Causes of keratitis:
The following reasons can lead to the development of an inflammatory process affecting the cornea of the eye:
- The presence of a foreign body in the conjunctival sac or on the cornea;
- “Dry eye” syndrome, which develops against the background of eyelid diseases, some neurological diseases, menopause, impaired tear formation or vitamin A deficiency;
- Eye allergies;
- Exposure of the eyes to excessively bright light, for example during welding without using a protective shield or glasses;
- Violation of the rules for wearing and disinfecting contact lenses;
- Long-term use of eye ointments with corticosteroids.
The causative agents of keratitis are:
- Mushrooms - aspergillus, fusarium, candida;
- Protozoa – Acanthamoeba;
- Bacteria – pseudomonas, streptococci, Haemophilus influenzae, staphylococci;
- Viruses – herpes simplex virus, adenovirus.
Signs and manifestations of keratitis
Since the cornea belongs to the light-conducting and refractive system of the eye, if a patient has keratitis, symptoms and treatment are primarily related to visual impairment and refraction, that is:
- Anomalies of the picture (blurredness, indistinguishability of details, changes in accommodation, difficulties in viewing close or, conversely, distant objects);
- Dotted, tree-like or disc-shaped areas of opacification on the cornea;
- “Sand” in the eyes, photosensitivity, lacrimation, pain and reflex closure of the eyelids (corneal or corneal syndrome);
- Scanty discharge from the eyes, redness at the border of the sclera and cornea (limbus).
Types of keratitis:
Keratitis can be of endogenous or exogenous origin. Endogenous keratitis occurs under the influence of internal causes present directly in the patient’s body. With exogenous keratitis, the inflammatory process is caused by a number of external factors.
Based on the nature of inflammation, keratitis is divided into acute, recurrent and chronic.
Depending on the exact location of the pathological changes, central and peripheral keratitis are distinguished.
Depending on the reason that caused its development, keratitis is divided into the following types:
- Viral keratitis. Their causative agent is the herpes virus or adenovirus. Herpetic keratitis develops as a result of activation against the background of a general decrease in immunity of the herpes virus (Herpes Simplex) present in the nervous tissue of many people. In most cases, this form of the disease is chronic, in which periods of remission are followed by periods of exacerbation. It is almost impossible to completely cure herpetic keratitis. According to medical statistics, in 60% of cases, corneal blindness is caused by herpetic keratitis. Adenoviral keratitis can develop as one of the complications of colds.
- Fungal keratitis usually develops against the background of massive antibiotic therapy and in people with reduced immunity. It manifests itself as redness of the eyes and severe pain.
- Bacterial keratitis. Its causative agent is most often Staphylococcus aureus. Observed in traumatic eye injuries. It may also occur in contact lens users who violate hygiene rules.
- Allergic keratitis. This form of the disease is caused by an eye allergy to pollen and/or the presence of certain bacterial toxins in the tear fluid.
- Autoimmune keratitis occurs as a result of complex disorders in the activity of the human immune system, as a result of which it begins to recognize the corneal tissue as foreign and attack it.
Keratitis can occur in severe, moderate or mild form. Often the inflammatory process spreads to other parts of the eye, leading to the development of keratoconjunctivitis, keratouevitis, etc.
Prevention of keratitis when using contact lenses
Nowadays you won’t surprise anyone with contact lenses. Disposable, reusable, soft and hard, long-term wear, for vision correction and decorative - these tiny plastic hemispheres have long and firmly taken their place on pharmacy shelves and bathroom shelves. However, contact lenses should not be taken lightly. If used incorrectly, they can lead to the development of keratitis. This is an inflammation of the cornea - the transparent outer layer of the eye, which is in contact with the inner surface of the lens.
Alarming symptoms:
- Vision decreases, the picture looks blurry.
- The mucous membrane of the eye turned red, and the conjunctiva acquired a pink tint.
- The eye hurts even after removing the lens.
- Painful sensations in bright light.
- Sensation of a foreign object in the eye.
Keratitis
Keratitis is caused by a variety of causes.
Bacterial keratitis
This type of keratitis is caused by the activity of Staphylococcus aureus or Pseudomonas aeruginosa. Bacteria enter the cornea from the skin or from water if the lens is not sufficiently cleaned or handled with dirty hands. Other risk factors for bacterial keratitis:
- wearing lenses at night while sleeping
- incorrect selection and use of hard lenses
- insufficiently washed lenses
- storing lenses in tap water
- using someone else's lenses
This type of keratitis requires careful diagnosis and treatment with drops containing antibiotics and special gels that protect the cornea.
Parasitic keratitis
This type of keratitis is most common among contact lens wearers. It is caused by a single-celled parasite, the amoeba Acanthamoeba, which can live in unboiled tap water. The amoeba gets into the eye if lenses are stored in containers with added tap water, as well as when swimming in dirty ponds and pools, especially heated ones. Amoebic keratitis is a very serious eye disease that, without urgent and serious treatment, can lead to blindness.
Viral keratitis
In most cases, viral keratitis is caused by the herpes simplex virus. As a rule, infection of the eye occurs when the contents of herpetic blisters from the mucous membranes of the lips or mouth come into contact with a contact lens. This usually happens if the lenses are handled with unwashed hands.
Herpetic keratitis is very severe and can recur: deep ulcers form on the mucous membrane, penetrating into the deep layers of the cornea, and sometimes a deep cataract develops.
