Remember! Self-medication is not acceptable! Only an ophthalmologist can correctly diagnose and prescribe appropriate treatment.
The cornea is one of the most important optical structures of the eye (see structure of the eye). At the same time, she is very vulnerable, which is due to her almost continuous contact with the environment during wakefulness. The cornea is located in the palpebral fissure, so it is exposed to light, heat, microorganisms, and foreign bodies. A wide variety of anatomical and functional disorders (tumors, dystrophic and inflammatory processes, injuries) can occur in it. Inflammatory processes in the cornea are not always strictly isolated and, due to the common blood supply and innervation, entail changes in other parts of the eye (conjunctiva, sclera, choroid).
Keratoconus
A condition of the cornea in which its shape is significantly changed in the form of a cone-shaped protruding central zone (see.
). More often it occurs as a congenital anomaly, often combined with other developmental anomalies of the eyes and various organs. But it can also be acquired. Develops at the age of 15-20 years, progresses slowly, vision decreases gradually. At the apex of the cone, Descemet's membrane can rupture and then, due to the penetration of moisture into its tissue, the stroma of the cornea becomes cloudy. The diagnosis of keratoconus is made on the basis of biomicroscopy, ophthalmometry, refractometry, and keratometry. With keratoconus, pronounced astigmatism is detected and often irregular. Corrected with contact lenses in case of malignant disease (see.
) patients require surgical treatment - corneal transplantation.
Keratoglobus
| It differs from keratoconus in the spherical shape of a protrusion of the entire cornea, thinned by approximately 1/3 of the thickness (see.
|
More information about the surgical treatment of corneal abnormalities can be found in our flash video
Keratitis is an inflammatory disease of the cornea that occurs in approximately 0.5% of cases, but due to residual opacities, in most cases it results in a more or less pronounced decrease in visual function.
Subjective symptoms of keratitis are: photophobia, lacrimation, the presence of purulent discharge, blepharospasm, pain, foreign body sensation and decreased vision. Objective signs are a violation of the transparency and specularity of the cornea. Objective symptoms also include pericorneal injection, ingrowth of superficial and deep vessels, and sensitivity disorder.
Keratitis is characterized by such a cardinal feature as the presence of an inflammatory infiltrate (infiltrates) in various parts of the cornea of various shapes, sizes and depths. Infiltration in the cornea deprives it of transparency, specularity and shine, which is caused by a violation of the integrity of the epithelium. Most keratitis, especially superficial, leads to the fact that the epithelium in the area of infiltration is destroyed, exfoliated and eroded. Deep corneal infiltrates may ulcerate.
The clinical picture of certain types and forms of keratitis may vary depending on age, general condition of the body, properties of the pathogen, routes of spread and localization of the lesion.
Prevention
To prevent conjunctivitis, experts recommend adhering to the following rules of prevention:
- Wash your hands with soap before touching your face and eyes;
- Individual towels;
- In case of allergic conjunctivitis, do not be near the allergen to prevent its contact with the mucous membrane.
- In the professional version, wear glasses, respirators and other protective equipment.
People of different ages experience eye conjunctivitis, and each patient’s disease progresses individually. Therefore, it is very important to consult an ophthalmologist at the first signs to make an accurate diagnosis.
Eye keratitis - symptoms and treatment, photos, causes of the disease in adults and children
Blepharitis - photos, symptoms and treatment in adults
Description:
- There is no specific prophylaxis that could prevent the development of the disease.
- Secondary prevention methods boil down to the fact that allergens must be removed from the surrounding area.
- A person must adhere to a certain diet and lifestyle, which is typical for all allergy sufferers.
- If a person finds himself in potentially dangerous conditions, combination eye drops should be used, which provide an immediate effect that remains effective for half a day.
- During the period of remission, specific immunotherapy is implemented.
Doctor's conclusion and recommendations
Regardless of whether an adult or a child is allergic, it is very important to pay due attention to your health. Experts advise periodically visiting an allergist who will give recommendations based on your actual health condition.
