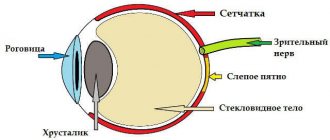
Angiopathy is a pathological change in blood vessels caused by a disorder of nervous regulation. Retinal vascular angiopathy is not an independent disease. This is just one of the manifestations of some pathological conditions complicated by damage to the body’s blood vessels, including the vessels of the retina. Retinal vascular angiopathy equally often affects both men and women. It also occurs in children, but most often it is diagnosed in people over 30 years of age. Today, experts pay maximum attention to this disorder, because it often causes irreversible changes in vision function, up to complete blindness.
Retinal angiopathy - what is it?
The term “angiopathy” consists of two words: “angio” - vessel and “pathy” - disease. With angiopathy, for some reason the normal functioning of its vessels is disrupted. In this case, the retina does not receive enough blood supply due to impaired function of the fundus vessels.
Angiopathy is not an independent diagnosis, but a consequence of other pathologies.
With retinal angiopathy, the blood supply to the arteries and veins of the posterior wall of the eyeball changes, which leads to progressive visual impairment.
Causes
Any angiopathy appears as a result of any long-term malfunction in the body. Most often, this pathology is observed in patients whose health is impaired due to:
- pressure disorders (arterial hypertension, dystonia or hypotension);
- increased intracranial pressure of various origins (congenital pathology, in old age, due to diseases);
- systemic vasculitis;
- juvenile angiopathy (Eales disease);
- diabetes mellitus;
- vascular atherosclerosis;
- arteritis (usually in the head area);
- glaucoma;
- injuries (usually head, neck, face);
- perinatal pathology (injuries or anomalies in newborns);
- infectious brain lesions (including congenital);
- general intoxication (for external or internal reasons);
- thrombosis;
- serious nervous shocks;
- work in hazardous industries;
- radiation damage;
- smoking;
- high degree scoliosis;
- aged over 70 years.
Kinds
Usually the patient is given a diagnosis indicating the type of angiopathy. The type of illness indicates the disease that caused the appearance of this eye pathology.
There are types of retinal angiopathy:
- traumatic;
- diabetic;
- hypertensive;
- hypotonic;
- youthful.
Causes
The cause of this or that type of retinal angiopathy is best illustrated by the type of disease of which it is a complication. Thus, damage to the vessels of the retina can be caused by:
- Disorder of the nervous regulation function responsible for the tone of the vascular wall;
- Arterial hypertension;
- Traumatic brain injuries and injuries of the cervical spine;
- Increased intracranial pressure;
- Cervical osteochondrosis;
- Blood diseases.
In addition, experts call risk factors for the development of retinal vascular angiopathy:
- Age-related changes in the elderly;
- Smoking;
- Difficult daily working conditions;
- Intoxication of the body;
- Individual characteristics/anomalies in the structure of vascular walls.
Manifestations of the disease
The main danger of retinal angiopathy lies in its asymptomatic course.
Often, retinal angiopathy is accidentally detected during a fundus examination by an ophthalmologist. When the symptoms of angiopathy become clearly visible, then this stage of the disease already requires long-term and expensive treatment.
When is it absolutely necessary to see a doctor?
This must be done immediately if a person suddenly begins to notice changes in himself in the form of:
- A sharp decrease in vision. In this case, the patient touches distant objects or is unable to read small print.
- Frequent redness of the eyes with streaks of burst blood vessels.
- The appearance of “floaters” or veils before the eyes.
- Narrowing of the visual field and peripheral vision. In this case, the patient may have difficulty seeing what is happening to the side of him: a leaving car, an approaching person, etc.
- Feelings of pulsation in the eyes.
- Frequent eye pain with minimal exertion (working at a computer, short reading or needlework).
The first symptoms of angiopathy are rarely taken into account, so the disease develops further.
The most common symptoms of this disease in the mature stage are:
- decreased visual acuity and clarity;
- deterioration or loss of color sensitivity;
- narrowing of the field of vision or blurring of it;
- the appearance of lightning, dots or white lines before the eyes.
