Causes of keratitis
In the vast majority of cases, the cause of keratitis is inflammation caused by bacteria or viruses. In its “pure” form, keratitis is quite rare; more often it is observed together with conjunctivitis - inflammation of the mucous membrane of the eye.
Normally, microflora is constantly present in the conjunctival cavity and does not have a pathological effect. But, with the slightest damage to the surface epithelium of the cornea, penetrating into the wound, it can cause an inflammatory process that disrupts the transparency of the optical media.
Causes of keratitis:
- viruses.
Viral etiology is determined in the largest number of cases of the disease. About 60-70% are herpes simplex and herpes zoster viruses (shingles). In second place is adenovirus, followed by measles keratitis, chicken pox, etc.;
- bacteria.
These pathogens form purulent infiltrates or ulcers. By their nature they can be nonspecific (strepto-, staphylo-, pneumococci, bacilli - Pseudomonas aeruginosa, intestinal, etc.) and specific (against the background of tuberculosis, syphilis, chlamydia, etc.). A special case is acantabaemal keratitis, a severe form of eye disease caused by a pathogenic protozoan. More often occurs when the rules for wearing contact lenses are violated - swimming in soft lenses, adding a new solution to an old one, rinsing soft lenses with water, etc.;
- fungi – aspergillus, candida, fusarium;
- exposure to UV radiation;
- allergies to medications (in the form of drops);
- disturbance of innervation – neurotrophic keratitis;
- general diseases - rheumatoid arthritis, Sjögren's disease, etc.
General diseases and conditions that reduce the body's protective functions - diabetes mellitus, hypovitaminosis, asthenia - aggravate the course and complicate the treatment of keratitis.
Symptoms
Body signals that indicate inflammation of the cornea are:
- pain in the eyes of varying degrees of moderation;
- decreased visual acuity;
- corneal clouding;
- photophobia;
- sensations of “sand in the eyes”, discomfort;
- blepharospasm.
However, there are also specific symptoms that indicate a specific form of the disease, since when diagnosed with keratitis, the symptoms depend on the cause of inflammation of the cornea. Thus, viral keratitis can be distinguished from other types of disease by the presence of vesicular rashes, spots and streaks of irregular, asymmetrical shape, trigeminal neuralgia.
Primary herpes keratitis is characterized by an acute course: in addition to the main symptoms, a blistering rash is observed on the eyelids, lips, wings of the nose and other areas of the skin. Light foci of opacities and bubbles are visible on the cornea. Post-primary herpes keratitis is characterized by corneal edema, spasmodic closure of the eyelids (blepharospasm), slower regeneration of damaged epithelium; gradual ingrowth of newly formed vessels into the cornea is observed. The sensitivity of the cornea of the eye sharply decreases or completely disappears. This form of the disease lasts for about 2-3 weeks. Fungal keratitis, also known as keratomycosis, is often introduced into the eyes through mechanical damage to the mucous membrane of the eye by cereals, wood, and soil on which fungi (molds, yeasts, radiata) are present. Cloudiness appears on the cornea, and at the site of the lesion there is a compaction in the form of an accumulation of cellular elements and blood (infiltrate), which may have raised edges. As a result of complications of inflammatory eye diseases, such as blepharitis, conjunctivitis, meibovitis, superficial marginal keratitis develops. This occurs due to the fact that, against the background of the underlying inflammatory disease, the nutrition of the cornea of the eye is disrupted, since it is compressed by the inflamed and swollen eyelids and conjunctiva. On the damaged, compressed cornea, compactions appear, after which ulcers form - they bother the patient. At the same time, the symptoms of marginal keratitis do not have any specific differences from the standard clinical picture of the disease. Elderly people are susceptible to the appearance of marginal corneal ulcers as a consequence of trophic disorders in the body. This disease is caused by pathologies and keratitis of unknown cause. A creeping corneal ulcer occurs after damage to the anterior surface of the cornea. It differs from a regular ulcer in the presence of pus and the involvement of the iris in the inflammatory process. Non-penetrating eye injuries, contusions, foreign body penetration, chemical and thermal burns cause traumatic keratitis. This type of inflammation of the cornea is also directly related to occupational diseases. It can be caused by the following reasons:
- dust – regular exposure to metal, textile, coal, cement, lime dust causes inflammatory diseases of the organs of vision: conjunctivitis, keratitis, keratoconjunctivitis;
- chemicals in the form of fumes, dust, gas cause keratoconjunctivitis;
- radiation – causes eye burns, photophobia, and frequent eyelid closure. Metal deposition in the body reduces visual acuity.
