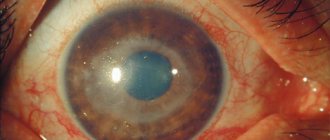
Scleral vascular injection
The whites of the eyes turn red due to dilation of blood vessels in various structures of the eyeball.
In ophthalmology, the overflow of capillaries with blood is called injection.
The sclera is colored red or purple. The condition occurs as a symptom of infectious, viral diseases, injuries. Treatment depends on the cause of the redness.
Causes of scleral injection
Injection of the sclera causes:
- attack of glaucoma;
- infections;
- conjunctivitis;
- allergy;
- dryness;
- inflammation of the choroid: iridocyclitis, uveitis;
- inflammation of the cornea: keratitis;
- a tumor of the orbit that prevents the outflow of venous blood;
- allergy;
- hemorrhage after a blow, fracture of the base of the skull, orbit;
- measles;
- coughing attacks with whooping cough.
Rarely, congestive injection of the eyeball occurs in newborns with congenital glaucoma.
Kinds
Injections are classified according to the affected vessels in the structural elements of the eye.
Conjunctival
Superficial hyperemia occurs in the outer membrane - the conjunctiva. Signs:
- short vessels do not touch the iris;
- the red color on the sclera fades closer to the center;
- as they move away from the cornea, the capillaries become wider;
- the branched blood network is clearly visible.
The vessels move along with the conjunctiva. Blood is retained and refills them when pressed.
Pericorneal
Deep or ciliary injection occurs from dilatation of the ciliary vessels of the looped network. Differences from surface form:
- long, wide capillaries reach the iris;
- purple, lilac blurry rim around the cornea;
- the vessels do not move;
- the movement of blood during compression is not traced.
The matte episcleral tissue hides individual parts of the vascular network, so the dark edging appears continuous. The width and color intensity of the injection ring depends on the thickness of the sclera and the stage of inflammation.
Mixed
Simultaneous dilatation of deep and superficial vessels caused by inflammation of the cornea.
Scleral
The injection affects the scleral, episcleral circulatory network. Signs:
- swelling of the sclera;
- blue, purple tint;
- lack of blood movement in the vessels during compression.
By nature it is divided into diffuse and limited.
Diagnostics
The degree of blood circulation in the vascular network is determined with a glass rod. The instrument is used to press the affected area and move the surface layer of the eyeball. During the procedure, immovable deep ones are visible under the movable upper vessels.
To determine the type of injection, a test is done with a solution of adrenaline, which is instilled into the eyes. Reaction on the sclera with different types of redness:
- disappearance of hyperemia after 2 minutes - conjunctival;
- lack of reaction - deep;
- narrowing of individual areas of the vascular network - mixed.
Dilatation of superficial vessels occurs with conjunctivitis. Uveitis, keratitis, and iridocyclitis cause a pericorneal appearance.
Studying the patient's medical history will help clarify the origin of the injection. Redness is caused by infectious respiratory diseases and inflammation of the cranial nerves.
Since vascular redness is caused by diseases of various etiologies, additional research is needed:
- biomicroscopy - the eye is examined with a slit lamp, in the light of which pathologies in the structure of the circulatory network are visible through the microscope;
- tonometry - high eye pressure dilates blood vessels, the procedure will determine glaucoma;
- fluorescein angiography - contrast injected into a vein will show changes in the vascular system on ultrasound;
- MRI - the affected area can be seen on a three-dimensional image of a tomograph.
Ophthalmoscopy and examination of the fundus are not informative, as they show the inner chamber of the eye, the retina.
Treatment
The main therapy is aimed at eliminating the primary disease and includes taking antibiotics and antihistamines. Injection caused by bacteria, viruses, goes away after treatment with eye drops:
- Albucid is an antibacterial drug for the treatment and prevention of inflammation of the conjunctiva, cornea, and eyelids;
- Ophthalmoferon - a drug with diphenhydramine and interferon acts as an anesthetic and promotes regeneration;
- Oftan Dexamethasone - relieves inflammation in keratitis, blepharitis, allergies;
- Ciprofloxacin is a universal antimicrobial agent.
Vasoconstrictor drops are used after making an accurate diagnosis:
- Visine - used for red eyes caused by external factors;
- Okumetil - the main component tetrazoline is supplemented with linden and chamomile extract to soothe the mucous membrane;
- Afrin - indicated for superficial injection caused by allergies;
- Visomitin - stimulates the formation of the tear film on the surface of the eye.