In systemic diseases, retinal angiopathy is a consequence of the general fragility of blood vessels in the body. In this case, the patient may have minor bleeding or hemorrhages (skin, nasal, streaks of blood in the stool, etc.)
Symptoms of the disease
Source: diabet.guru In the initial stages, this disease may not show any signs.
This explains why most cases are discovered too late, when the changes are already irreversible. Patients usually complain of the following symptoms:
- blurred vision,
- objects at some distance appear blurry,
- blurred vision,
- the appearance of flashes, lightning, sparks in the eyes,
- dark spots or dots appear in the field of vision,
- nosebleeds,
- pulsation in the eyes, pain.
In severe cases, there is a risk of vision loss. Symptoms of angiopathy depend on the underlying disease that led to damage to the retinal vessels.
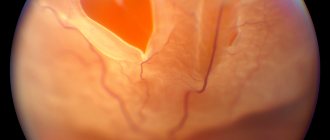
Changes in retinal vessels
Most often, ophthalmologists are faced with hypertensive angiopathy of the retina of both eyes, which develops gradually, going through several stages of its development.
At the beginning of the disease, the retinal vessels narrow, their expansion is somewhat less common, and small veins twist like a corkscrew in the area of the macula. At this stage, when examining the fundus, you can see spasmodic arteries, slight swelling of the optic nerve head and the adjacent retina.
Sometimes small pinpoint hemorrhages are found. Another characteristic sign is the symptom of “bull’s horns” - irregular branching of the arteries.
Normally, the arteries branch at an acute angle, but with hypertension they begin to change their angle towards a right or even an obtuse angle, and this leads to increased resistance in the vessels and increased pressure inside the eye.
In addition, increased pressure causes increased pulsation of blood vessels, resulting in overstretching of the vascular wall, the vessels become long and tortuous.
In the next stage - angiosclerotic, the arteries become of unequal caliber, thickened, acquire excessive tortuosity or, conversely, straightness, their walls lose elasticity and a yellowish tint appears, which gradually, as the vessel deteriorates, changes to white (silver wire symptom).
The stage of hypertensive angiopathy completes the changes that have begun and leads to changes not only in the vascular wall, but also in the retina itself - swelling, degeneration and multiple hemorrhages.
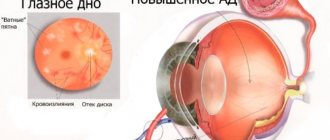
Degrees of angiopathy in hypertension
In hypertension, angiopathy is associated with overflow of the bloodstream. Depending on the severity of symptoms, the disease in hypertensive patients can have different severity: 1, 2 or 3 degrees. With hypertension, the vessels of the fundus dilate and twist, and small hemorrhages form in the ophthalmic veins. Subsequently, the retina becomes cloudy, and hemorrhages become a constant companion for hypertensive patients.
1st degree
This is the stage when the disease process is still reversible. If you begin to seriously fight the underlying disease, then changes in the eyes will be able to be eliminated.
Retinal angiopathy in the initial stage is characterized by ophthalmological disorders such as:
- varicose veins;
- narrowing of the arteries;
- increased tortuosity of blood vessels;
- discrepancies between the width of the vessels and their length.
2nd degree (moderate)
This stage occurs if there was no timely treatment at the onset of the disease. At this stage, there are already organic changes in blood vessels.
The second stage is characterized by manifestations:
- increasing discrepancies in the size of blood vessels and their tortuosity;
- narrowing of blood vessels with deterioration of blood circulation through them;
- phenomena of thrombosis and vascular hemorrhage;
- the appearance of microaneurysms and growths in the area of the optic nerve;
- narrowing of the field of view and blurring of it;
- decreased visual acuity and the appearance of myopia.
3rd degree
At this degree, organic vascular damage is maximally expressed, and vision deterioration can reach complete blindness.
Stage 3 angiopathy is characterized by symptoms:
- swelling of the retina and optic nerve:
- hemorrhages in the retina;
- white lesions:
- severe impairment of visual acuity and blurred vision (up to loss).