Classification of keratitis
The disease is classified according to several factors: cause, severity, depth and localization of pathological foci.
Keratitis is distinguished:
- Superficial and deep. Superficial are pathological foci located under the epithelium or covering 1/3 of the stroma. Deep – extending over the entire thickness of the cornea;
- Central, paracentral and peripheral. Unfavorable prognosis for vision with keratitis located centrally in the pupil area;
- Exogenous and endogenous. The exogenous nature of keratitis involves the entry of a pathological factor from the outside - bacteria, viruses, fungi, injuries, etc. Endogenous - tuberculosis, syphilitic, neurotrophic, etc.
Diagnosis of keratitis and the formation of a diagnosis takes into account classification criteria, for example: “Acute adenoviral superficial central keratitis.”
Forms of keratitis
A rare form of keratitis is fungal keratitis. This pathology develops after a minor injury to the eye, which can occur if a foreign body gets into the eye. Most often, this form of keratitis is observed in residents of rural areas. If the patient does not seek help from a specialist, the infection may spread further and affect the entire eye.
Symptoms of infection appear a couple of days after infection. If the foreign body is not removed from the eye, then keratitis can develop into a creeping ulcer. Symptoms of fungal keratitis:
- the focus of inflammation is yellow or white;
- the inflammatory focus is quite large;
- dryness is noted at the site of inflammation, sometimes the affected area resembles cottage cheese;
- the focus of inflammation is surrounded by a roller, which serves as the boundary of infiltration.
Often these symptoms do not change in any way for several days, but the disease continues to develop, so that the cushion gradually disintegrates and the corneal cells die.
The inflammatory focus can itself separate from the cornea, and in its place a depression forms, which over time turns into a thorn.
Viral keratitis is caused by viruses in the body. Most often it occurs in children during adolescence. As for the localization of the source of inflammation, it can be either on the upper layer of the cornea or go into its deeper layers. With this form, the cornea becomes opaque, vision sharply decreases, and in severe cases, the corneal tissue may become dead.
The disease is caused by herpes zoster or herpes simplex. Viral keratitis, in turn, is divided into several subtypes - tree-like, diffuse, punctate, discoid, metaherpetic, vesicular.
Types of keratitis
Symptoms of the disease are characterized by frequent repetitions and a long course of the disease. Small bubbles appear on the cornea, sensitivity decreases, and trigeminal neuralgia may develop. The patient's eye turns red and pain symptoms appear; Once the blisters burst, ulcers may appear. With each relapse of the disease, visual acuity will decrease.
You can completely lose your vision with ulcerative keratitis. The result of the disease is scarring on the cornea. The edges of the cornea are mainly affected, but the central zone can also be affected.
The size and shape of the sores may vary. At first, the patient feels pain, which especially intensifies when blinking, then severe tearing and photosensitivity appear, and in rare cases, purulent compartments can be noticed.
Injuries to the cornea can cause traumatic keratitis. This could be an eye contusion, a thermal or chemical burn, or a foreign body getting into the eye. As the disease progresses, the vessels grow into the cornea.
If the keratitis is superficial, then branching of blood vessels can be observed; if the injury was deep, then branching of the vessels is accompanied by germination into the cornea. As a result of the formation of erosion, the patient suffers from pain and lacrimation. One of the symptoms of the disease is twitching of the upper eyelid.
Punctate keratitis is characterized by small dots that create a defect in the cornea. The eyes turn red, vision deteriorates, lacrimation appears, and the patient feels tingling and roughness in the eye.
Symptoms and diagnosis of keratitis
With keratitis, a so-called pericorneal injection occurs - redness of the eye, more pronounced around the cornea. If the conjunctiva is also involved in the pathological process, the redness is total, the eye is bright red.
