Inflammation of the cornea (that is, the front transparent part of the eye that covers the iris and pupil) is called keratitis. One of the common types of the disease is infectious keratitis ; this inflammation can be bacterial, viral, fungal or protozoal. Treatment of infectious keratitis is determined by the cause of the inflammation.
Types of disease
Herpetic keratitis of the eye is a disease in which ophthalmologists distinguish several varieties. First of all, the division occurs into primary and post-primary pathology.
The primary disease is typical for children. It is provoked by the immaturity of the immune system, and affects not only the eyes, but the entire body as a whole.
| Post-primary deviation develops in children over two years of age, as well as in adult patients. The main reason lies in the decrease in the body's defenses. |
In addition to dividing into primary and post-primary forms, ophthalmologists use another classification. In accordance with it, they distinguish:
- tree-like form, affecting the surface layers, characterized by the formation of small bubbles, which, after rupture, leave a structure resembling a tree;
- discoid variant, which is characterized by damage to the deep layers of the cornea, accompanied by a sharp decrease in vision;
- the metaherpetic form is also accompanied by deep damage to the stroma of the eye, the ulcers have a river-like structure;
- the diffuse version resembles a discoid one, but the lesion does not have clearly defined boundaries;
- keratoiridocyclitis is a type that provokes severe pain due to the involvement of the trigeminal nerve in the pathological process.
Symptoms of infectious keratitis
There are common symptoms that occur with various infectious keratitis:
- red eyes;
- lacrimation and other discharge from the eyes;
- irritation and pain, difficulty opening the eyelids;
- photophobia;
- blurred vision;
- sensation of the presence of a foreign body in the sore eye.
If you experience these symptoms, you should immediately see an ophthalmologist (for example, at our OkoMed clinic). Late diagnosis and treatment of this disease increases the likelihood of developing severe complications, including loss of vision. Next, we will look at the types of infectious keratitis and the features of their treatment.
Causes of the disease
The main factor in the development of the disease is the presence of the herpes simplex virus type 1 (HSV-1) in the body. In approximately 70% of cases, the pathogen affects the superficial layers of the eye, 20% of the damage occurs in the stromal components. Another 10% is a mixed form.
| Children and adolescents are at risk for this disease. |
In adults, the deviation is also diagnosed, but less frequently. Herpes simplex virus type 2 (HSV-2) poses a great danger to older patients. The course of the disease in this case is longer, the stroma is affected more often with irreversible changes.
HSV is present in the body of a significant number of people. However, not everyone develops keratitis. The following factors that reduce the body’s immune defense contribute to the activation of the virus in the blood:
- frequent stress exposure;
- hypothermia or, conversely, overheating of the body;
- active irradiation with ultraviolet light;
- diseases of the endocrine system;
- infections of other origins that drain the immune system.
Establishing the cause of virus activation is an important step in the fight against herpetic keratitis. If you understand which factor led to a decrease in immunity and eliminate it, recovery will occur faster.
How is it diagnosed?
Herpetic keratitis is diagnosed by examination with a slit lamp . In case of clinical suspicion, there is the possibility of performing a test called PCR (polymerase chain reaction), which very accurately detects the presence of viruses.
Sometimes dry eyes can be diagnosed, which also causes epithelial wounds in the form of dendrites or with other types of infection, such as those caused by the pathogen acanthamoeba.
Symptoms and development of the disease
Keratitis of herpetic origin develops gradually. First, the patient is diagnosed with a mild bacterial infection. A person does not see a doctor because he may not pay attention to symptoms such as red eyes for no reason and watery eyes. As the symptoms progress, photosensitivity and corneal swelling appear. Vision decreases.
The first sign of herpetic keratitis is the appearance of small blisters on the cornea. Over time, they burst and ulcers form in their place. Vision deteriorates. If one eye is affected, then only that one. If both organs are involved, then on both sides.
People often try to treat themselves using antibacterial drops. However, such treatment has no effect, since the virus is not affected by antibacterial agents. Symptoms progress rapidly.