Fundus examinations
Angiopathy itself, or vasopathy as it is also called, is diagnosed simply; it is more difficult to find out its source. Ophthalmoscopy is used to examine the vessels of the fundus.
It comes in two types:
- Indirect. Involves the use of a lens and an additional light source. This method is the most reliable;
- Straight. For this method, an instrument is used that is equipped with a light source and special lenses, this will increase the image scale by 15 times.
Before the diagnosis, no special preparatory measures are prescribed. If the problem cannot be examined, special drops can be instilled; they will dilate the pupil and solve this problem.
What signs are characteristic of healthy eyes?
- The retina should be red;
- The blind spot must be clearly visible;
- There should be no hemorrhages in the fundus;
- Veins should be wider than arteries, and the vessels should be clearly visible;
- The optic disc is pinkish and will have a rounded appearance.
Types of illness
After visiting a specialist, not only the diagnosis is established, but also the type of angiopathy. Among the types of this disease there are types of angiopathy:
- hypertensive;
- hypotonic;
- mixed;
- dystonic;
- diabetic;
- background;
- venous;
- traumatic.
Let's consider the features of each type of these types of angiopathy.
Hypertensive type
Occurs with prolonged hypertension and is caused by blood-filled vessels. This leads to degenerative changes in the retinal vascular bundle. In this case, visual acuity often decreases and a feeling of fogginess occurs. The condition may worsen if hypertension continues to progress.
Hypotonic type
Occurs due to decreased vascular tone and stagnation of blood in the vessels. Such stagnation causes thrombosis of the capillaries. In this case, hemorrhages appear in the eyeball and retina. Vision is seriously affected by these changes.
Mixed type
Caused by disturbances in vascular regulation by the autonomic nervous system. This pathology is preceded by any systemic ailments that affect the vascular network of the body. And the capillaries of the eye fundus suffer first of all.
Although systemic diseases can occur at any age, the mixed form is more common in patients over 30 years of age. Such pathologies can lead to serious deterioration or loss of vision. The main manifestations of vascular disorder are manifestations of “flares”, blurring or pain in the eyes, and hemorrhages in the retina.
Treatment of mixed type angiopathy is closely related to the improvement of blood circulation throughout the body. Comprehensive treatment of the underlying disease can improve the condition of the eyes.
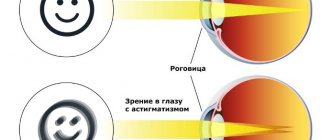
Diabetic
Occurs in diabetics. Lack of insulin in diabetes causes disturbances in glucose metabolism. However, the disease does not end there: if the insulin hormone is insufficient, disturbances in all metabolic processes (carbohydrate, protein, fat, mineral) occur in the body.
In diabetes, blood vessels throughout the body are narrowed and affected, starting with capillaries and ending with large main vessels. At the same time, blood flows slower and blood vessels become clogged. Lack of blood circulation creates problems in the tissues, depriving them of normal nutrition. In this case, the eyes are among the first to be affected, manifesting themselves in a high degree of myopia or even blindness.
Background angiopathy
Appears against the background of other diseases. With this type of angiopathy, dystrophy processes develop in the retina. This type of pathology is a consequence of a number of diseases or conditions: vascular diseases, blood diseases, autoimmune vasculitis, traumatic lesions of the neck or head, intoxication, diabetes mellitus, hypertension, high intracranial pressure, work with constant visual tension.
With background angiopathy, changes in the vascular walls disrupt their functioning. Persistent eye dysfunction leads to irreversible visual impairment, including loss of vision.
Venous
It occurs as a complication of pathologies associated with impaired blood flow. In this case, the blood flows more slowly and forms stagnations, which leads to the formation of blood clots or hemorrhages in the eyeball. The veins then become tortuous and dilated throughout. Often such a violation occurs in “experienced” hypertensive patients.
Venous angiopathy can lead to multiple disorders such as blurred vision or progressive myopia. Improvement in this disease is closely related to the treatment of the underlying disease.