This is accompanied by corneal (or corneal) syndrome, which includes the following symptoms:
- photophobia;
- lacrimation;
- reflexive squeezing of the eyelids – blepharospasm;
- foreign body sensation;
- pain, stinging in the eye;
- when the pathological process is localized in the central or paracentral sections - decreased visual acuity.
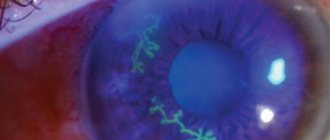
Diagnosis of keratitis at the first stage includes taking an anamnesis (clarification of the connection with previous general diseases, injuries), testing visual acuity, examination at a slit lamp (biomicroscopy) - determining the degree of decrease in visual functions, the depth of occurrence, the prevalence and localization of inflammatory foci, the presumptive cause diseases. A fluorescein test is performed to determine the integrity of the epithelium - the surface of the cornea is stained and examined in the light of a slit lamp with a blue filter. In some cases (neurotrophic, herpetic keratitis), superficial corneal sensitivity is determined.
Further diagnosis of keratitis is laboratory; it consists of bacteriological and cytological examination of a smear from the surface of the cornea and conjunctiva. If necessary, an immunological study, allergy tests, etc. are carried out, depending on the suspected cause.
Treatment
In case of keratitis, treatment is carried out only after determining the cause of inflammation of the cornea of the eyes by a qualified ophthalmologist. The treatment process itself should take place in a hospital under the supervision of an ophthalmologist for 2-4 weeks, depending on the stage of the disease and the patient’s condition. The viral form of the disease can be cured by prescribing antiviral drugs and immunomodulators. Diagnosis of a secondary infection requires treatment with antibiotics. Treatment of fungal keratitis consists of prescribing antifungal drugs, to which the type of fungi found on the cornea is sensitive. The protracted form of the disease also requires layer-by-layer therapeutic keratoplasty - a microsurgical operation to partially or completely replace the cornea of the eye. The traumatic nature of keratitis is treated with eye drops that contain anti-inflammatory drugs, substances that accelerate tissue regeneration, and vitamins. They relieve inflammation, improve trophism and accelerate epithelization. For all types of keratitis, drops containing painkillers or anesthetics are prescribed to relieve pain.
Treatment of keratitis
In most cases, treatment of keratitis is carried out on an outpatient basis, in severe cases - ulceration, deep massive infiltrates, keratouveitis - in a specialized hospital department. The duration of therapy depends on many factors, from 7 days to several weeks.
At the first visit to the doctor, before laboratory diagnosis of keratitis, empirically prescribed broad-spectrum antibacterial drugs, often on an ointment basis, and an antiviral agent (for example, Floxal ointment and Oftalmoferon insillation). Before starting therapy, smears are taken for laboratory testing. If both medications are prescribed in drop form, as a rule, the regimen also includes an eye gel for speedy regeneration - Korneregel, Actovegin, Solcoseryl, etc. If treatment of severe keratitis is carried out in a hospital, antibiotics can also be prescribed in the form of injections - subconjunctival, parabulbar, intramuscular and intravenous. After laboratory diagnosis of keratitis, clarification of the pathogen and its sensitivity to antibiotics, the drug may be changed.
In some cases, based on the characteristic clinical picture, the doctor immediately identifies keratitis as herpetic or adenoviral. In these cases, the emphasis is on antiviral drugs in the form of drops and ointments (for example, acyclovir ointment and Oftalmoferon drops, Poludan). Even with full confidence in the viral etiology of keratitis, antibacterial drops are prescribed as a prevention of secondary infection. Quite often, the course of treatment for keratitis includes tablet forms (acyclovir, valacyclovir).
For specific keratitis - tuberculous, syphilitic, etc. – a specialized specialist (TB doctor, dermatovenerologist, infectious disease specialist) is involved in the treatment.
In severe cases of corneal ulceration, microsurgical techniques are used: the edges and bottom of the ulcer are cauterized with a laser, or thermocoagulation is performed, or cryoapplication with liquid nitrogen is performed.
Special tests and special symptoms
Description
Sometimes it happens that a routine eye test reveals or suggests some problem that requires further analysis and additional testing, or the patient may themselves complain about some of the things we will touch on below.