Redness caused by dryness can be relieved with artificial tears.
Was the article helpful?
Rate the material on a five-point scale!
( 3 5.00
Source: https://proglazki.ru/bolezni/inektsiya-sosudov-skler/
↑ Episcleritis
Episcleritis
- inflammation of the superficial (outer) loose layers of the sclera, abundantly supplied with blood vessels.
Scleritis
- inflammation of the middle and inner layers of the sclera, which are poor in their own blood vessels.
The etiology of episcleritis and scleritis is varied. They often occur in collagen diseases as a result of autoimmune disorders.
c, often as a result of toxic-allergic reactions (syphilitic and tuberculous episcleritis). A hematogenous route of penetration of bacteria and viruses into the sclera is possible (metastatic granulomatous scleritis, tuberculous and syphilitic deep scleritis).
Metastatic purulent deep scleritis
may occur if there are foci of infection in the patient’s body - staphylococcal, streptococcal, etc. Scleritis often develops with sepsis, but is also possible with furunculosis, tonsillitis, tonsillitis, osteomyelitis, etc.
The inflammatory infiltrate in scleritis consists mainly of lymphocytes, as well as epithelioid and giant cells. Along the ciliary arteries, the inflammatory process can spread to other membranes of the eye.
Purulent scleritis
contains predominantly polynuclear leukocytes. The inflammatory infiltrate in tuberculous scleritis corresponds to a typical tuberculoma.
There are anterior and posterior sclerites
, which develop respectively in the areas of the sclera supplied with blood from the anterior and posterior ciliary arteries. According to the clinical course, acute and chronic scleritis are distinguished. Due to the weak vascularization of the sclera, exudative and proliferative reactions are not expressed sharply and often have a chronic course. An acute course is characteristic of purulent scleritis.
The course of episcleritis and scleritis is different. For mild flow
the inflammatory infiltrate resolves quite quickly under the influence of the treatment.
In cases of massive inflammatory infiltration
of the sclera, necrosis of cellular elements and collagen fibers of the sclera is observed, followed by the development of scar tissue, thinning and ectasia of the sclera.
The diagnosis of episcleritis and scleritis is simple, established with focal illumination of the eye
, with biomicroscopy and ophthalmoscopy. Often, cytological and virological studies of conjunctival scrapings in the area of scleral infiltration help in establishing the etiology of the process. To establish the toxic-allergic nature of episcleritis and scleritis, the immunological method of focal tests is used by studying the reactions of the inflammatory infiltrate in the sclera (focal reactions) to cutaneous, intradermal and subcutaneous administration of specific allergens - tuberculin, toxoplasmin, staphylococcal or streptococcal allergen.
Nodular episcleritis
occurs more often in middle-aged and elderly people. Near the limbus, round nodules appear, covered with hyperemic conjunctiva that is not fused to them. Palpation of the eye is painful. The process, as a rule, is bilateral, its duration is usually 1 - 1.5 months, then the nodules resolve, leaving a slight slate coloring of the sclera. The course of the disease is long with frequent relapses followed by remissions; with relapses of the disease, nodules appear in new places, sometimes around the cornea, along the entire circumference of the limbus. Photophobia and lacrimation are usually not observed. Nodular episcleritis is differentiated from phlyctena. The purple hue of hyperemia, the absence of characteristic superficial vessels approaching the nodule, and the duration distinguish this process from phlyctenulosis.
Migratory episcleritis.
Suddenly, in one or the other eye, a flat, hyperemic focus appears, often painful, near the limbus. In some cases, changes in the eyes are accompanied by angioedema of the eyelids and migraine. These changes pass quickly, lasting from several hours to several days. The correct frequency of relapses is characteristic.
Rosacea-episcleritis.
In the case of this disease, nodules appear in the episclera, reminiscent of changes in migratory episcleritis. Usually there is also damage to the cornea - rosacea keratitis (see Keratitis). Naturally combined with rosacea on the face. The severity of the process is determined by damage to the cornea. There is a tendency to relapse.
Treatment of episcleritis
begin with frequent instillations of corticosteroid solutions (4-6 times a day).
