes the use of visometry, computer perimetry, color testing, determination of visual fields, ophthalmoscopy, fundus biomicroscopy and X-ray examination: fluorescein angiography and optical coherence tomography. Carrying out these procedures makes it possible to detect pathology and classify it, and to make the clinical picture more complete, a blood test is performed. Identifying the exact cause of retinitis allows you to prescribe the most appropriate treatment.
Signs of retinitis
The degree of manifestation of this unpleasant disease depends on the area of the lesion, as well as on the location of inflammatory foci on the retina. One of the symptoms is a sharp decrease in central or peripheral vision, depending on where the damage is located. However, visibility may decrease in low light conditions. Color perception may also change. But retinitis doesn't always present this way. For a long time, the process can proceed unnoticed by the patient in mild stages. Since there are no nerve endings in the retina, a person does not feel pain signals.
With severe degrees of the disease, blood vessels can be destroyed, which can cause hemorrhage in the retina or vitreous body (hemophthalmos). If retinitis is started, the process can spread to other tissues and cause inflammation of all the membranes, which will lead to irreparable damage to the eye. That is why, in case of any unpleasant sensations, it is necessary to urgently diagnose the visual organs. The eyes are a fragile instrument given to us by nature and we need to be careful about their health. After all, it is impossible to restore lost vision.
Treatment of retinitis
Depending on the diagnostic results, antiviral or anti-inflammatory drugs are used for treatment: antibiotics, topical ointments and drops with corticosteroids. In cases of specific retinitis that occurs against the background of a general somatic disease, therapy is selected in accordance with the general picture of treatment. Often, antispasmodics and vasodilators, vitamins and agents to improve metabolism are also prescribed. Treatment of retinitis is usually carried out in a hospital setting.
Unfortunately, with inflammation of the retina, it is not possible to avoid significant deterioration in vision and achieve complete restoration of visual function even with adequate treatment. That is why it is important to follow measures to prevent complications in general somatic diseases, infectious and viral pathologies, as well as avoid injuries and burns in order to prevent such a dangerous disease as retinitis of the retina.
Treatment
The first step is to eliminate the root cause. A progressive infectious disease will not completely cure retinitis. To eliminate the root cause, doctors of related specialties are involved.
The main treatment is therapy for the disease. If the cause of the pathology is an infection, then antibacterial medications are prescribed for treatment. Anti-inflammatory drops are used in combination with antibiotics intramuscularly. It is possible to use antibiotics for internal use. For treatment, steroid drops are selected to relieve inflammation.
To improve blood supply to the retina, treatment is prescribed in the form of injections with vitamin or vascular preparations. Moreover, if the patient has recently appeared hemorrhages during examination, then vascular drugs are contraindicated. Treatment is carried out in the form of injections intramuscularly or in the area near the eyes.
Laser coagulation is performed if retinal detachment has occurred. The sooner the disease is diagnosed and the procedure is performed, the more likely it is that the patient’s vision will be preserved. In case of a large area of the retina or the impossibility of laser coagulation, surgical intervention is performed. During the operation, the vitreous is removed and a bandage is installed.
Manifestations
Retinitis in typical cases is characterized by the following symptoms:
- Rapidly progressive decrease in visual acuity;
- The appearance of fog and veils before the eyes;
- Floating spots and dots;
- Flickering of objects;
- Distortion of their contours;
- Flashes of light before the eyes;
- Dropping fields of view.
In addition to hereditary and congenital cases, these symptoms are associated with certain factors that increase the likelihood of developing retinitis. These are chronic infections in the body, rheumatological diseases (hemorrhagic vasculitis, rheumatoid arthritis) and previous operations on the organ of vision.
Coates' retinitis
Coates' retinitis is a congenital, but not hereditary, disease. It is characterized by unilateral damage to the retina due to the irregular course of the vessels behind it. With this pathology, blindness and glaucoma (a condition with increased intraocular pressure) often develop.
If such retinitis is present, its symptoms are quite specific. First of all, the doctor identifies during ophthalmoscopy a sign such as leukorrhea - a white glow of the retina. In addition, the person is bothered by blurred vision, flashes of light and emerging colored patterns (these are associated with detachment of the retina).
When photographing with a flash, almost all patients have a “yellow eye” in the image. This color is associated with the reflection of light rays from dilated vessels that contain cholesterol plaques. If the child’s eyes in the photo are yellow, then you should immediately contact an ophthalmologist. You will be helped and seen at a convenient time at NEARMEDIC centers.
Retinitis of the eye - what is it?
Retinitis
or inflammation of the retina can occur due to various infectious diseases or as a toxic-allergic reaction. The retina is a very thin, less than one-third of a millimeter (300 microns) thick, light-sensitive tissue. It provides the basic functions of the visual organs - central and peripheral (lateral) vision. Treatment of retinitis depends on the causes of its occurrence and is most often inpatient.
Retinitis of the eye is an inflammatory disease of the retina, which can be either unilateral or bilateral.
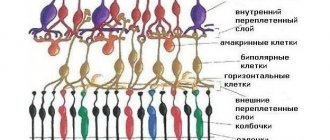
The retina is a thin layer of the eye, about one-third of a millimeter thick. It contains photoreceptors (rods and cones) responsible for central and peripheral vision. In retinitis, damage to the retina usually begins in small areas but then grows and leads to noticeable deterioration of vision.
Cytomegalovirus retinitis
CMV retinitis is an inflammatory lesion of the retina caused by cytomegalovirus. Most often occurs in people with weakened immune systems, incl. against the background of HIV infection. Typically acute or gradual loss of vision. At the same time, blurred contours of the objects in question appear, flies flickering before the eyes and the presence of floating spots. Cytomegalovirus is characterized by sequential involvement of one and then the other eye.
Retinitis of different nature is clinically similar to each other, so it is difficult to distinguish them. But there are certain features that are very rarely encountered with cytomegalovirus infection. So, it is not typical for her to experience pain and a burning sensation in the eye, increased tearing and irritation of the conjunctival membrane.