The ophthalmologist must conduct an examination in order to subsequently refer the patient to one or another specialist to make a more accurate diagnosis and/or prescribe appropriate treatment. "Dry Eye"
Under normal conditions, the surface of the eye is covered with a thin film of tears. This three-layer film is extremely important for the eye to perform its functions and maintain the cornea in working condition (Fig. 24).
Since blood does not flow directly into the cornea, these superficial cells maintain their metabolism by obtaining oxygen and nutrients and get rid of their waste products through tears (if there are no tears at all, the transparent cornea will become opaque to light, which in turn will lead to blindness ). With each blink, tear components produced by the lacrimal gland and other glands wash the surface of the cornea. If the production of tears for one reason or another decreases, then dryness and burning in the eyes will cause you great inconvenience.
This problem occurs quite often, and therefore we will examine these circumstances in more detail. The tear film consists of three layers. The outer one, formed by lipids (components of fatty acids), keeps the middle aqueous layer from evaporating too quickly. The inner mucin layer controls the degree of hydration of the cornea (see Fig. 24). If the aqueous layer evaporates too quickly, the higher concentration of salts begins to irritate the eye and cause a burning sensation.
For many people, these symptoms appear in dry, cold weather, when this dryness is further aggravated by heating appliances. In summer, a similar effect can be caused by air conditioners. Many are affected by other environmental factors, such as dry climate, smoky rooms, strong winds and smog.
Sometimes the effects of the medications you take can also affect you. Some antihistamines and decongestants dry out not only the nasal mucosa, but also the eyes. Other medications can also reduce the release of moisture: diazepam (sedative), atenolol (for high blood pressure). As you age, the amount of tears you produce naturally decreases. Also, some diseases, such as Sjögren's syndrome, a systemic disorder that often accompanies rheumatoid arthritis, can cause both dry eyes and dry mouth.
Dry eyes are quite common among contact lens wearers, especially the soft type.
The severity of this problem can be assessed using various tests. Most often, a few drops of colored liquid are dropped into the eyes - this is done to study how quickly the surface layer of moisture evaporates. Another test uses a special dye (Rose Bengal) to stain dry, dead cells. These tests do not cause any particular inconvenience to the patient.
Dry eyes also occur when tears are produced normally, but the blink reflex is impaired or does not work at all. Also, which is quite rare, the patient sometimes does not completely close his eyelids during sleep. Normal blinking may also be impaired if the eyelids are damaged or burned. The exposed cornea in these cases can dry out, which leads to serious consequences. In mild cases of dry eye, artificial tears or ointments may provide relief, but in severe cases, it may be necessary to block the tear duct in the lower eyelid to retain all available moisture, or use soft therapeutic contact lenses to protect the cornea.
"Wet Eye"
This phenomenon may seem exactly the opposite of dry eye, but in reality it is sometimes just a reaction to dryness. As a rule, older people suffer from this, and the doctor must distinguish between the “feeling” that the eye is watering and real tears flowing down the cheeks. To check whether the cause of the disorder is a clogged tear duct, a few drops of colored liquid are instilled into the eye. After a couple of minutes, the patient blows his nose, and the resulting material is examined for the content of a colored substance. Clogged tear ducts can be cleared quite easily.
Decreased corneal sensitivity
The next time something gets into your eye, don't complain about the pain and streams of tears. Be grateful that your eye reacts exactly as it should. Pain, of course, is a warning signal that something is bothering the cornea, and excessive lacrimation is an attempt by the body to wash away the foreign particle.
In rare cases, the cornea may lose its sensitivity. If you don't feel any foreign body rubbing against your cornea, it can cause serious damage to your vision. It is quite easy to check the sensitivity of the cornea using a small piece of cotton wool or any other instrument. Complete loss of sensation indicates a serious neurological problem, but this should not be confused with a gradual decrease in sensitivity as a result of aging.
Increased eye height, or “bulging eyes”
This does not apply to people with naturally large eyes; This section addresses cases where one or both eyes seem to become
more. In fact, this does not mean that they have enlarged, but rather that they are beginning to protrude (exophthalmos). If both eyes bulge somewhat, an overactive thyroid gland is most often responsible for this.