A 2.5% suspension of hydrocortisone, a 0.3% solution of prednisolone, a 0.1% solution of dexamethasone, oftan dexamethasone, Sofradex drops, ophthalmic medicinal films with dexamethasone and Canadex are used (1-2 times a day). During treatment, corticosteroids are combined with antimicrobial drugs (Maxitrol, Macidex, Colbiocin, Tsipromed, Garazon, Eubetal, Prenacid). Instill a 20% solution of sulfacyl sodium, 10-20% solution of sulfapyridazine sodium, 0.02% solution of "..."a, 0.25% solution of chloramphenicol. Desensitizing agents are also prescribed - instillation of a 2% solution of amidopyrine with a 0.1% solution of adrenaline hydrochloride (10 drops per 10 ml of solution), 0.5% solution of diphenhydramine.
Dry heat and UHF are indicated locally It is necessary to identify the cause that caused episcleritis. When the microbial etiology of the process is established, along with general treatment, antibiotics (monomycin, gentamicin, ampicillin, kanamycin) are administered under the conjunctiva.
Injected sclera - causes of red eyes
The eye is an organ that has a rather complex structure and gives us the most complete information about the world around us.
A person’s eyes can tell a lot about him, including the state of health of his body.
Redness of the eyes is an alarming symptom that should alert you and serve as a reason to consult a doctor. You will learn from this article what may be the cause of scleral injection.
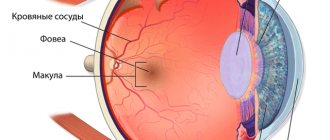
What is sclera
The sclera of the eye is its outer layer, which covers the vast majority of the surface of the eyeball. The so-called “white” of the eye is the sclera. It consists of several layers of fibrous tissue, which is formed by its constituent collagen:
- Episcleral layer;
- The sclera itself;
- Inner layer (brown plate).
The functions of the outer shell of the eye are quite extensive. Basically, this is the protection of deep layers from the harmful effects of ultraviolet rays due to their refraction, which provides a person with good quality of vision.
The sclerotic membrane also protects the eye from damage and environmental influences. Another very important function of the sclera is that it serves as a framework for the subsequent attachment of the eye muscles, ligaments and blood vessels to it.
In addition, due to its density, the sclera has the ability to take part in maintaining eye pressure.
Redness of the sclera
Often, after visiting an ophthalmologist, a person may see the following entry in the outpatient card: “sclera injected.” What does it mean? In fact, this phrase is simply deciphered - the whites of the eyes turned red. Many people often simply do not pay attention to reddened eyes, attributing it to fatigue and overwork.
These reasons are indeed the most predominant among others, but scleral injection may also indicate the presence of more serious diseases.
Redness of the sclera is caused by dilation of the blood vessels of the eye, and this can be caused by two types of factors: external and internal. Internal ones include:
- High blood or intracranial pressure;
- Inflammatory process of the eyelid margin – blepharitis;
- Infectious diseases - influenza, sore throat and others can contribute to temporary redness of the sclera;
- Inflammation of the blood vessels of the eye - uveitis.
Also, injected sclera can be a sign of diseases such as:
- Glaucoma is a chronic disease that leads to increased eye pressure. Further development of the disease provokes the death of retinal cells and atrophy of the optic nerve and, as a result, can lead to blindness;
- Arterial hypertension is a persistent and prolonged increase in blood pressure, which can serve as an impetus for the further development of heart attacks and strokes;
- Scleritis is an inflammatory process affecting the deep layers of the sclera.
External factors causing scleral injection:
- Frequent work at the computer. Office workers and avid gamers especially suffer from this. Staying in front of a monitor for a long time does not have the best effect on the condition of the eyes - the mucous membrane dries out, the optic nerve and the muscles of the fundus of the eye become overly strained;
- Wearing lenses. Undoubtedly, lenses are one of the most ingenious inventions of mankind, but sometimes wearing them can cause redness of the eyes. Follow simple rules: put on lenses with clean hands, store them in an antiseptic solution and do not confuse the lenses for the left and right eyes - each of them has its own microflora;
- For allergy sufferers, redness of the eyes may be a reaction to allergens - for example, pollen particles sticking to the mucous membrane of the eye;
- Environmental factors - cold wind, dust or cigarette smoke often provoke redness;
- Sometimes the profession can also leave its mark on eye health - for example, among welders, redness of the sclera is a very common symptom. In this case, you should consult an ophthalmologist to rule out a burn.
What is sclera
The sclera is the membrane of the eye that performs a supporting and protective function. The thickness of this shell differs in different areas. In the equator zone it is approximately 0.4 mm, and in the area of the cornea and optic nerve head its thickness reaches 0.8 mm. The sclera is quite resistant to the negative effects of external factors. But even on this shell there are areas of thinning that can be injured under certain conditions.
