Amblyopia, translated from ancient Greek as “lazy eye,” is a condition in which the coordinated work of the brain and the eyes is disrupted. Vision in one eyeball decreases, all brain work is directed to the functioning of the second eye.
There are primary and secondary forms of the disease . The primary one is formed in the womb. Secondary is acquired during life under the influence of unfavorable factors.
ICD-10 code: H53.0 Amblyopia due to anopsia
Impaired binocular vision results in the inability to judge the depth and volume of what you see. The assessment of the spatial arrangement of objects is impaired.
Symptoms
There are different degrees of manifestation of the disease; with a mild course of the disease, symptoms may not be expressed. Experts have identified individual symptoms in childhood and adulthood.
Amblyopia in children manifests itself in the following symptoms:
- Strabismus.
- Tilt of the head when reading, or closing one eye.
- Poor coordination of movements.
Symptoms in adults are different:
- Double vision.
- Veil, vagueness.
- Sudden deterioration in vision for a long period or a couple of hours.
At the initial level of development, the patient is not aware of the existence of the disease and only accidentally notices the different optical powers of the eyes.
Forecast
- Visual acuity decreases.
- Vision correction doesn't help.
- In an unfamiliar place, he cannot find his way.
- One eye deviates to the side.
- Reading or focusing on an object is accompanied by closing one eye or tilting the head.
- His color perception is impaired.
- The eyes cannot adapt to the dark.
Causes of hysterical amblyopia
- Strabismic or dysbinocular. Manifests itself as suppression of the visual image of one eye (suppression). In 70% of cases, amblyopia of this type is detected with incorrect fixation. In this case, the retina is fixed in any area, with the exception of the central region. This case is considered separately and is called correct (central) fixation.
- Obscuration or deprivation. A characteristic feature is clouding of the optical environment of the visual organs. Suspicion of the occurrence of this type of disease falls if eliminating the causes of amblyopia does not help restore vision and no defects are visible in the fundus area.
- Refractive. A fuzzy image is projected onto the retina when you look at an object. Because of this, the refraction of light rays becomes unnatural.
- Anisometropic. The creation of a complete picture from images received from both eyes is disrupted. This manifestation is characteristic of different refraction of light rays in both eyes. The result of this is the display of the visible object through each retina in different sizes.
- Hysterical amblyopia or psychogenic blindness. This is a rare type of disease that occurs against the background of a state of strong excitement.
Amblyopia is a functional vision disorder. With amblyopia, the contrast sensitivity of the eye and the ability to see objects clearly (the accommodative ability of one or both eyes) are impaired. Amblyopia cannot be corrected with glasses or contact lenses. The eyes see very different pictures from each other. And the brain is not able to combine them into a single stereoscopic image, i.e. binocular vision is impaired. As a result, one eye begins to see worse.
- Visual acuity decreases.
- Vision correction doesn't help.
- In an unfamiliar place, he cannot find his way.
- One eye deviates to the side.
- Reading or focusing on an object is accompanied by closing one eye or tilting the head.
- His color perception is impaired.
- The eyes cannot adapt to the dark.
Causes
Many factors can cause vision loss in one eye. People suffering from psychosis and hysteria, premature babies, and children with developmental delays are at risk.
Most often, the disease occurs in childhood against the background of strabismus, when the work of one eye is disabled due to turning to the side.
The following ophthalmological diseases also become causes:
- Anisotropy.
- Cataract.
- Long-term clouding of the crystal.
- Drooping eyelid.
Additional facts
Toxic amblyopia was first described by the Austrian ophthalmologist G. Bier in 1817 in a patient with tobacco intoxication. Every year, about 10-12% of patients hospitalized in the ophthalmology department suffer from this pathology. Most often the disease can be diagnosed in people of working age. According to statistics, in 16% of cases of methanol poisoning, complete blindness occurs; in 68% of cases, patients react only to the movement of the hand in front of the eyes. In 16% of cases, visual acuity exceeds 0.1 diopter. In ophthalmology, the disease occurs with equal frequency among males and females. The geographical features of the spread of pathology have not been studied.
H53.0 Amblyopia due to anopsia
Diagnostics
Diagnosis should be carried out by an ophthalmologist. Eye acuity is checked using special tables. In the presence of strabismus, the angle of deviation from the norm is determined by the Hirshberg method.
To identify amblyopia, you need to be examined by an ophthalmologist. After conducting tests for eye acuity, color correction, perimetry and refraction, the doctor will determine the severity of the disease.
During a comprehensive study, additional examinations will be carried out: ultrasound of the eyeball, refractometry, skiascopy, and a consultation with a neurologist will be scheduled.
There are five known degrees of amblyopia. The decline in eye acuity occurs progressively from low to high.
↑ Optic nerve hypoplasia
A congenital non-progressive anomaly associated with a decrease in the number of axons that form the optic nerve during normal development.
↑ ICD-10 CODE
H47.3.
Other optic disc diseases.