If only one eye protrudes, then the possibility of hemorrhage, inflammation or the presence of a tumor should be taken into account, with which something needs to be done urgently. Often this protrusion can be very slight, so special instruments must be used to measure it and compare both eyes.
Ghosting pictures
If you've ever experienced double vision—from fatigue, after taking medication, or after drinking too much—then you know how disgusting it is. Sudden double vision for no apparent reason is a rather serious symptom. Whatever the reason, this indicates that the eyes are not able to look at the same point.
When you are tired or use drugs (including alcohol), the brain's ability to control and control the eye muscles is temporarily impaired. In such cases, simply resting or eliminating exposure to the relevant chemicals is usually sufficient.
Much more serious is the sudden onset of double vision, which is observed constantly. The typical cause of this is a small stroke or hemorrhage, or less commonly a brain tumor. In most cases, proper treatment of the cause of this double vision will slowly but surely restore its sharpness. As a temporary measure, you can use special prismatic glasses.
Visual field impairment
Normal vision is the result of two interconnected systems: accurate and sharp vision when looking directly at a given object and a general understanding of the background around you. To make this clearer, let's do a little experiment: look into the distance, extend your arms out to the sides at shoulder level, and wiggle your fingers. If you have good peripheral vision, you will notice your fingers moving (this also confirms that at the limit of the visual field, movement is the main factor of perception).
If you lose either central or peripheral vision, you may be legally blind. You may think that having only sharp central vision is enough, but this is not true. Why? Roll two pieces of paper into tubes and apply them to your eyes. Yes, you can watch TV and read, but try walking in an unfamiliar environment or going down the stairs. Without peripheral vision, it is completely impossible to drive a car even with the minimum level of safety. Conversely, if you lose central vision, you may be able to walk, but you will not be able to read or recognize the faces of others.
Central and peripheral vision can be affected by various diseases. A classic example of limited peripheral vision is glaucoma, in which the field of vision gradually narrows down to a narrow central area.
More often it happens that peripheral vision is not completely lost, but only a certain area of it. Usually a person does not even realize this, since this area is captured by the field of vision of the second eye. However, if it is located on the outside or below, then sometimes you will suddenly start to stumble upon unnoticed
obstacles for you. Loss of vision in such areas can be caused by aneurysms, bleeding, tumors, and so on.
The visual field is checked using special computerized devices in which small points of light flash against a dark background. The computer records the location and size of the area that is not in the field of view and produces a printout for subsequent analysis (Fig. 25).
Amsler Grid
As the name suggests, a grid of fine lines is used to detect small changes and distortions in vision. If you look at its center with each eye in turn, it may turn out that you will not see some lines or they will not seem clear enough to you (Fig. 26).
The reason for this may be retinal detachment, hemorrhage or some other disease. Quite often, an Amsler grid is given to the patient at home so that he can monitor changes in his vision.
Vision contrast
The ability to distinguish an object in low light or against a background of similar color depends on the eye's sensitivity to subtle changes in contrast. The visual system has several subsystems (channels), each of which is “tuned” to perceive certain levels of contrast. A typical visual acuity test uses high-contrast letters and is of little use for detecting problems that may occur in lower-contrast channels. This should be especially noted, especially since, after all, the main part of our visual load is not reading black letters on a white background at a distance of 5 meters.
There may be natural variations in contrast perception between individuals, but aging, eye diseases, diseases affecting the visual system, amblyopia, and the use of certain medications can all have negative effects on contrast vision.
Contrast vision is checked using a test that takes only a few minutes. This test can also be useful when prescribing new or tinted glasses or lenses: it can tell the doctor not to change lenses if this causes a decrease in contrast perception.
Checking color perception
Color vision is usually tested during a routine examination to identify any particularly severe problems in color perception. For professions that require increased sensitivity to color - such as an artist, art historian, set designer, decorator, fashion designer, etc. - or to identify a disease at an early stage, more sophisticated color perception tests are used.
In one such test, the task involves arranging circular colored disks into the correct sequence of shades. The most sophisticated test for color perception is using an anomaloscope: during this test, the subject is asked to mix primary green and red color sources so as to obtain a standard yellow color.