There are very few blood vessels in the sclera. But vessels pass through it and go to the choroid from the inside. The outside of the sclera is covered with a special loose layer, which ensures good mobility of the eyeball in the orbit. But there is almost no innervation here.
The eye muscles, which are responsible for the movements of the eyeball, are attached to the sclera. The tunica albuginea protects the visual organ from mechanical injury.
There are several congenital and acquired diseases of the sclera that affect the quality of vision.
Injection of eye vessels treatment
The blood vessels in our eyes are quite fragile. When the integrity of their walls is violated for various reasons, hemorrhage occurs in the eye tissue, blood circulation is disrupted, and metabolic processes suffer. Damage to blood vessels can lead to complete blindness. We will tell you what preventive and therapeutic agents can be used to strengthen blood vessels.
If the vessels of our body are weakened, then the metabolic process is inhibited, blood circulation is disrupted, and as a result, oxygen and microelements do not flow in the required quantities to all parts and tissues of the body, including the eyes. Poor circulation directly affects the deterioration of the quality of vision.
Blood with necessary nutrients enters the tissues through the ophthalmic artery. The most important of these are the capillaries that supply the optic nerve and retina. Since there are no valves on the ophthalmic veins, any blockage of the vessels is very dangerous for the organs of vision. Let's consider what reasons can affect the violation of the integrity of the walls of blood vessels and their rupture.
- External circumstances. The most common cause of capillary damage is a foreign body getting into the eyes, a thermal burn, or prolonged exposure to dry air. At the same time, the person begins to vigorously rub his eyes, and the integrity of the walls of the blood vessels is violated.
- Frequent and prolonged visual overload. They affect people whose professional activities involve constant eye strain - system administrators, programmers, drivers, jewelers, etc. Long-term tension when working at the same distance leads to the fact that the capillaries begin to burst. This category also includes climbers, divers, pilots, flight attendants - that is, people whose professions or hobbies are associated with constant changes in external pressure, which also negatively affects the strength of blood vessels.
- Physical overexertion.
The risk group includes athletes involved in weightlifting and loaders who constantly lift weights. At the moment when a forceful jerk occurs, the vessels suddenly fill with blood, which increases the risk of their rupture. In women, capillaries may also burst during labor, so a fundus examination should be performed after childbirth. - Injuries to the head and organs of vision. A sharp physical impact can cause hemorrhage in the eyeball. In case of severe impacts to the head or face, it is necessary to conduct a fundus examination, as well as a general diagnosis of the visual organs, in which the doctor will identify possible complications. For example, when struck, blood can leak into the vitreous and cause retinal detachment.
- Pathological processes and general diseases of the body. The weakening of the blood vessels in the eyes is also influenced by various disturbances in the functioning of the body:
- failure of the endocrine system;
- eye diseases - keratitis, conjunctivitis;
- hypertension, which is characterized by sudden jumps in blood pressure;
- intraocular tumors - they begin to compress the eyeball, which leads to rupture of the vessels inside it;
- lack of vitamins, especially rutin, A, C, which are responsible for the elasticity of the walls of blood vessels;
- sensitivity to changes in atmospheric pressure;
- reaction to taking certain medications, such as aspirin;
- alcohol abuse - hemorrhage occurs as a result of a sharp narrowing and dilation of blood vessels under the influence of alcohol components.
Angiopathy - damage to the blood vessels of the eyes
In fact, angiopathy is not a separate disease, but the consequences of diseases that affect the blood vessels of the whole body, including the retina. There are several reasons that provoke the occurrence of various vascular eye diseases.
This pathology occurs in both children and adults, but the majority of people susceptible to it are patients over the age of 30. It is divided into several types depending on the cause that provoked it.
Let's look at what types of angiopathy there are.
- Hypertensive It is a consequence of hypertension that has developed in a person. At the initial stages, this disease does not manifest itself in any way, and the patient does not suspect that he has problems with the blood vessels of the eyes. Often this is only discovered when there is noticeable visual impairment. An examination of the fundus reveals the stage of the current process:
- retinal angiopathy of the hypertensive type in the initial stage - dilation of venous vessels that become tortuous;
- angiosclerosis - loss of elasticity of the retinal arteries and their thickening, while there is a lack of blood in the arteries and its stagnation in the veins;
- retinopathy - small hemorrhages in the retinal tissue and its destruction;
- neuroretinopathy is a stage when pathological destruction affects the optic nerve, it swells and loses its contour. The consequence of advanced hypertensive angiopathy can be thrombosis of the central retinal vein, as well as acute circulatory disorders of its central artery.