Traumatic
It happens that the most minor injuries lead to a sharp deterioration or loss of vision. This often results from injuries to the neck, brain, and compression of the chest. Swelling after contusions, for example, leads to retinal opacities.
With traumatic angiopathy, the vessels of the cervical spine are compressed, while the ocular vessels are narrowed. As a result, intracranial pressure increases, which with this type of angiopathy can be consistently high. The tone of the retinal vessels suffers from this, which is expressed by constantly worsening visual disturbances, manifested by increasing myopia.
The mechanism of complications in traumatic angiopathy is due to the fact that sudden compression of blood vessels during injury also spasms the blood vessels of the eyes, which causes hypoxia of the retina with the release of fluid from it. Subsequently, the injury leads to organic changes in the retina and hemorrhages in it. This disease also affects the optic nerve, which leads to severe deterioration or loss of vision.
In newborns
This is a special type of angiopathy, which is often considered as a normal variant. Often this diagnosis is made at the birth of the baby. But sometimes angiopathy in babies can be a harbinger of congenital neurological problems.
Often, angiopathy in infants occurs after head injuries due to difficult childbirth. In this case, redness of the eyes and the appearance of spider veins are noticeable. Usually these symptoms pass quickly.
However, consultation with a neurologist for neonatal angiopathy is mandatory in any case.
The retina of babies reacts very quickly to various stresses (emotional, physical), and changes in body position. At the same time, specialists should be alert to the phenomena of any venous congestion or vasoconstriction in the eyes of children.
Often, retinal angiopathy indicates some existing pathology in the baby. Its identification and proper treatment leads to a reduction in pathological changes in the blood vessels of the eyes.
Retinal angiopathy in children
Hypertensive angiodystonia of the retinal vessels in newborns is a consequence of complicated childbirth, birth trauma, or disturbances in the intrauterine development of the child.
The following factors can provoke the appearance of pathology in a baby:
- poor maternal nutrition during pregnancy;
- genetic predisposition;
- congenital malformations of the cardiovascular system;
- fetal hypoxia;
- premature birth;
- damage to the cervical spine during childbirth.
With proper treatment, retinal angiopathy in newborns goes away within a couple of months. If the baby shows signs of angioneuropathy, then he needs to be shown to a specialist, since this phenomenon may indicate the development of such pathologies:
- diabetes;
- glomerulonephritis;
- renal retinopathy;
- blood pressure disorder.
You should immediately consult an ophthalmologist if you experience the following symptoms:
- blurred visible image;
- poor distance visibility;
- nose bleed;
- hematuria;
- Pain in the eyes;
- loss of vision.
Retinal angiopathy in older children can occur against the background of recent infectious diseases, with VSD, as well as due to disturbances in material metabolism or pathologies in the activity of retinal vessels.
Provoking factors
In addition to the causes that lead to angiopathy, it is known about the factors that provoke and aggravate the course of the disease. Often the following factors can serve as such “push” factors:
- smoking;
- elderly;
- chronic intoxication (including alcohol);
- hematological diseases with a tendency to blood clots;
- diseases with severe disturbances of neurovascular regulation (due to osteochondrosis, increased cranial pressure, head injuries);
- anatomical features of arteries.
Angiopathy in diabetics
In diabetes, this disease develops most often (angiopathy of the hypertensive type is in second place), so you need to be very careful. It is the cause of blindness in diabetics under 65 years of age. The reason for this increase is due to a constant increase in blood glucose levels, which leads to pathologies in the structure of blood vessels throughout the body.
A gradual loss of vision will be caused by the development of occlusions and blood penetration into the tissues of the retinas of both eyes, resulting in the formation of infiltrates and hemorrhages. With diabetes, there are a number of factors that can increase the likelihood of developing the disease:
- kidney disease;
- pregnancy;
- deadlines. If the disease has lasted for more than 7 years, the probability increases, but it can occur earlier if the patient does not adhere to the basic rules and recommendations of the doctor;
- smoking;
- pressure (increased).