The first episodes of the disease can be tolerated relatively easily. This is due to the fact that the disease does not immediately affect the deep layers of the cornea. However, with each subsequent relapse, the patient's condition progressively worsens.
Protozoal keratitis
Such pathologies are caused by protozoan parasites - amoebas (Acanthamoeba and Hartmanelta), which live in the soil, standing reservoirs, swimming pools, tap water and sewer pipes.
Normally, the human body does not allow the amoeba cyst to penetrate the tissue, but in case of injury to the cornea (for example, when wearing contact lenses), infection can occur. People who do not follow the rules for cleaning and storing lenses, as well as those who suffer from dry eye syndrome and diabetes, are at risk of developing protozoal (acanthamoeba) keratitis. The likelihood of infection increases after undergoing ophthalmic surgery.
This form of infectious keratitis is characterized by severe pain in the eye, redness of the affected eye and photophobia. The disease occurs in a chronic form.
Diagnostic features
Herpetic keratitis is a disease that requires careful diagnosis. The doctor may suspect a disease based on the clinical picture, but before starting treatment it is necessary to obtain laboratory confirmation of the diagnosis. For this:
- if primary infection is suspected, an intradermal test with the HSV vaccine is performed;
- perform scraping and evaluation of epithelial cells from the cornea;
- do an analysis of tear fluid;
- measure intraocular pressure in the ophthalmologist’s office using a special device;
- in the primary form, serological tests are performed to show the titer of antibodies to viral particles;
- PCR is performed - a study with the help of which it becomes possible to determine the DNA of the herpes virus in the biomaterial, to understand which strain of the pathogen provoked the disease.
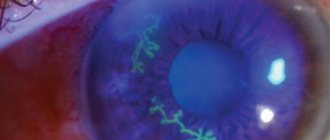
An important diagnostic step is to determine how affected the cornea is. To do this, a special substance is instilled into the patient’s eyes, capable of causing harmless temporary coloration of the element. Depending on the degree of staining of different areas, conclusions are drawn about how active the disease is.
Diagnostic measures
The disease is determined based on symptoms and analysis of concomitant infection. An external examination, laboratory tests, and visometry are carried out.
The condition and sensitivity of the cornea is assessed by:
- biomicroscopy;
- pachometry;
- microscopy of confocal, endothelial type;
- keratometry.
Erosions and ulcers are detected during a fluorescein instillation test.
A PCR smear from the surface of the conjunctiva helps to identify the causative agent of infection. Sometimes viral keratitis appears against the background of other types of disease.
A specialist will talk about inflammation of the cornea in the following video:
Conservative therapy
If herpetic keratitis has developed, it is recommended to start treatment as early as possible. Therapy is quite complex and lengthy, since the virus has the ability to easily adapt to antiviral agents. The task is further complicated by the fact that medications often have significant contraindications and restrictions for use, which makes their use difficult.
Treatment is recommended to be carried out in a hospital setting. The first step is to try to use conservative approaches aimed at suppressing the infection.
Medicines
Medicines aimed at combating the herpes virus are adapted for use in eye treatment. True, these drugs cannot completely destroy the infection in the body, but only significantly reduce its severity and put the virus into a dormant state.
Medicines are used in the form of drops or oils. This could be, for example, Valaciclovir or Acyclovir. This is where pathogenetic therapy ends. The rest of the treatment is purely symptomatic.
To reduce pain, it is recommended to treat the eyes with Lidocaine. The drug blocks the transmission of impulses, easing the severity of unpleasant symptoms.
Immunostimulating therapy may be recommended as an additional treatment. Interferon-based drugs are used to promote the production of antibodies and the destruction of viral particles.
Isoprinosine, a drug with dual effects, may be prescribed. It not only stimulates the immune system, but also has an antiviral effect against herpes. Isoprinosine, unlike other drugs, is available only in tablet form, and therefore, when used, has a systemic effect on the patient’s body.
Electrophoresis
The use of electrophoresis is of an auxiliary nature in the treatment of herpetic keratitis. The essence of the procedure is simple. A special tampon soaked in interferon is applied to the affected cornea. Application time averages 5 minutes. Under the influence of electrophoresis, the drug is more actively absorbed by body cells and has a better effect on the body.