Bacterial coccal keratitis
A creeping ulcer has a number of typical features in its clinical course and outcomes. Before the era of sulfonamides and antibiotics, such ulcers were very difficult, often ending in blindness. Currently, they are rare and occur with the best outcome, with preservation of visual acuity. A creeping corneal ulcer is most often caused by pneumococcus, which invades the corneal tissue through a defect in its surface. Coccal flora (staphylococci, streptococci, pneumococci) are present in the conjunctival sac of healthy people as saprophytes, but with a decrease in the body’s defenses they can lead to the development of the disease.
| A pathogen that has penetrated into the cornea, most often pneumococcus, due to its powerful proteolytic properties, quite quickly causes a violent inflammatory-necrotic process. In the typical course of a creeping corneal ulcer, an infiltrate with a yellowish-purulent tint appears on the first day. Purulent infiltration is located closer to one side of the defect, and the infiltrate begins to spread in this direction. The spread occurs both on the surface and in depth. The disease is accompanied by severe cutting pain, lacrimation, photophobia, blepharospasm, severe mixed injection of the eyeball and chemosis of the conjunctiva (see.
|
| In the following days, the infiltrate noticeably moves into the transparent part of the cornea and ulcerates. The progressive edge of the ulcer is undermined, the regressive edge is sloping. The regressive edge is quickly covered with epithelium and cleared. The entire ulcer gradually clears, the epithelium covers the bottom of the ulcer, forming a facet in the cornea. The corneal tissue at the site of the ulcer is then replaced with connective tissue, which lifts the epithelium. The transparency of the cornea is impaired. When an ulcer penetrates deep into the cornea, the main obstacle is encountered on the side of Descemet's membrane, which turns out to be the most resistant to the action of pneumococcus that corrodes the corneal tissue (see.
|
Remember! Self-medication is not acceptable! Only an ophthalmologist can correctly diagnose and prescribe appropriate treatment.
In our clinic, you will undergo all the necessary examinations using modern high-precision equipment and will prescribe the necessary treatment.
Bacterial keratitis
This disease develops under the influence of pathogenic microbial flora. In the vast majority of cases, bacterial keratitis develops due to damage by staphylococci, streptococci, pneumococci and Pseudomonas aeruginosa. The risk of developing keratitis increases if the following factors are present:
- corneal injury (foreign body, burn, etc.);
- wearing and improper storage of contact lenses;
- irrational use of certain medications;
- the presence of certain eye pathologies (corneal dystrophy, dry eye syndrome, conjunctivitis, etc.);
- chronic infections (such as tooth decay or sinusitis);
- diabetes;
- immunodeficiency.
As a rule, the bacterial variety of infectious keratitis has an acute onset with sharp pain, lacrimation, increased light sensitivity and spasm of the eyelids, and the disease progresses rapidly. In the corneal area there are yellow or brown infiltrates, varying in size, shape and depth of location. Purulent discharge from the eyes is usually present. The cornea takes on a matte tint and vision deteriorates.
Depending on what pathogen causes inflammation of the cornea, the symptoms of the disease vary. Thus, with keratitis associated with the proliferation of Pseudomonas aeruginosa, inflammation quickly spreads to the inner membranes of the eyeball and is very difficult. With gonococcal lesions of the cornea, a purulent whitish ulcer forms on it, which spreads both over the surface of the cornea and deep into it.
Purulent infectious keratitis requires professional treatment in an eye clinic. If the cause of purulent keratitis is not identified and specific treatment for such a disease is not carried out in a timely manner, perforation of the cornea and infection may enter the cavity of the eyeball with the most severe consequences.
Tuberculous keratitis
Tuberculous keratitis is of metastatic origin - the process can spread to the cornea from the ciliary body (see the structure of the eye) through the venous sinus of the sclera, from the iris during the formation of anterior adhesions, from the aqueous humor of the anterior chamber, from the mucous membrane (conjunctiva) or from the skin of the eyelids. There are three forms of tuberculous keratitis: deep diffuse, deep limited and sclerosing.