Why is retinal angiopathy dangerous?
Angiopathy is also called a “time bomb” in the body. Impaired vascular functions can lead to dystrophic changes in the retina. In addition to deterioration of vision or myopia, the pathological process can lead to its complete loss.
If you do not take retinal angiopathy seriously, it can after some time lead to serious disorders in the form of:
- progressive visual impairment;
- hemorrhages in the vitreous body and retina or their dystrophy;
- narrowing of the visual field;
- progression of myopia;
- optic nerve atrophy;
- glaucoma;
- cataracts;
- retinal detachment;
- complete blindness.
In addition, angiopathy cannot be triggered. Untimely treatment of this disease may be ineffective. It is important to catch the disease in the phase of functional disorders, before irreparable organic changes occur in the retina.
Angiopathy in pregnant women
It occurs quite often when carrying a child, but it cannot be said that cases are extremely rare. But it is more harmless and can go away on its own 3 months after childbirth. The disease occurs due to an increase in the volume of blood that circulates throughout the body. This will not harm either the mother or the child.
But, if the mother was sick before the fetus was conceived, especially with diabetic or hypertensive angiopathy of the retina of both eyes, then complications or development of the disease are possible. It is imperative that you regularly go for preventative examinations to an ophthalmologist throughout your pregnancy to keep the situation under control. When there is a threat of retinal detachment, doctors may prescribe artificial birth.
Principles of therapy for angiopathy
Treatment for angiopathy may differ for different forms of this disease. The main principle in the treatment of any type of angiopathy is to determine the cause of the disease and treat the primary diagnosis.
That is, in case of hypertension, it is necessary to closely engage in its effective treatment, selecting medications and constantly measuring pressure. And if you have diabetes, it is important to regularly take glucose-lowering medications and measure your blood glucose.
In addition to general therapy, as angiopathy progresses, the most effective methods for restoring the retina must be selected. Most often, the following medicinal methods are used in therapy:
- Disaggregants - drugs for improving microcirculation and tissue nutrition, strengthening the vascular wall (Actovegin, Pentoxifylline, Trental, Solcoseryl, Vazonit, etc.)
- Medicines to reduce the permeability of the vascular wall (Ginkgo biloba, Xanthiol nicotinate).
- Tissue metabolism activators (Cocarboxylase, ATP).
- Vitamin therapy (Anthocyanin forte, Lutein complex, Neurorubin, vitamins B, C, E and A, nicotinic acid) to maintain good microcirculation in the eye vessels.
- Drugs to reduce the likelihood of thrombosis (Magnikor, Aspirin Cardio, Trombonet, Dipyridamole, etc.)
- Local therapy (instillation of drops with corticosteroids, Taufon, Emksi-optik, Emoksipin, Aisotin).
- Cholesterol control and reduction (Pravastatin, Atorvastatin, etc.)
- A diet limiting high-calorie foods, salt, spices, and alcohol to slow down the transformation of the retina.
In addition to the main methods, the following treatment methods have proven themselves to be excellent in the treatment of angiopathy:
- Special physical therapy to improve the functioning of blood vessels and the heart, gymnastics for the eyes, yoga asanas.
- Physiotherapy (magnetic therapy, laser coagulation, acupuncture). The device “Sidorenko’s Glasses” (combines the effects of phonophoresis, color therapy, pneumomassage and infrasound) has shown itself to be quite effective in treating this disease. Also, some private clinics use the innovative pulse therapy device STIOTRON. It is believed that this new device is capable of restoring the regeneration of damaged blood vessels and eliminating malfunctions in the eye itself.
- Massage of the neck-collar area to improve blood circulation and better outflow of eye vessels.
How and with what to treat the disease?
Therapy for retinal angiopathy should be carried out in conjunction with eliminating the source - the underlying disease. Therefore, each type of angiopathy has its own treatment algorithm.