It is recommended to repeat the procedure until a fresh epithelial layer is formed on the lesions. After a course of procedures, it is possible to get rid of the feeling of irritation of the cornea, which causes a lot of inconvenience.
After a course of procedures, a slight clouding will develop at the site of inflammation. As practice shows, it does not affect the patient’s vision in any way.
| Doctors draw patients' attention to the fact that treating keratitis caused by the herpes virus using folk remedies is strictly prohibited. |
Improper treatment will lead to progression of the disease, which, in turn, can cause significant reduction or loss of vision. Folk remedies have no effect on the pathogenic microorganism, helping to cope only with the symptoms. In order to defeat the disease, this is catastrophically not enough!
Outcomes of corneal inflammation
With a mild course of keratitis and superficial occurrence of foci of inflammation, recovery is complete, the cornea restores transparency.
In severe cases, deep infiltrates or ulcerations form, which later, scarring, leave persistent opacities. When the defect is centrally located, a persistent decrease in visual acuity occurs, which entails the need for keratoplasty.
The formation of a corneal ulcer can result in scarring or, in especially severe cases, a breakthrough into the anterior chamber - perforation.
Penetration of the inflammatory mass into the eye cavity through a corneal defect causes active intraocular inflammation, which can result in endophthalmitis and the need for enucleation - removal of the eyeball. Make an appointment
Surgical interventions
Conservative therapy is the basis for the treatment of herpes keratitis, but it is not always effective. In some cases, the disease, despite the medications used, continues to progress, and vision rapidly deteriorates. Then surgery is recommended. Two methods are used.
Scraping
The technique is the simplest and most common. Using a special device, the doctor carefully cleans off the epithelium affected by the disease. Cleaned areas are treated with an antiseptic solution. Then their healing is observed.
Keratoplasty
A complex operation that is a last resort. It is performed if conservative therapy with scraping does not have the desired effect. During the operation, the affected area of the cornea is removed, and the donor part of the organ is carefully sutured in its place.
Before keratoplasty, the patient must undergo examinations, as before a full-fledged surgical operation. The manipulation is performed only after the exacerbation of herpes keratitis has passed. During the period of exacerbation, intervention is not done, since donor tissue may be damaged and rejected.
| A quick solution to the problem is a last resort. |
It is used if the patient has advanced his disease, and there is no hope of correcting the situation using conservative methods.
Endogenous infectious keratitis
In some cases, keratitis is endogenous, developing against the background of pathologies such as tuberculosis, syphilis, malaria, etc. In this case, the infection is introduced into the eye tissue with blood or lymph. There are many types of endogenous keratitis. Thus, parenchymal keratitis becomes a complication of congenital syphilis. This disease is protracted, recurs, and is often accompanied by iridocyclitis.
When the eyes are affected by Koch's wand, phlyctenulous keratitis develops; this disease occurs mainly in children and is characterized by a pronounced corneal syndrome (pain, lacrimation, photophobia, blephrospasm) and the presence of characteristic nodules in the layers of the cornea. The onset of the disease is acute, the course is long, and relapses are likely.
Prevention methods
The prognosis of the disease largely depends on how quickly it was diagnosed and how carefully the patient follows the treatment recommendations received from the ophthalmologist. Early stages of keratitis are cured with good effect, the likelihood of relapse is minimal. Severe forms require constant medical supervision and surgical correction to maintain the ability to see.
It is much easier, as ophthalmologists note, not to treat an already formed pathology, but to avoid it. To do this, it is recommended to follow simple preventive measures to prevent the infection from activating or entering the body. Among them:
- avoiding situations in which there is a risk of eye injury;
- the use of special safety glasses if a person’s work involves repairs, construction, or welding;
- careful adherence to hygiene rules when using contact lenses, refusal to wear other people's lenses that may be infected with the herpes virus;
- compliance with precautions when working with substances that can leave a burn on the cornea;
- hardening of the body, which helps increase immunity, preventing the activation of the pathogen in the body;
- protecting yourself from overheating, hypothermia, infections and other unpleasant pathologies that can provoke an exacerbation of herpes.