↑ EPIDEMIOLOGY
The incidence of the disease is approximately 1 case in 50,000.
↑ ETIOLOGY AND PATHOGENESIS
A disorder of the development of ganglion cells that occurs during the embryonic period (the size of the embryo is 15-19 mm) and is caused by many factors. Typically, hypoplasia is idiopathic, but can be the result of diabetes in the mother or exposure to drugs and toxic substances (quinine, phenytoin, alcohol, etc.).
↑ CLINICAL PICTURE
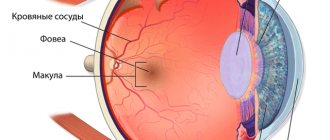
The disc is reduced in size, pale, surrounded by a faint pigment ring. The outer ring (about the size of a normal disc) consists of the lamina cribrosa, pigmented sclera and choroid. Options: yellow-white, small disc with a double ring or complete absence of nerve and vascular aplasia. With a bilateral process, the disc is often difficult to detect; in this case, it is determined along the course of the vessels.
Optic nerve hypoplasia is accompanied by bilateral vision loss (in 80% of cases from moderate to complete blindness).
If central vision is preserved, defects in the visual fields may be detected. The afferent pupillary reflex is absent. Unilateral optic disc changes are often associated with strabismus and can be seen by a relative afferent pupillary defect and unilateral weak or absent fixation (instead of positional nystagmus).
A “double ring” symptom is possible, due to the fact that the reduced disc is surrounded by pigment epithelium, filling the space from its edges to the border of the normal-sized scleral canal.
Optical hypoplasia of the nerve is rarely combined with septo-optic dysplasia (Morsier syndrome: absence of the transparent septum (septum pellucidum) and pituitary gland, which is accompanied by disorders of the thyroid gland and other hormonal disorders: growth retardation, hypoglycemia attacks are possible, often combined with mental retardation and malformations of brain structures ).
↑ DIAGNOSTICS
↑ Laboratory research
Light microscopy: reduction in the number of ganglion cell axons, thinning of the nerve fiber layer.
↑ Instrumental research
Automatic perimetry, determination of threshold sensitivity, manual kinetic perimetry according to Goldmann to identify defects in the field of view. CT, MRI: to identify missing areas of the brain (septum pellucidum, pituitary gland). EVP: to clarify the safety of axons of ganglion cells. ERG: to assess retinal function.
↑ Differential diagnosis
With atrophy or aplasia of the optic nerve.
↑ Example of diagnosis formulation
OD: optic disc hypoplasia.
↑ TREATMENT
↑ Treatment goals
Improvement of visual functions.
↑ Surgical treatment
Surgical treatment of strabismus for cosmetic purposes.
↑ Indications for consultation of other specialists
When the anomaly is combined with pathology of the nervous and endocrine systems, consultation with a neurologist and endocrinologist is necessary.
↑ Approximate periods of incapacity for work
Depends on the degree of decrease in visual acuity. In case of bilateral blindness, registration of a disability group followed by special education and employment.
Treatment
Like any other disease, amblyopia is best treated at the initial level. The younger the patient, the greater the chance of achieving success in therapy. It is almost impossible to eliminate vision problems in adulthood.
For positive vision correction, it is necessary to determine the type of amblyopia and begin therapy by eliminating the causes.
Treatment methods, depending on the type, are divided into:
- Traditional. Occlusion - turning off the healthy eye using occluders.
- Surgical intervention. Obscurational amblyopia requires correction of ptosis, removal of cataracts and correction of strabismus surgically.
- Conservative. For refractive disease, conservative methods of therapy are used. Glasses are selected and laser correction is performed.
- Physiotherapeutic. Medicinal electrophoresis, vibration massage and reflexology give good results when stimulating the sore eye.
- Psychotherapeutic. If a patient has hysterics associated with a disease, sedatives are prescribed.
Treatment is aimed at achieving balanced visual acuity in both eyes of the patient.
Primary
Determination of the angle of strabismus. The method is carried out using a synoptophore apparatus. The angle of strabismus is determined using the Hirschberg method - the reflex from the ophthalmoscope is normally located in the center of the pupil, but in case of strabismus it is asymmetrical.
Secondary
Amblyopia in children is a pathology in which there is a deterioration in visual acuity in one, or less often, two eyes. This disease is also called “lazy eye”. With amblyopia, the child does not realize that his vision is impaired.
Obscuration (deprivation) amblyopia
caused by congenital or early acquired clouding of the optical media of the eye. It is diagnosed if decreased vision persists despite elimination of the cause (for example, cataract extraction), and in the absence of structural changes in the posterior parts of the eye.
Passive pleoptics involves sealing (occlusion) of the dominant eye; active pleoptics combines occlusion of the dominant eye with stimulation of the retina of the defective eye through light, electrical impulses, and special computer programs.
Ambleopia ICD
Lazy eye syndrome in adults is diagnosed quite rarely, because in 2/3 of cases it is caused by strabismus or a difference in visual acuity in the eyes, which is detected during a medical examination of preschoolers.