- Diabetic Develops against the background of ongoing diabetes mellitus in the absence of adequate treatment. In this case, all the blood vessels of the body are affected, including the eye ones: there is a thinning of their walls, deterioration of blood circulation, and, as a result, blockage, multiple hemorrhages in the retina and a significant decrease in vision.
- Hypotonic The tone of small blood vessels decreases, blood overwhelms them, blood flow slows down and, as a result, thrombosis occurs. In this case, they begin to pulsate strongly.
- Traumatic Occurs with brain injuries, damage to the cervical spine, or sudden compression of the chest. This increases intracranial pressure and compresses the blood vessels in the cervical region.
In addition to retinal angiopathy, there are other diseases associated with the vessels of the eyes:
- chorioretinitis is one of the forms of posterior uveitis, inflammation of the choroid, which can be caused by tuberculosis, AIDS, toxoplasmosis and other diseases;
- aneurysm of blood vessels of the eyes;
- thrombosis of the central retinal vein and others.
We have touched upon only a small part of vascular eye diseases, which are very dangerous for humans and require timely treatment.
In each case, a thorough diagnosis is carried out, and then therapeutic measures are prescribed, including the use of eye drops to strengthen blood vessels.
To achieve a stable result, therapeutic measures must be carried out in parallel against the disease that has caused disturbances in the blood vessels of the eyes.
Vitamin preparations for the prevention of vascular disorders
The human visual organs in the modern world experience enormous loads every day. Most people, spending time at the computer during the day, switch to watching TV or picking up a mobile gadget in the evening.
Discomfort in the eyes, dryness, burning, blurry images have long become common symptoms for many, but few pay attention to them, attributing them to banal fatigue.
Meanwhile, such signs indicate chronic fatigue, which leads to the development of serious diseases of the retina or optic nerve, and, as a consequence, to complete loss of vision. That is why, for prevention purposes, you need to use strengthening eye drops.
How do strengthening eye drops work?
When blood vessels are weakened, blood circulation is disrupted and, accordingly, the flow of oxygen to the tissues of the eyes is disrupted. Metabolic processes deteriorate, the quality of vision decreases. As a result, the capillaries weaken even more and, as soon as they become overfilled with blood, they begin to burst, and visible hemorrhages appear on the whites of the eyes.
The active components of medicinal liquids help nourish all parts of the visual organs: lens, optic nerve, retina. They help strengthen damaged blood vessels and restore normal blood circulation.
This result is achieved with the help of vitamins and minerals that are included in ophthalmic preparations in this category.
Source: https://mir-ua.ru/inekcija-sosudov-glaza-lechenie/
Scleral injection: causes, symptoms, treatment
Injection of the sclera is the redness of the whites of the eye, which is associated with vasodilation. This pathological phenomenon is accompanied by many ophthalmological and systemic diseases.
Chronic lack of sleep or prolonged work at the computer can provoke dilation of blood vessels in the eyes. If the redness of the whites persists for too long, you should consult an ophthalmologist.
He will conduct an examination and identify the cause of this condition.
Signs and symptoms of scleral injection
Injection of the sclera always occurs with a number of characteristic symptoms. First of all, it is immediately noticeable that the white of the eye is very red. But besides this, other signs of inflammation are observed:
- There is pain in the eye of varying intensity. It can be either light and almost invisible, or shooting. Often the pain radiates to the temples, eyebrows and lower jaw.
- Pain when moving the eyeballs.
- Sensation of a foreign body in the eyes. A person has the feeling that sand is poured onto the mucous membrane.
- Tearfulness and photophobia.
- The eye appears red and swollen.
- If you look closely at the eye, you can see yellowish areas and dilated blood vessels.
- The eyelids are very swollen, with palpation the pain noticeably intensifies.
With scleritis, protrusion of the eyeball is often observed, the visual organ becomes as if bulging.
With scleritis, a decrease in visual acuity is almost always observed, which is explained by impaired blood circulation in the tissues.
When does it occur
The causes of scleritis are quite varied. The following diseases and conditions can provoke dilation of blood vessels:
- Chronic tuberculosis.
- Syphilis.
- Chronic rheumatoid arthritis.
- Ankylosing spondylitis.
- Systemic lupus.
- Sarcoidosis.
- Corneal ulcer.
- Allergic reactions.
- Various infectious diseases.