Fungal keratitis
Wearing contact lenses increases the likelihood of developing fungal keratitis. This can happen if the eye is injured or small particles of plants or soil get under the lens. People with weakened immune systems are at even greater risk. Most often, this type of keratitis is caused by fungi of the Aspergillus and Candida families. Fungal keratitis can affect the deep layers of the cornea and lead to the formation of a cataract. Its diagnosis and treatment are quite difficult and often lead to treatment errors.
Prevention
To avoid risks when using contact lenses:
- Remove lenses immediately if you feel pain, your eyes are irritated or red.
- Be sure to wash your hands with soap and water before removing or putting in lenses
- rinse the lenses thoroughly in a solution specially designed for this purpose
- store lenses in a special container
- never use running water to rinse lenses
- never dilute the cleaning solution with plain water
- Avoid showering, bathing or swimming in a pool while wearing contact lenses
- Do not leave lenses in overnight unless they are re-purposed for this purpose.
- never wear someone else's contact lenses
- be sure to consult a doctor if you experience any unpleasant symptoms after wearing lenses
Diagnosis of keratitis
To diagnose corneal inflammation, the following diagnostic methods are used:
- Determination of visual acuity using a sign projector or special tables - visometry;
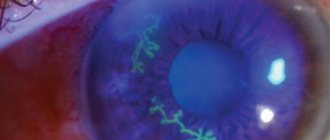
- Examination of the eye using a slit lamp - biomicroscopy;
- Examination of the cornea using special dyes - fluorescein test.
To determine the pathological agent that caused the development of keratitis, the polymerase chain reaction method is used.
Microsurgical treatment of keratitis
When corneal ulcers form due to eye keratitis, treatment consists of localizing the defect using a laser, diathermocoagulation, and cryodestruction. You can try to remove the resulting cataract with an excimer laser, or transplant a donor cornea into the patient. The last type of intervention is performed for corneal perforation and common cataracts leading to blindness. Any types of laser microsurgery are performed at the I. Medvedev Center using modern equipment by top-class masters!
Consequences of keratitis
If a patient has keratitis whose treatment is not carried out or is delayed, ulcers and perforations of the cornea occur, in 8% of cases the eye dies, in 17% the surgeon removes it due to the failure of treatment. Corneal opacities or cataracts (leukomas) impair vision and require a corneal transplant.
Separately, it is worth touching on such a disease as a conjunctival cyst of the eye, the treatment of which consists of its removal. Mucosal cysts are formed due to blockage of the mouths of the glands in it and look like small transparent bubbles or seals under the skin of the eyelids. Such formations interfere with blinking and irritate the eyeball, so they should be removed. It is best to use a laser or high-frequency current, without scars, blood and pain under local anesthesia.
The use of lasers in ophthalmological practice makes it possible to perform operations of any complexity, shorten the period of disability, reduce the number of complications and carry out interventions that were previously impossible (laser correction of corneal damage, excision of cataracts).
Specialists from the ophthalmology department of the I.Medvedev International Center for Health Protection were among the first to introduce laser microsurgery and therapeutic laser. We successfully use advanced technologies in the field of ophthalmology to this day! Choose the best!
——————————————————— If you need to get professional advice from a doctor, visit I. Medvedev’s medical clinic. You can make an appointment by calling +7 495 681 2345 or filling out the form
Causes
The appearance of keratitis is also promoted by long-term work in front of a PC screen, without a break (dehydration of the eye due to overload), excessive exposure to the sun without eye protection, contact lenses, decreased lacrimation, diseases of the fifth cranial nerve, immunosuppressants (drugs that affect the immune system). system), as well as eye contact with contaminated liquids (for example, high chlorine content in swimming pools).
Other causes of keratitis include genetic factors, trauma to the cornea (eg, burns, ultraviolet rays), or diseases such as diabetes, cancer, autoimmune diseases, or HIV.
Classification
There are several classifications of corneal inflammation. Keratitis can be divided into:
- Exogenous, associated with external factors;
- Endogenous, caused by internal changes in the human body.
According to another classification, acute, chronic and recurrent keratitis are distinguished. Based on the location of the source of inflammation, central and peripheral variants are distinguished. Sometimes the inflammatory process spreads to neighboring structures of the eye, resulting in keratoconjunctivitis, keratouveitis and other diseases.
After laser vision correction, infectious keratitis usually occurs due to the ingress of microorganisms from the external environment. Chronic eye infections, such as the herpes simplex virus, often worsen in the postoperative period.
Features of the course of the disease
In the first month, the disease may manifest itself with the following symptoms:
- slight photophobia and lacrimation;
- the appearance of a violet-red rim around the cornea (the so-called pericorneal injection);
- In the substance of the cornea, upon examination, the ophthalmologist may notice an accumulation of infiltrates - cells uncharacteristic for this area in the form of dots, strokes, dashes;
- rough surface of the cornea, swelling of the epithelium.
As the disease progresses, blood vessels become involved. One and a half to two months from the onset of the first symptoms, deep vascularization begins - the formation of new pathological vessels. They grow into the corneal tissue, leading to their thickening. The cornea looks like cloudy glass and has a rough surface. The patient complains of increased pain in the eyes and decreased clarity of vision.
During a biomicroscopic examination, the doctor may detect specific deposits on the posterior surface of the cornea. They destroy the protective barrier, and liquid begins to leak into the corneal tissue from the vessels.
After two months, the symptoms of syphilitic keratitis begin to decrease. The corolla around the membrane becomes less bright, pain and irritation subside, the cornea gradually brightens - from the peripheral zones to the central ones. This period of resorption can last from several months to a couple of years. In 7 out of 10 patients, vision is at least partially restored, but in 30% of cases the damage is too severe, and the clarity of vision decreases irrevocably.