With the development of moderate or high degree anisometropia, the patient is unable to see a clear image and also has difficulty oriented in space. In such people, with visual stress, the eyes quickly become tired: lacrimation, a feeling of sand and discomfort appear.
Amblyopia and its pronosis
The key to any recovery is not only the early detection of the disease, but also the impeccable implementation of all the ophthalmologist’s recommendations.
Important! The greatest effect of treatment occurs before the child reaches 6-7 years of age.
After this age, you can only count on partial recovery. In adults with amblyopia, the loss of vision is irreversible.
Poor treatment results are associated with ignoring recommendations for wearing glasses, the child’s reluctance or fear of visiting a doctor. As a result, time is missed when the optic nerve is not yet formed and can be easily corrected.
If the disease is left to run its course, the outcome will be complete blindness, especially in adulthood.
Content:
- 1 Myelin fibers 1.1 ICD-10 CODE
- 1.2 EPIDEMIOLOGY
- 1.3 ETIOLOGY AND PATHOGENESIS
- 1.4 CLINICAL PICTURE
- 1.5 DIAGNOSTICS 1.5.1 Laboratory tests
- 1.5.2 Instrumental studies
- 1.5.3 Differential diagnosis
- 1.5.4 Example of a diagnosis formulation
- 2.1 ICD-10 CODE
- 2.7.1 Treatment goals
- 3.1 ICD-10 CODE
- 3.6.1 Treatment goals
- 4.1 ICD-10 CODE
- 4.6.1 Treatment goals
Description
The causes of congenital diseases of the optic nerve are varied. Developmental anomalies are caused by mutations or the adverse effects of various environmental factors on the body of the mother and fetus. In many cases, the cause of the anomalies remains unknown. Etiological factors operating during embryogenesis and the initial stages of organogenesis (3rd week - 3rd month) can significantly affect the development of the eye. For example, many congenital abnormalities are detected with astigmatism on the optic disc, which often has an oval shape. The central cup of the optic disc can be filled:
- hyaline deposits (druze); drusen can be both on the surface and in the tissues of the optic disc, which resembles disc edema (papilloedema);
- remnants of a persistent hyaloid artery (Bergmeister's papilla), this papilla in the embryonic period passes from the disc to the lens.
Some of these and other congenital anomalies are accompanied by permanent defects in the visual field, which can cause diagnostic errors.
The following defects in the development of the optic nerve and retina are discussed below: myelin fibers, morning glow syndrome, as well as coloboma, disc pitting and optic nerve hypoplasia.
Prevention
The high level of development of medicine today does not provide guarantees or protection. The only prevention of this unpleasant disease is an examination by an ophthalmologist. The child's first appointment is scheduled in the first month of life. You can then limit your visits to one per year.
If clouding of the eye or strabismus in a child is detected early, it is necessary to promptly eliminate these deficiencies. From birth, babies must maintain a sleep-wake schedule. Children should be fed a balanced diet and health promotion activities should be carried out.
Amblyopia is a rare eye disease that reduces visual acuity. Worldwide, no more than 2% of people on the planet suffer from this disease. This disease most often affects children, so timely consultation with a doctor and the appointment of competent therapy will help restore good vision and live without glasses.
LiveJournal
Description
Toxic amblyopia.
This is visual dysfunction caused by acute or chronic intoxication. Common manifestations for all forms are a progressive decrease in visual acuity, the appearance of “fog” or “floaters” before the eyes, visual discomfort, and impaired color perception. Diagnosis is based on visometry, biomicroscopy, perimetry, ultrasound of the eye, ophthalmoscopy, and fluorescein angiography. Patients are shown etiotropic treatment, which is based on the administration of sodium bicarbonate for methanol intoxication. Calcium lactate is used for lead poisoning, keratoprotectors are used for iodine.
Pathogenesis
The development of clinical symptoms during tobacco intoxication is caused by exposure to cyanide, which is contained in large quantities in smoke. A decrease in vitamin B12 in the blood contributes to the progression of pathological changes. It has been proven that cyanide should normally be neutralized by this vitamin. With hypovitaminosis, they accumulate in the tissues of the body and potentiate dystrophic changes in the ganglion cells of the retina. In the pathogenesis of the alcoholic form, the leading role is given not to the effects of alcohol, but to endo- and exogenous hypovitaminosis. In case of poisoning with methyl alcohol, damage to the optical nerve fibers and retina occurs only at stage 3. The development of pathological changes is provoked by exposure to formaldehyde, which inhibits cellular respiration and the process of glucose oxidation. Even in minimal dosage, formaldehyde damages the inner lining of the eyeball. First, the ganglion cells are affected, then the neurons of the visual pathways. In chronic lead poisoning, clinical symptoms develop only with significant accumulation of the chemical element. Visual dysfunction is observed in almost all individuals who have been in contact with iodine vapor for a long time.