Diseases in which metabolism is disrupted can also provoke scleritis. These also include diseases of an endocrinological nature. Inflammation of the sclera can be caused by various injuries to the visual organs. Redness is often observed in the postoperative period, after eye surgery.
In rare cases, the development of scleritis is associated with the entry of pathogenic fungi into the visual organs.
Diagnostic measures
Diagnostic measures consist of studying the patient’s complaints and thoroughly examining him. In many cases, this allows the disease to be diagnosed. Additionally, a number of instrumental studies are prescribed to help confirm the diagnosis. In some cases, the doctor gives a referral for an ultrasound of the visual organs and computed tomography.
If there is a suspicion that scleritis has become a complication of some systemic disease, then a full examination and subsequent treatment are recommended.
Consequences and prevention
If scleritis is left untreated for a long time or is treated incorrectly, this leads to a number of serious complications:
- If the cornea is involved in the inflammatory process, keratitis may develop.
- If the iris and ciliary body are affected, iridocyclitis may begin.
- In some cases, suppuration begins, this indicates an abscess in the sclera.
- Secondary glaucoma may begin.
- Tissue healing with scleritis leads to the formation of a scar, which, in turn, leads to astigmatism.
- The nutrition of the eye tissues is disrupted, which leads to clouding of the cornea and impaired visual acuity.
- Swelling and even detachment of the retina may occur.
Prevention of injection of scleral vessels comes down to timely treatment of infectious and ophthalmological diseases.
You need to strengthen your immune system, for this you should eat well, exercise and walk a lot in the fresh air. Do not forget that scleritis can be caused by vascular diseases and metabolic disorders.
To avoid vision problems, it is necessary to promptly treat all chronic diseases.
Source: https://oculistic.ru/bolezni/drugie-zabolevaniya/prichiny-inetsirovannosti-skler
Scleral vascular injection – Doctor for your eyes
The eye is the main sensory organ through which a person receives up to 90% of information from the surrounding world. Many have encountered the phenomenon of “red eye” syndrome, when the sclera turns red.
The cause of vascular rupture is the fragility and fragility of the vascular wall, so strengthening the blood vessels is an important link in treatment.
Visual analyzer device
Based on the structure of the eyes, they can be classified as the most complex optical devices. The organ is located symmetrically in special receptacles of the skull - the eye sockets. It consists of many structures: the visual-nervous apparatus, the choroid, the dioptric system. All elements are enclosed in a durable outer capsule.
The choroid of the eye is located between the sclera and the retina. The vessels feeding the eye are numerous; they branch into smaller formations - capillaries, which form anastomoses with each other and gather into a dense vascular network.
The proper functioning of these structures depends on how blood is delivered to all parts of the eye. Normally, the vascular network does not penetrate the tunica albuginea.
Red eye syndrome occurs either when blood vessels dilate or because of hemorrhage, when the thin walls of the capillaries burst. All actions aimed at strengthening the blood vessels of the eyes should begin with identifying the causes of the pathology.
Many diseases directly affect the strength of the vascular wall: they increase its permeability and reduce its elasticity. Red veins or a diffuse spot on the white of the sclera is a signal of trouble in the blood supply system of the eyeball
Diseases of the choroid are severe, and given the rich innervation of these structures, with severe pain.
Causes of red eyes
Redness of the tunica albuginea often appears when some part of the eye is inflamed with the involvement of blood vessels in the pathological process. They fill with blood and expand, causing the sclera to become stained.
The mechanism of local swelling of blood vessels comes down to the effect on them of inflammatory mediators (histamine, serotonin), which can relax the vascular wall. Infectious agents are viruses, bacteria, fungi, protozoa that cause keratitis, blepharitis, stye, purulent lesions of the eyelid. An early symptom of these inflammatory diseases is red eyes.
Allergic eye damage
The anatomical and physiological characteristics of the organ of vision require constant contact with allergens, which are contained in large quantities in the surrounding air.
Allergic inflammation occurs when a foreign substance (antigen) enters the sensitive mucous membrane of the eye - the conjunctiva. The released biologically active substances (histamine, bradykinin) increase vascular permeability and cause their dilation.
Diseases of the eyeball
Sometimes hemorrhages are the first sign of the development of serious eye diseases.
Underestimation of this symptom can lead to serious complications, including loss of vision:
- Retinal disinsertion.
- Retinal vein blockage.
- Eye tumors.
- Inflammation of various structures.