Electrodiagnostics of vision
Electrical impulses generated in the eyes and transmitted to the brain by the optic nerve can be measured using special sensitive instruments. Just like taking an electrocardiogram using an electrocardiograph, a device called an electroretinograph (ERG) gives us information about the functioning of the retina in patients with hereditary or acquired retinal damage.
The modern visual reaction speed test measures the electrical activity of the optic nerve along its entire length to the corresponding part of the cerebral cortex. In this case, electrodes are applied to certain points of the head, but this does not cause any inconvenience to the patient. During the examination, you can obtain data for each eye, assess potential visual acuity and objectively detect amblyopia. This procedure is especially useful when testing vision in young children or people with mental retardation, from whom it can be quite difficult to obtain relevant answers.
Ultrasound and echography
When the internal structures of the eye are difficult to see due to bleeding, clouding of the lens or cataracts, ultrasound is used to “see” what is happening inside. This procedure is completely painless; it measures the echo returned from the ultrasonic waves and analyzes the condition of the structures to identify scars, tumors, detachments, the presence of foreign bodies, and so on. Ultrasound is most often used to measure the size and location of individual structures of the eye before cataract surgery and to calculate the refractive power of the implanted lens.
Angiography of blood vessels
This test is designed to evaluate the blood supply to the retina and the choroid located on its inner surface, as well as to detect tumors. A special fluorescent substance, visible under ultraviolet light, is injected into a vein and quickly enters the retinal vessels. Every few seconds, photographs are taken through a special blue filter, which can help identify ruptures, blockages and/or the formation of new blood vessels. Because there is an unlikely but serious health hazard from injecting a fluorescent substance, this procedure is used only when the information cannot be obtained by other means.
Gonioscopy
A gonioscope is essentially a contact lens equipped with small mirrors to examine the angle between the cornea and iris. The information it provides can help differentiate between open- and closed-angle glaucoma, detect tumors or lesions, recognize injuries that cause tearing, and evaluate the effectiveness of laser treatment.
Interferometry
If you have a dense cataract, it is very important to assess what level of vision can be expected after its removal. Because cataracts obstruct the view of the inside of the eye, the doctor may not be aware that there is any other damage to the retina. In this case, after cataract removal, the patient may experience serious disappointment - because his vision will hardly improve.
A device called an interferometer sends an intense beam of coherent light (often a laser) into the eye. It is also used to predict the level of vision after treatment of amblyopia.
Measuring dark adaptation
Cataracts or other eye diseases often cause increased sensitivity to brightness because the beam of light entering the eye is narrowed. If the light source is bright enough, your vision will be impaired. For example, in normal lighting a person may have fairly good vision (0.6-0.7), but in very bright light his vision is assessed as only 0.1. A device for measuring dark adaptation (adaptometer) provides information about those levels of brightness (gloss) at which a person is no longer able to see, thereby allowing him to determine whether certain darkened lenses will help him. This device is also used to measure the time it takes for vision to recover after shining a very bright light on the retina. A similar phenomenon is often observed when moving to a dark place after being in a sunlit space or when the driver is temporarily “blinded” at night by the headlights of an oncoming car. Although the time for such vision recovery usually increases with age, delays and slow recovery can also be caused by certain diseases or vitamin deficiencies.
X-ray, computed tomography and nuclear magnetic resonance method
Suspected fractures or cracks in any of the bones that form the eye socket may require x-rays. For complex injuries involving muscle entrapment, computed tomography can facilitate diagnosis to localize foreign bodies and examine possible tumors. Nuclear magnetic resonance studies are more often used to diagnose soft tissue diseases; this method should not be used in the presence of foreign metallic bodies.
Cell counting
A crucial role in maintaining the transparency and overall health of the cornea is played by its inner layer, called the endothelium (posterior epithelium).
.
Unlike the outer layer, the epithelium
, the endothelium does not replace damaged cells by generating new ones. The remaining cells increase in size and fill the entire space (those who wear long-term contact lenses will likely experience these changes in cell shape).
Before cataract removal or corneal surgery, a device is often used to assess the quantity and quality of these cells. Since many of them will be removed during surgery, this preliminary assessment helps assess the risk and likelihood of success of the operation.