In addition to drugs that correct the underlying disease, the following are prescribed:
- Medicines to improve blood circulation and strengthen the walls of blood vessels in the eyes (Actovegin, Trental, Kaviton, Emoxipin);
- Medicines that reduce vascular permeability (Dobesilate, Parmidine);
- Vitamin complexes to restore vision and strengthen capillaries;
- Blood thinning drugs (Agapurin, Curantil, Persantine);
- Drops that improve microcirculation (Taufon, Emoxipin);
- Physiotherapeutic measures (infrared laser radiation, magnetic therapy, acupuncture).
As maintenance therapy, plant extracts and decoctions of chamomile flowers, lemon balm and St. John's wort leaves, and hawthorn flowers and fruits can be used.
If the pathology of the retinal vessels has led to irreversible consequences, surgery will be required. One of the fastest and most effective methods of such treatment is laser coagulation.
The procedure is performed under local anesthesia and takes only 20 minutes. As a result, the damaged vessels fuse with the retina. Treatment of the disease should be prescribed by a qualified specialist.
Initially, therapy for angiopathy must be aimed at treating the main ailment, otherwise it will not bring much effect. Based on the disease that caused eye angiopathy, treatment is prescribed. The most commonly observed is hypertensive angiopathy.
Therapy should be based on taking medications that improve vascular elasticity and blood circulation. In addition to drugs to treat hypertension, medications are used to dilate blood vessels. Medicines used: Trental, Cavinton and Stugeron.
The movement of blood in the vessels is impaired due to its viscosity. Lack of oxygen is accompanied by a narrowing of the blood vessels in the fundus, so oxygen inhalations are recommended, which expand cerebral blood flow. In order for accumulations of hemorrhages to resolve, antioxidants, angioprotectors and enzymes are prescribed.
In diabetic angiopathy, the use of medications is counterproductive. Treatment includes correction of indicators: lipid metabolism, blood pressure, high sugar levels, and the patient’s weight. Laser coagulation of the retina is prescribed when irreparable changes have not yet occurred in it.
Important
If the operation is performed in a timely manner, there should be no complications. A restoration process in the vessels will be observed. For advanced angiopathy in both eyes, vitrectomy is used. You should constantly monitor your blood glucose levels and follow your diet.
If you have diabetic eye disease, vision correction is necessary. If hypotension occurs against the background of a peripheral malfunction, blood pressure is corrected and the imbalance in the nervous system is eliminated.
To do this, the following measures are used:
- getting rid of stress and bad habits;
- physical activity;
- healthy eating, eating foods with vitamin B;
- neck and limb massage;
- strengthening the immune system;
- medicinal herbal baths;
- physiotherapy,
- aromatherapy.
These measures increase the degree of tension in the vascular walls, which normalizes blood pressure. Drug treatment is necessary if these measures are not enough.
Then drugs that resist harmful effects (schisandra, aralia, ginseng), nootropic drugs (Piracetam, Glycine, Pyriditol, hopantenic acid), cerebroprotectors (Cinnarizine, Vinpocetine, Actovegin, Ginko) are prescribed.
For eye angiopathy, drugs are used that improve blood circulation: Pentilin, Vazonit, Trental, Actovegin, Pentoxifylline, Cavinton, Piracetam, Solcoseryl. Medicines are prescribed that reduce vascular permeability: Parmidine, Ginkgo biloba, Calcium dobesilate.
Medicines that reduce platelet fusion: Ticlodipine, Acetylsalicylic acid, Dipyridamole. Such medications are prohibited for pregnant women, as well as during breastfeeding and in childhood.
To treat angiopathy of both eyes, physical procedures are used: magnetic therapy, acupuncture, laser irradiation. They have a positive effect on the patient's condition with eye disease.
Treatment of retinal angiopathy of both eyes should always be carried out only as part of complex measures in relation to the underlying disease. In the absence of such an approach, treatment will have low effectiveness, and the likelihood of improvement is almost zero.
General methods of therapy:
- To reduce blood viscosity and improve its fluidity, antiplatelet agents are prescribed (Agapurin, Clopidogrel, xanthinol nicotinate, Curantil, Persantine);
- To protect blood vessels from free radicals and lipid oxidation products, antioxidants (alpha-tocopherol, ascorbic acid, Veteron, Divertin) and angioprotectors (Doxium) are used.