Injections of blood vessels or the appearance of a capillary network on the sclera of the eyes can cause:
- visual fatigue (TV, computer),
- excessive alcohol consumption,
- lack of sleep,
- physical action - when a blow to the area of the eyeball occurs, rupture of blood vessels and hemorrhage under the conjunctiva of the eye occurs,
- eye contusions due to head injuries,
- chemical exposure - a negative effect on the eye of irritating substances at high concentrations in the atmosphere (chlorine, sulfur, asbestos and others),
- foreign body entering the eye,
- Violations of the rules for wearing contact lenses (wrongly chosen, contaminated).
Important! Hemorrhages in the eyes occur quite often in a person’s life and are not a sign of a serious illness if there are no other symptoms (pain, inflammation, blurred vision). But long-term disruption of the blood supply to the eye structures leads to disruption of their functions.
Causes of choroid fragility
The vessels of the eye are part of the general circulatory system of the human body. Pathological processes leading to changes in the strength and elasticity of the vascular wall due to diseases or age-related changes fully apply to them.
Many diseases affect the strength of the vascular wall: under the influence of various unfavorable factors, its permeability and elasticity increase. These include pathologies of the hematopoietic system, diabetes mellitus, and pressure surges due to hypertension.
Hemorrhages in the eyes due to systemic diseases are caused by:
- Reduced blood clotting (hemophilia), long-term use of blood thinning medications - anticoagulants and antiplatelet agents.
- Pathological fragility of blood vessels: connective tissue diseases (lupus erythematosus, autoimmune vasculitis), atherosclerosis, diabetes mellitus. Hypovitaminosis of vitamins C, K, P.
- Increased arterial and venous pressure with hypertension, with intense physical activity, efforts in women during childbirth, with suffocation, vomiting. In older people, blood vessels in the eyes can burst when bending over, coughing, straining, or constipation.
- In babies, strong crying leads to an increase in the intracapillary pressure of the eyes, they become filled with blood and become visible on the whites.
Methods for strengthening eye blood vessels
If it turns out that the main cause of hemorrhages is weak blood vessels, first of all care should be taken to ensure that the body receives sufficient amounts of vitamins C, K, P, A, and E along with food.
Drug treatment
Systemic administration of vasodilator drugs is indicated for concomitant diseases. You can strengthen damaged blood vessels with the help of vitamin complexes, vascular preparations, and eye drops.
Vitamins:
- C – helps strengthen blood vessels, takes part in hematopoiesis.
- P - reduces the fragility and fragility of capillaries, reduces the permeability of the vascular wall.
- K – regulates the biosynthesis of proteins involved in blood clotting.
- A – is necessary for the normal functioning of the retina.
- E – accelerates metabolic processes.
Lutein is a combined vitamin complex. Contains blueberry extract, vitamins C, E, A, trace elements zinc, copper, iron.
Optix - tablets contain lutein, beta-carotene, vitamins C, E.
Complivit Oftalmo - contains carotenoids, lutein, folic acid, a complex of vitamins: A, E, C, B1, B6, B12, minerals - selenium, zinc, copper.
Vitamins for the eyes are prescribed when there is increased stress on the organ of vision, to improve metabolic processes, stabilize cell membranes and strengthen blood vessels.
Eye drops
Taurine – reduces intraocular pressure, normalizes blood circulation. Used in the form of eye drops, 1-2 drops 4 times a day.
Oftan-Kataprom - multi-component eye drops dilate blood vessels and improve ocular blood circulation. Emoprox, Emoksipin, Emoksi-Optic (analogs) – have an angioprotective effect and can remove a blood clot.
Increases tissue resistance to oxygen deficiency. They strengthen the vascular wall. Therapy is aimed at resolving intraocular hemorrhages.
Hemorrhages vary in severity and size of the affected segment. It is possible to limit yourself to instilling eye drops only in mild cases.
Traditional methods
The use of folk remedies for eye hemorrhages is limited. Inept intervention can lead to irreparable consequences.
You can make contrasting eye baths: prepare two deep bowls - one with warm, the other with cool water. After immersing your face in a bowl of warm water, open and close your eyes several times, and do the same manipulation in a bowl of cold water.
Hardening with ice cubes. Infusion of chamomile inflorescences - a glass of boiling water per tablespoon - leave for 30 minutes. Pour into an ice tray. After freezing, apply to closed eyelids for 10 minutes.
Brew tea bags in boiling water. After cooling, place on eyes for 15 minutes.