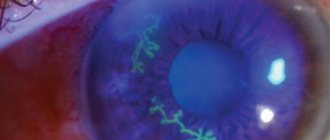
| The main clinical signs of incipient tuberculous keratitis are characterized by redness of the mucous membrane of the eye, slight photophobia and lacrimation. The cornea appears diffusely cloudy. In the depths of the opacities of the cornea, individual grayish-yellow infiltrates of different sizes are visible, to which vessels reach deep into the cornea. Near the infiltrates, the vessels branch and envelop them, giving the impression that the infiltrates are in baskets (see.
|
Development of phlyctenular conjunctivitis
Phlyctenular conjunctivitis occurs as a result of high sensitivity of the mucous membrane of the eye to bacteria. A characteristic sign of the disease is the appearance of phlyctenas on the cornea or conjunctiva - usually yellowish nodules. This reaction is caused
In this article
- Development of phlyctenular conjunctivitis
- Treatment of phlyctenular conjunctivitis
- Phlyctenular conjunctivitis in children
- Precautionary measures
tuberculous, chlamydial and staphylococcal agents. The disease is a type of allergic conjunctivitis. The most common cause of phlyctenular conjunctivitis is tuberculosis. Therefore, people suffering from this infectious disease are susceptible to it.
Phlyctenular conjunctivitis occurs in one eye, but there are cases of simultaneous or sequential involvement of both eyes. At the first stage of the disease, a person feels irritated, profuse lacrimation begins, and a fear of light appears. Then, 1-2 millimeter bubbles form at the edge of the cornea. They are clearly visible because bundles of dilated vessels approach them.
Eye infection can occur in several ways. For example, when saliva containing the causative agent of the disease comes into contact with the organs of vision, as well as through the blood. Primary infection is possible in the following ways:
- Contact. Infection occurs through mucous membranes.
- Nutritional, that is, through food contaminated with tuberculosis bacteria.
- Airborne. The most common route of infection. The pathogen enters the air during coughing and sneezing, and as a result, infection occurs when mycobacteria are inhaled.
Syphilitic keratitis
Syphilitic keratitis can be either congenital or acquired. Inflammation occurs in the posterior layers of the cornea, in its stroma (parenchyma), hence the second name for keratitis - parenchymal. Usually manifests itself between the ages of 5 and 20 years, rarely at the age of 1-5 years, and in isolated cases occurs in infants. In girls, keratitis is more common.
| The Hutchinson triad is characteristic of parenchymal keratitis: keratitis, Hutchinson teeth, hearing loss. Parenchymal keratitis is in most cases bilateral. The development of typical diffuse parenchymal keratitis begins with the appearance of moderate hyperemia of the eye, photophobia, lacrimation and clouding of the cornea, often from above, near the swollen limbus. Biomicroscopic examination shows that these opacities consist of small infiltrates in the form of dots and streaks located in the deep and middle layers of the cornea. The surface of the cornea above the clouding becomes rough. Sensitivity decreases. Gradually, all the phenomena increase, the injection increases, the clouding spreads further and further and, finally, the entire cornea becomes cloudy and dull, like a watch glass, sometimes acquiring a porcelain-white hue. Simultaneously with the appearance of opacities in the cornea, vessels appear that run in its deep layers and retain the features of deep vessels (see.
|
The period of increasing phenomena lasts 6-8 weeks, and then they gradually subside, eye irritation and injection decrease, and subjective sensations weaken. At the same time, clearing of the cornea begins from the periphery, which spreads to its center. The center remains cloudy for the longest time, clearing up last. The resorption process is very slow, and until the cornea brightens, several months pass (up to a year or more). In mild cases, the cornea appears completely transparent, and only with the help of a slit lamp are visible remnants of opacities and empty vessels that remain forever. In 70% of cases, vision is restored to one degree or another, but in some cases, when persistent opacities remain on the cornea, visual acuity decreases significantly. There may be a deviation from the described typical course of parenchymal keratitis, when inflammatory infiltration of the cornea begins from the center, and not from the periphery, and resolution of the process also occurs from the center. There are cases when very few vessels develop or are completely absent. In these cases, the resorption of opacities is especially slow. In isolated cases, parenchymal keratitis may be accompanied by severe corneal ulceration.