Study of the thickness of the cornea and anterior chamber of the eye
There are times when it is important to know the thickness of the cornea and the depth of the anterior chamber of the eye. This is done using an instrument called a pachymeter, which is attached to a slit lamp biomicroscope. It can be very useful in measuring the thinning or thickening of the cornea after prolonged contact lens wear.
Ophthalmodynamometer
This instrument is specifically designed to measure systolic and diastolic blood pressure in the retinal arterial vessels. It can often detect an increase in intracranial pressure before other symptoms appear (this device is now being replaced by more modern and sensitive methods).
Article from the book: Vision, glasses and contact lenses | Solomon G., Zinn W..
Outcomes of corneal inflammation
With a mild course of keratitis and superficial occurrence of foci of inflammation, recovery is complete, the cornea restores transparency.
In severe cases, deep infiltrates or ulcerations form, which later, scarring, leave persistent opacities. When the defect is centrally located, a persistent decrease in visual acuity occurs, which entails the need for keratoplasty.
The formation of a corneal ulcer can result in scarring or, in especially severe cases, a breakthrough into the anterior chamber - perforation.
Penetration of the inflammatory mass into the eye cavity through a corneal defect causes active intraocular inflammation, which can result in endophthalmitis and the need for enucleation - removal of the eyeball. Make an appointment
FAQ
How does the virus spread?
The spread of herpetic keratitis usually occurs through direct contact between an active herpetic lesion in any other part of the body and the eyes . To prevent this, you must strictly maintain contact lens hygiene; if you suffer from herpetic keratitis in one eye, do not spread it to the other.
Other measures to prevent herpetic keratitis and its relapses are :
• Avoid touching your eyes if you have a cold or inflammation in another part of the body.
• Do not wear contact lenses if you have active ocular herpes.
• Do not use cortisone ophthalmic drops if you have an active herpes infection, as this may allow the virus to multiply and, in the case of a previous herpes infection, may contribute to a new outbreak.
Possible complications
Complications of keratitis:
• Inflammation and damage to the cornea, which can leave scars on the cornea
• Corneal ulcers with risk of bacterial infection
• Chronic or recurrent viral infections of the cornea
• Chronic inflammation of the cornea
• Temporary (due to inflammation during active infection) or permanent (due to residual scar) loss of vision.
How long does it take to treat the disease?
The duration of herpetic keratitis will depend on the size, depth and cause of it . Eye ointments or oral antiviral medications commonly used to treat herpetic keratitis are prescribed by an ophthalmologist.
Despite this, the infectious period lasts from 7 to 10 days . After this period, corneal damage and inflammation persist until tissue regeneration begins. It may be complete and without complications in cases of superficial epithelial infection or with consequences due to residual scar in cases of stromal lesions.
Are people who wear contact lenses more likely to develop this type of condition?
Yes, people who wear contact lenses are 6 times more likely to develop herpetic keratitis, especially if they wear them for many hours a day or at night, as this causes small epithelial wounds through which the herpes virus can enter. This is why it is very important to practice good hand hygiene (especially if you have an active herpes infection in another part of the body), use lens cleaning and preservative solutions correctly, do not overuse contact lenses, do not swim with them, and remove them if you notice any discomfort.
Can the infection come back?
Although precautions are taken, it is very common for herpetic keratitis to reactivate due to the following factors:
• Stress
• Ultraviolet radiation
• Injuries or bruises on the body
• Use of certain medications
• Menstruation
• Instilling some eye drops
Patients with immunodeficiency or atopy are more prone to recurrent or refractory herpetic keratitis. Relapse occurs due to the fact that the herpes viral infection affects a large part of the population (the first infection can appear in early childhood, even in the form of a cold). After the first infection, which never goes away, but our immune system controls it and blocks the virus in the lymph nodes of the body. In the previously mentioned situations, when a certain immunosuppression occurs, the virus takes the opportunity to leave the ganglion and affect some parts of the body, mainly the lips.
Diagnostics
The diagnosis is made after examination.
- The doctor checks visual acuity: for this he uses tables.
- The fundus is examined: an ophthalmic lamp is used.
- The ophthalmologist finds out the patient’s complaints (collects anamnesis).
- Examines the cornea using dye.