Important! When hemorrhages in the eye occur in the posterior chamber, they are not visible, but symptoms such as deterioration in general condition, blurred vision, and pain in the affected eye are present.
Prevention
To ensure that episodes of rupture of eye vessels occur as rarely as possible, you should follow simple rules of visual hygiene.
- The diet should include foods containing the required amount of vitamins and microelements. Water-soluble vitamins C, K, P are found in currants, cherries, citrus fruits, rose hips and chokeberries, dill, parsley, and sweet pepper. Fat-soluble vitamins A and E are found in cod liver, sea fish, vegetable and animal oil, eggs, and dairy products.
- Creating conditions for proper sleep (evening walks, airing).
- Proper organization of the workplace: sufficient lighting, the distance to the screen or book should be at least 50 cm.
- Breaks are necessary when watching TV or working with a computer: every hour - 10 minutes of rest.
- Physical exercises for the eyes.
- Protect your eyes from ultraviolet radiation with glasses with a UV filter.
Numerous preventive products for strengthening fragile eye blood vessels contain herbal ingredients. They can be used for a long time with increased load on the organ of vision.
(25,00
Source: https://dcglaza.ru/inekcija-sosudov-skler.html
Posterior trepanation of the sclera
Posterior trepanation of the sclera was proposed in 1915 by FH Verhoeff for decompression of the eyeball in case of developed expulsive hemorrhage (see Expulsive hemorrhage) in order to create a free outflow of blood from the suprachoroidal (perivascular, T.) space, as well as for the evacuation of transudate with detachment of the choroid.
V.P. Filatov in 1936 proposed the use of posterior T. s. as an auxiliary operation performed before opening the eyeball cavity, for example, before cataract extraction, antiglaucomatous operations to prevent complications (expulsive hemorrhage, choroidal detachment).
Posterior trepanation of the sclera is usually performed in the lower outer quadrant of the eyeball or in the place of the greatest accumulation of transudate. After an incision of the conjunctiva along with Tenon's capsule, the sclera is exposed 5 mm from the limbus. Trepan diam. 2 mm is placed on the sclera (4-5 mm from the limbus for choroidal detachment and 8-10 mm for expulsive hemorrhage) and T. is performed. Forced removal of blood from the suprachoroidal space during expulsive hemorrhage is carried out according to the method of M. M. Krasnov (1959) by introducing air into the anterior chamber or vitreous body, provided that the incisions in the anterior part of the eye are sealed. Operation of the posterior T. s. finished by placing a continuous suture on the conjunctiva and Tenon’s capsule.
Trepanocyclodialysis is an operation of the posterior T. s. in combination with cyclodialysis (see) - indicated for open-angle glaucoma, as well as for glaucoma complicating cataract extraction (see Aphakia); it allows, before opening the eye, to slightly reduce intraocular pressure and perform cyclodialysis through a trepanation hole in the sclera. As a rule, the operation is performed in the upper outer quadrant. The trenonic foramen is formed 4-5 mm from the limbus. It is advisable to first puncture the cornea at the limbus for the purpose of dosed extraction of intraocular fluid, reducing intraocular pressure and using this channel at the end of the operation to restore the anterior chamber and wash out the hyphema (see). A suture is not placed on the corneal puncture. Trepanocyclodialysis is completed by applying a sealed suture to the conjunctiva and Tenon's capsule. Antibiotics are injected under the conjunctiva.
Bibliography:
Current issues in the diagnosis, clinical picture and treatment of glaucoma, ed., A. M. Sazonov et al., p. 98, M., 1979; Alekseev B. N. et al. Caffeine therapy according to M. Zh.: Krasnov in the treatment of ciliochoroidal detachments, Vestn., ophthalm., No. 1, p. 11, 1983; Multi-volume guide to eye diseases, ed., V. N. Arkhangelsky, vol. 5, p. 132, M., 1960; Manual of eye surgery, comp. V. P. Odintsov and K. X. Orlov, vol. 2, p. 764, M.-L., 1934; Rumyantseva A.F. Eye surgery, p. 244, Kyiv, 1959; Duke-Elder S. Fundamental concepts in glaucoma, Arch. Ophthal., v. 42, p. 538, 1949; Lehrbuch und Atlas der Augenheilkunde, hrsg. v. T. Axenfeld, S. 576, Jena, 1958; Verhoeff FH. Scleral puncture for expulsive sub-choroidal hemorrhage following sclerostomy, Ophthal., Rec., v. 24, p. 55, 1915.
B. N. Alekseev.