- To resolve foci of hemorrhage, it is advisable to prescribe enzymes (Wobenzym, Papain, prourokinase).
Treatment of angiopathy using low-energy infrared laser radiation has also proven effective.
Forecast
The prognosis for angiopathy closely depends on the correctness and timeliness of treatment of the underlying disease. Often, with timely diagnosis and proper treatment, pathological processes in the vessels of the eyes can be stopped or complications can be delayed as much as possible.
However, at an advanced stage (for example, uncorrectable high blood sugar or malignant hypertension), angiopathy can lead to partial or complete loss of vision.
In some cases, with severe angiopathy, there is a high risk of retinal detachment. In this case, a modern method of surgical treatment of this disease is used - the method of laser coagulation.
conclusions
Angiopathy is a change in the nervous regulation of retinal vessels, leading to their weakness (relaxation) or spasm. Blood supply processes are disrupted, as a result of which vision suffers. The causes of angiopathy in both eyes are usually other diseases: diabetes, hypertension, etc. As well as injuries to the spine and brain. If angiopathy is detected at the initial stage, its further development can be prevented. Lack of timely treatment is fraught with the development of dangerous complications such as retinoschisis. The main methods of treating retinal angiopathy are drugs and surgery. It is necessary to periodically visit an ophthalmologist for a preventive examination, since ocular angiopathy does not manifest itself in the initial stages.
Treatment depends on the type of ocular angiopathy. It should be timely and aimed at treating the underlying disease (diabetes, hypertension, etc.).
Prevention
Retinal angiopathy often occurs on the site of existing health problems. Therefore, to maintain eye health, it is important to take care of your body as a whole: promptly pay attention to alarm bells regarding high blood pressure, high blood sugar, progressive osteochondrosis, any head or neck injuries, etc. It is also extremely important not to overload your eyes with prolonged reading or sitting at the computer or TV, with handicrafts. In addition to the mandatory pauses, for better functioning of the eye muscles, it is advisable for people with mental work to do special gymnastics for the eyes 1-2 times a day (according to Zhdanov, Norbekov, etc.).
Knowing that the initial phases of retinal angiopathy are asymptomatic, an annual preventive examination by an ophthalmologist is important. The condition of damaged eye vessels is irreversible and can result in blindness. That is why regular visits to an eye doctor are necessary for people over 40 years of age and people with any chronic diseases. Selecting the right treatment and adjusting your lifestyle often helps to delay the development of the disease by decades.
Vascular abnormalities in the retina cannot be ignored. For any eye problems, you should consult a specialist. Only a qualified doctor should treat angiopathy, since the same symptoms can occur in different eye pathologies with completely different treatment methods. Take care of your eyes!
Sources used:
- Kvasova M. D. Vision and heredity. - Moscow / St. Petersburg: Dilya, 2002.
- Optical coherence tomography of the retina. — M.: MEDpress-inform, 2021.
- Retinal vein occlusions. Etiology, pathogenesis, clinic, diagnosis, treatment / S.N. Tultseva, Yu.S. Astakhov. - Moscow
- Wikipedia article
Diagnostics
To identify retinal vascular angiopathy, you must contact an ophthalmologist to undergo a comprehensive examination of the visual organ. The diagnosis is made taking into account the symptoms in the collected history and the data of an ophthalmological examination. To clarify the diagnosis and detail the description of the disease, special studies may be prescribed, which include:
- Ultrasound scanning of blood vessels, carried out to study the speed of blood flow and the condition of the walls of blood vessels.
- X-ray examination (with a radiopaque substance) to audit the patency of blood vessels.
- Magnetic resonance imaging, performed for the purpose of detailed determination of the structure of blood vessels and soft tissues.
After performing diagnostic measures, qualified specialists at our clinic will prescribe the necessary treatment, which they will carry out and monitor its effectiveness through dynamic observation.