There is also a vaccine that helps fight the infectious agent. It is recommended to introduce it in early autumn, before the onset of severe cold weather. It is the cold season that often causes exacerbations. Before vaccination, the patient is recommended to take a course of antiviral drugs.
Herpetic keratitis is a disease that develops slowly but steadily. If you ignore it for a long time, you can face significant inconvenience, and sometimes even lose your vision partially or completely. A timely visit to the doctor when the first suspicious symptoms appear will help protect against complications. The main thing is to follow the ophthalmologist’s treatment recommendations after the infection has been accurately diagnosed!
Varieties
Viral keratitis is a group of eye diseases that causes significant discomfort to any person. At the moment, treating specialists distinguish two forms of this disease: adenoviral and herpetic. These pathologies have a number of differences and require completely different approaches to treatment. It is for this reason that ignoring the course of the disease is extremely dangerous.
Adenoviral form
Adenoviral keratitis is a form of disease in which adenoviruses rapidly multiply in the eye. In the vast majority of cases, this problem occurs in preschool children - they encounter it due to a decrease in immune abilities. The first signs of adenoviral keratitis appear after 5-8 days. The child has the following symptoms:
- Body temperature rises significantly;
- Otolaryngological diseases appear;
- Severe headaches occur;
- The lymphatic system is affected;
- The functioning of the digestive tract changes;
- The eyelids become swollen and red;
- Severe tearing appears;
- Itching and burning occurs.
Adenoviral keratitis is easily treatable. However, before prescribing therapy, a specialist must conduct extensive diagnostics. With its help, it will be possible to determine the exact type of this disease.
It happens:
- Catarrhal - a pathological process affects the edge of the cornea. The duration of the disease is about a week, complications occur extremely rarely;
- Follicular – bubbles form on the conjunctiva of the eye;
- Filmy – a gray film forms on the conjunctiva of the eye, which is difficult to remove.
Herpetic form
Herpetic keratitis is the most common type of viral keratitis. It can be caused by the herpes simplex virus, or Varicella Zoster. The following factors can provoke an exacerbation of this disease:
- Consequences of injuries;
- Previous infections and other diseases;
- Severe hypothermia;
- Decreased immune abilities;
- Experienced stress;
- Pregnancy and other hormonal changes.
The herpetic form of viral keratitis has two forms: primary and postprimary. The first type most often occurs in children, when the body first encounters the virus.
This condition can be recognized by the appearance of a runny nose, cough, and increased body temperature. In addition, the cornea becomes cloudy and multiple bubbles form in it.
The post-primary form of viral keratitis is diagnosed in older children. It indicates increased activity of the dormant virus. The course of the post-primary form of keratitis is acute; unpleasant symptoms continue to torment the patient for several weeks. This disease can be recognized by unpleasant discharge from the eyes, photophobia, and blepharospasm.
Treatment
Acute herpetic keratitis in an advanced stage.
Only treatment for viral keratitis that is carried out in a comprehensive manner can be called correct.
Therapy of this type, in order to increase its effectiveness, should be aimed not only at suppressing viral infection or stimulating local and general immunity, but also at increasing the regenerative potential of the cornea.
As part of etiotropic therapy, the patient may be prescribed medications such as:
- Installation of interferon inducers, as well as various types of antiviral drugs. The latter include interferon and deoxyribonucleases.
- Oral administration of large doses of acyclovir is an antiviral agent, the use of which will be most effective in case of severe viral keratitis.
- The course of treatment for the problem we are considering today often also includes various kinds of painkillers, the same analgin, for example, as well as antihistamines, vitamins and antioxidants. To correct the immune status, levamisor is used, as well as extracts of the thymus gland and intramuscular injections of non-specific gamma globulin.
The photo shows medications for the treatment of viral keratitis
Deep viral keratitis, occurring with ulceration of the cornea, can sometimes lead to persistent intense clouding of the cornea, as a result of which the patient experiences a sharp decrease in visual acuity. At the same time, in order to overcome it in the early stages, using a course of treatment that includes any of the above-mentioned drugs would be quite enough!