In almost half of all cases, syphilitic keratitis is complicated by iritis, sometimes with abundant fatty precipitates and powerful posterior synechiae. Intraocular pressure is in most cases reduced, but often it increases and sometimes even significantly. Quite often, with parenchymal keratitis, chorioretinitis is noted, which develops independently of it and can occur with both congenital and acquired syphilis. Sometimes, with acquired syphilis, gumma of the choroid may develop, and opacities may develop in the vitreous body. Rarely, damage to the optic nerve and paralysis of the eye muscles are observed. They are usually symptoms of damage to the central nervous system. Recurrences of parenchymal keratitis may occur. Acquired syphilitic keratitis, as a rule, occurs more easily and quickly.
Treatment
Phlyctenular keratoconjunctivitis develops faster than other forms of the disease.
It can get to the point where the main symptoms appear within a few hours and cause severe discomfort and pain.
And in such cases, first aid may be required.
The first action should be instillation of a suspension of hydrocortisone (two drops in each eye), after which a 1% solution of atropine sulfate is instilled and yellow mercury ointment is applied in a 2% concentration .
Keep in mind! For basic treatment, the following drugs are used:
- 10% calcium chloride solution (intravenously);
- streptomycin (intramuscular);
- anti-tuberculosis drugs (saluzide, tubazid);
- dexamethasone 0.1% in the form of drops (up to four times a day);
- Alomide (up to 6 times a day);
- cortisone (in the form and dosage recommended by your doctor);
- multivitamin complexes according to the scheme in accordance with the instructions.
Herpetic keratitis
Every year this eye disease is becoming more common throughout the world. Its course is more severe and predominantly affects children and young people. Among all inflammatory processes of the cornea, herpetic keratitis accounts for up to 70% of cases.
Herpes is one of the filterable neurodermotropic viruses. The entry gates for the introduction of the virus into the human body are the skin and mucous membranes of the oral and nasal cavities, pharynx and genitourinary organs, as well as the conjunctiva. The epithelium of the integumentary tissue also serves as a reservoir where the herpes virus is stored in an inactive state. For the virus to enter the body, at least a slight disruption of the integrity of the integument or an increase in their permeability is required. The virus can also enter the body through airborne droplets and hematogenous routes. Herpetic infection can remain latent for a long time, and sometimes throughout life. Among the factors that provoke herpes, febrile diseases come first. Microtrauma of the cornea plays a role in the provocation of herpetic keratitis. Herpetic diseases can occur after hypothermia or prolonged exposure to the sun. Vitamin deficiencies also contribute to the development of the disease. Among the endocrine factors that provoke herpes, one should mention the menstrual cycle, menopause, and pregnancy.
According to the nature of the disease, herpetic keratitis has several clinical forms: punctate, vesicular, tree-like, metaherpetic, discoid and deep diffuse uveokeratitis.
| Vesicular keratitis is a superficial form of herpes. It is characterized by the fact that small, translucent bubbles appear on the cornea in any part of it, raising the surface of the epithelium. The blisters burst quite quickly and ulcers form (see.
|
| Tree-like keratitis is manifested by the fact that the resulting herpetic vesicles merge, ulcerate and form gray grooves - cracks in the corneal epithelium, resembling a tree branch with thickenings along the opacities (see.
|
| Metaherpetic keratitis differs from the first two superficial processes in that inflammatory infiltrates lie mainly deep in the stroma of the cornea and over a large area - this is a deep form of herpes. The cornea is a massive, eroded, dull gray surface (see Fig.
|
| Discoid keratitis. In typical cases, the disease begins with swelling of the epithelium in the central or paracentral zone of the cornea. The edema quite quickly spreads to the stroma, which thickens significantly, then a grayish-white round lesion, 3-6 mm in size, is formed in the thickness, often with a rich white small spot in the center (see.
|
Remember! Self-medication is not acceptable! Only an ophthalmologist can correctly diagnose and prescribe appropriate treatment.