A biopsy may be ordered to confirm the diagnosis. During the procedure, the cause of the pathological process is determined. The patient must report previous illnesses, including viral ones. It is possible that the cause of marginal keratitis is an eye injury: you should inform your doctor if this has occurred. The above methods are effective, but the ophthalmologist may prescribe bacteriological culture. In this case, the layers of the cornea are examined.
Prevention
The disease may recur. To avoid such a problem, you need to follow basic rules.
- Don't forget about eye hygiene, especially when wearing contact lenses.
- Protect your eyes from sunlight.
- When in hazardous work, wear safety glasses.
- Strengthen your immune system.
- Treat diseases in a timely manner.
Welding eye drops
Allergy eye drops are presented in this article.
All about Quinax eye drops https://eyesdocs.ru/medicinaoperacii/lekarstva/kapli-dlya-glaz-kvinaks-osobennosti-primeneniya-preparata.html
Causes
The disease is based on an inadequate response of the immune system to familiar, harmless things. When confronted with them, the body produces specific antibodies that act on mast cells and various inflammatory mediators. As a result, a whole complex of antigen-antibody reactions is activated.
The following main causes of allergic keratitis can be identified:
- pollen of grasses, trees;
- wool, saliva, particles of animal epithelium;
- food products, preservatives, emulsifiers, dyes;
- medicines;
- tobacco smoke, dust, harmful industrial impurities;
- cosmetical tools;
- household chemicals.
The causative factor can be any substance. Internal causes are also possible, such as various infections, bacteria and parasites, which have a toxic toxic effect on the body.
Treatment of the disease
Treatment is most often carried out in an inpatient setting. Drug treatment is selected in accordance with the form and cause of the disease. Viral keratitis is mainly treated with antiviral drugs, most often immunoglobulin (dropped into the eye) and immunomodulators (taken orally).
If keratitis was caused by herpes, then under no circumstances should corticosteroids be used, they can cause extremely serious complications. If the case is advanced, the patient is recommended to undergo a corneal transplant. To prevent recurrence of the disease, an antiherpetic vaccine is administered.
Symptoms of the disease
If keratitis is bacterial in nature, then treatment is based on broad-spectrum antibiotics, as well as antibacterial ointments. In this case, surgical intervention is performed if necessary.
In the treatment of keratitis the following are used:
- antiseptic solutions;
- novocaine blockades;
- drugs and agents that promote epithelization of ulcerative formations;
- biogenic stimulants;
- keratoplasty.
Marginal keratitis
As for prognoses, a positive process and the absence of relapses are determined by the following:
- the nature of the infiltrate;
- the area of his education;
- complications of various etiologies.
Provided that medical care was provided competently and in a timely manner, the infiltrates that were on the surface disappear completely. It is important to know that if keratitis has developed deep in the tissues of the cornea, then vision can decrease greatly, even complete loss is possible.
ethnoscience
Keratitis is very widely treated with traditional medicine. The most common ones are listed below:
- Sea buckthorn oil will help with light intolerance and soothe pain. First, 1 drop is instilled every hour, then (after a couple of days) the interval is increased to 3 hours. Using this remedy, you can feel noticeable relief even in advanced cases.
- If there is suppuration, then 2 drops of celandine juice (freshly squeezed) are instilled before bedtime, it is diluted with aqueous propolis extract in the ratio of 1 part juice to 3 parts propolis extract. If irritation occurs, the propolis extract must be increased.
- Clay lotions that are applied to the eyes, forehead and back of the head help a lot. To do this, put a 3 cm layer of clay in a napkin. The clay should be soft, not flowing, smooth and dense. Such compresses should be kept for about an hour or two. It is recommended to do 2-3 lotions per day.
- The juice from an aloe plant that is more than 3 years old must first be kept in the refrigerator for 10 days, then strained and diluted with mumiyo (about the size of a match head). Instill 1 drop of the resulting mixture once a day into one or both eyes. After a month, you can no longer add mumiyo, but only drip juice.
- In freshly baked rye bread you need to make a depression in which you need to place the glass upside down. Drops will form on the walls of the glass, which must be carefully collected and dripped 2-3 drops into both eyes once a day.
Additional symptoms of keratitis