In our clinic, you will undergo all the necessary examinations using modern high-precision equipment and will prescribe the necessary treatment.
Viral keratitis
As the name implies, viral keratitis is a consequence of viruses entering the gas. The development of the disease is accompanied by redness and swelling of the tissues, as well as small rashes in the form of blisters.
A common form of pathology is herpetic keratitis. As is known, approximately 95% of the world's population are carriers of the herpes virus; in some cases, the balance between the host and the virus is disturbed, and a specific inflammation of the cornea develops. Watery eyes and photophobia occur, the cornea loses its shine and becomes cloudy. Pathology can affect the deep layers of the cornea, sclera and iris of the eye. Keratitis caused by the herpes virus is characterized by a long course with relapses.
Another type of viral inflammation of the cornea is adenoviral keratitis. This disease usually occurs in the cold season, is accompanied by conjunctivitis and affects both eyes. This type of keratitis is contagious to others; the infection is transmitted by airborne droplets, as well as through household objects.
Tuberculous-allergic (phlyctenulous, scrofulous) keratitis
Occurs in children aged 3-15 years and rarely in adults. The disease occurs against the background of inactive primary tuberculosis of the lungs and peripheral lymph nodes. It is an acute disease with signs of acute inflammation of the cornea. It is characterized by an acute, sometimes long-term course, frequent exacerbations and relapses. The specific substrate of this keratitis is the so-called lyktena. Phlyctena looks like a grayish-white nodule that appears in the cornea (usually at the limbus). Conflicts can be solitary (single) or multiple. Depending on the location, size of phlyctenula and vascularization of the cornea, it is customary to distinguish between superficial phlyctenulous keratitis, deep infiltrative keratitis (marginal infiltration, marginal ulcer), fascicular keratitis, pannosic keratitis, necrotizing keratitis.
| The appearance of phlyctena is accompanied by the growth of superficial vessels into the cornea in the form of a bundle stretching towards the phlyctena (see.
|
Allergic keratitis
They occur acutely after consuming intolerant medications, foods (strawberries, citrus fruits, eggs), or exposure to pollen from certain flowers. The clinical picture of these keratitis is the appearance of corneal syndrome, conjunctival-pericorneal injection of vessels and polymorphic infiltrates in the cornea.
Among metabolic inflammations of the cornea, keratitis should be noted, developing as a result of a deficiency in the body of vitamins A, E and B vitamins. Vitamin deficiencies cause various changes in the skin and mucous membranes, accompanied by loss of muscle rigidity and polyneuritis, decreased activity of the gastrointestinal tract. Damage to the cornea is caused by a violation of its sensitive and sympathetic innervation and has a certain stage.
Prexerosis is characterized by the disappearance of the tear layer in the palpebral fissure. In this regard, the conjunctiva becomes matte, dull, sometimes its pigmentation appears in the form of a triangle, with the apex towards the center. Dryness and dullness intensify with slow blinking. Superficial opacities form in the cornea.
Epithelial xerosis. During this period, xerotic dry plaques form in the form of “frozen fat” or “foam” - Iskersky-Bito plaques. They do not undergo necrosis, but the epithelium is constantly sloughed off. At the same time, the corneal epithelium peels off (hyperkeratosis). The sensitivity of the cornea is reduced. Due to the dryness of the cornea, clouding and destruction of the epithelium, visual acuity decreases. Only during this period do patients begin to complain of dry eyes and blurred vision.
Keratomalacia occurs as a result of profound vitamin deficiency and is expressed by bilateral “milky” opacification of the cornea. Turbidity, starting from the superficial layers, can cover most of the deep layers of the cornea within 24 hours. Simultaneously with the penetration of opacities deeper and wider, disintegration and rejection of the epithelium and stroma of the cornea occurs. The destruction (melting) of the cornea sometimes goes through all the layers, and then it becomes perforated and the internal structures of the eye fall out. The sensitivity of the cornea is always completely absent, and the decay process is painless. In other cases, the process stops, the ulcer scars and a powerful cataract forms with a decrease in visual acuity to light perception.
The interstitial form of keratomalacia, in addition to the phenomena of xerosis, is accompanied by a torpid corneal ulcer. The outcome of the disease is severe scarring with ingrowth of blood vessels into the cornea.
Symptoms
Symptoms of this disease are:
- painful sensations;
- photophobia and excessive lacrimation that appear in the first days;
- irritation and itching in the eyes;
- involuntary closing of the eyelids (blepharospasm);
- the formation of gray or yellowish bubbles with a diameter of up to two millimeters;
- dilation of blood vessels forming pathological ligaments near the conjunctival sacs of the eyes .
Symptoms mainly appear in one eye , less often - in both organs of vision (immediately or at intervals of several days).
Note! The pathology has such obvious signs only for one to three weeks.
After this, purulent conflicts resolve or significantly decrease, but they do not completely disappear on their own.
These are only periods of remission, which after a few weeks can be replaced by relapses and repeated rashes.
This, in turn, is fraught with additional infection with concomitant damage to vascular tissue and deterioration in the quality of vision.
Neuroparalytic keratitis
Neuroparalytic keratitis (keratitis neuroparalytica) is a typical representative of neurogenic diseases. The disease develops with paralysis of the first branch of the trigeminal nerve, as a result of operations or injections of alcohol into the area of the Gasser node, with pressure on the nerve from a tumor, bone fragments after injuries, as well as as a result of inflammatory processes. The cause of neuroparalytic keratitis is often past infectious diseases (influenza, measles, ARVI and others). Sometimes keratitis develops quickly, one to two days after damage to the trigeminal nerve, and sometimes several months later.
The disease begins with a mild pericorneal injection, which does not intensify in the future and may even disappear completely. Many very small gray, slightly raised dots appear in the corneal epithelium. In typical cases, the process in the cornea occurs in the center, where the epithelium is rejected and a defect is formed. The resulting ulcer proceeds very sluggishly and does not cause any subjective sensations; There are no symptoms of irritation, photophobia, or lacrimation. The sensitivity of the cornea is completely lost. The ulcer either heals or grows again. This can drag on for a very long time. If a secondary infection does not occur, the ulcer will heal, leaving varying degrees of cloudiness, and if it does, the ulcer may become purulent, followed by a severe outcome.
Fungal keratitis
| Fungal keratitis is caused by various types of parasitic fungi; their diagnosis is very difficult, since they resemble indolent bacterial keratoconjunctivitis with scanty discharge. In the cornea, grayish-whitish thread-like or petechial, loose-dry infiltrates appear with relatively smooth, clear contours, but with a perifocal yellowish zone (see.
|
Corneal dystrophies
| Corneal dystrophies are divided into primary (congenital) and secondary (acquired). Primary dystrophies are caused by metabolic disorders, mainly of protein metabolism, they require systematic inpatient monitoring in the ophthalmology department (see.
|
Causes
Phlyctenular keratoconjunctivitis is a consequence of complex allergic reactions that occur to a number of pathogens that affect lung tissue :
- Koch's tuberculosis bacillus;
- chlamydia;
- staphylococcus
It is worth noting! This type of keratoconjunctivitis is not a primary ophthalmological disease, but occurs only in patients with tuberculosis who are prone to allergies.
Due to such features of the etiology of the disease, complex step-by-step treatment according to a strict scheme is required.
And therapy control is carried out not only by an ophthalmologist, but also by a phthisiatrician who treats tuberculosis as the root cause of damage to the organs of vision.