The individual therapeutic strategy chosen by the ophthalmologist in the treatment of strabismus in adults depends on many anamnestic and clinical factors: heredity, age, lifestyle of the patient, etiological reasons and background for the development of strabismus, severity of pathology, etc. The most common methods are direct occlusion (wearing glasses with an opaque glass on the healthy eye, which “makes” the squinting eye work); long courses of exercises and/or instrumental training in order to strengthen the oculomotor muscular system; in some cases - surgical intervention as one of the stages of correction.
Occluders (in most cases, ordinary glasses with sealed glass) are prescribed mainly to children, but can also be used in the treatment of mature patients. The essence of this method is to exclude from the processes of visual perception not the squinting eye (as the central nervous system instinctively does), but the healthy one. In this case, the body has no choice but to use the abnormal visual organ; with long-term and correct application of the method, dynamically controlled by a doctor, the effect of constant training is triggered, and the functional status of the squinting eye is gradually restored. Treatment with an occluder should, however, be started before the formation of amblyopia (loss of visual functions of the squinting eye due to its long-term inactivity).
The essence of the disease
In this article
- The essence of the disease
- Classification
- Causes of development of divergent strabismus in children
- Divergent concomitant strabismus: causes of development in a child
- Symptoms
- Divergent concomitant strabismus in children: treatment
- Medicinal and surgical methods and means of treatment
- Possible complications
The disease disrupts the synchronicity of the location of the eyeballs in attempts to examine a specific object. At the same time, the eyes deviate in different directions; one eye or both can squint.
Children may experience delays in mental or physical development. In addition, this is also a visible defect, which can cause tightness and complexities. Strabismus can lead to complications, so you should not hope that it will go away on its own; at the first signs, you should immediately begin treatment.
What is strabismus?
Strabismus is another name for the condition that precedes strabismus. The condition is a lack of coherence in the activity of the muscle tissue of the eyes. Most often, the condition begins in early childhood, when both eyes function differently. In the absence of timely treatment, progressive strabismus develops. In rare cases, strabismus is diagnosed in newborns.
REFERENCE! Divergent strabismus is characterized by the divergence of the eyes from the midline towards the temples. This strabismus may spread to one or both eyes.
Useful video
Exotropia:
Classification
Strabismus (strabismus) is a condition in which the eyes “look” at the temples.
Divergent strabismus in children has the following forms:
- Permanent strabismus - with it, the position of the eyeballs remains unchanged.
- Periodic strabismus - it is noticeable only under certain conditions.
The permanent form of strabismus also has its own types:
- Congenital strabismus - occurs as a result of birth trauma, intrauterine infection, etc. Newborn babies are unable to focus on one point; with their eyes wide open, “floating” apples can create the impression that there is strabismus. It is necessary to distinguish the false form from the real strabismus in time.
- Sensory strabismus - in this case, one eye sees worse. The development of such strabismus is possible with cataracts and other types of clouding of the eyes. In this case, the eye that sits worse ceases to take part in the process of vision, and the balance in the work of the motor muscles is disturbed.
- Secondary strabismus can occur when correction of the length of the motor muscles is unsuccessful. This operation is performed for primary strabismus.
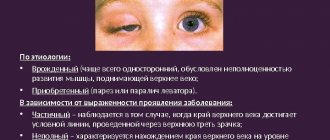
Also, concomitant divergent strabismus is classified according to the side of the lesion:
- monolateral - when one eye squints;
- alternating - there is an alternating deviation of the eyeballs from the correct position.
According to the time of development of pathology, they are distinguished:
- congenital concomitant strabismus - manifests itself in the neonatal period;
- acquired - stems from another disease.
The latter is also divided into several types:
- Constant squint.
- Temporary concomitant strabismus - appears while the eyes are resting without any special symptoms.
- Sensory: with such divergent strabismus, both or one of the child’s eyes begin to look in the wrong direction at the time of the development of the disease, during a period of fatigue, or a long stay in the open sun.
With strabismus, the child's eyes may lose clarity, and diplopia sometimes develops. If an eye with amblyopia begins to squint towards the temples, then we can say that a divergent sensory strabismus has occurred in the child. It is important to begin treatment as soon as possible.
Diagnostics
External deviation is obvious. Exotropia should not be confused with transient outward wandering of the eyes, which occurs in approximately 60–70% of normal newborns and resolves by 6 months of age.
Diagnosis of divergent strabismus consists of a series of tests:
- Measurement of visual acuity - may be normal or abnormal. The reduction may be caused by refractive error, pathology such as cataracts or retinal disorders, suppression, or a combination of these factors. Measuring visual acuity in young children is more challenging. For this, there are special circuits and devices that require a lot of patience.
- Cycloplegic refraction. This is an objective determination of the true refractive error by eliminating the effect of accommodation. Achieved by paralyzing the ciliary muscle with cyclopentolate eye drops or atropine eye ointment. Medicines also cause pupil dilation.
- Slit Lamp Test – This test checks for any disease or abnormality in the front of the eye.
- Examination of the fundus (retina) - fundoscopy - is used to examine the inside of the eye, involving the retina, optic nerve, blood vessels and allows you to measure the magnitude of the deviation, evaluate eye movements in different directions of gaze, check for the presence of diplopia, if present, determine the type, degree binocular vision.
Causes of development of divergent strabismus in children
With heteropia, the visual axis of one eye of the child deviates from the point of fixation. The visually received information is not combined, which is why the central nervous system blocks the image transmitted by the defective eye. If treatment is ignored, vision will deteriorate because the diseased eye does not perform its functions.
Strabismus in children occurs due to a defect in the eye muscles, which are necessary for the movement of the eyeball. There are many reasons for this defect in children, and they can be both congenital and acquired.
Among them:
- decreased visual acuity;
- eye damage as a result of injury;
- paralysis and paresis;
- pathological processes in the nervous system;
- stress;
- fright;
- infectious diseases.
Congenital strabismus in children is quite rare.
If the disease manifests itself in the first six months of a child’s life, then it is classified as infantile strabismus. Among the reasons for its manifestation:
- Crouzon and Down syndromes, which are genetic;
- hereditary causes;
- premature birth;
- intrauterine exposure to drugs and medications;
- cerebral palsy;
- congenital eye defects.
Heterotropia occurs in a small number of children, approximately 3%. As a rule, it manifests itself at 2-3 years: it is at this age that the ability to perceive images with both eyes at the same time is formed.
If treatment is not started, strabismus can lead to worsening vision (observed in 50% of such children). In addition, strabismus adversely affects the mental state. Also, strabismus in a child largely determines the scope of professional activity in the future: the list of professions for people with this pathology is quite narrow.
Heterotropia can also develop in adults. In this case, it occurs as a result of diseases leading to a sharp decrease in visual acuity, for example:
- leukomas;
- cataracts;
- retinal detachment;
- pathologies of the optic nerve.
Paralytic divergent strabismus in children develops due to the occurrence of traumatic brain injuries, cranial nerve palsies, tumors, fractures in different areas of the orbit, strokes, etc.
Divergent concomitant strabismus in children: treatment
Divergent strabismus in children is diagnosed without special equipment. Pathology can be determined even visually.
For treatment the following is prescribed:
- glasses or soft contact lenses;
- hardware treatment;
- therapy that helps to gain and consolidate binocular vision;
- surgical intervention.
Glasses help correct refractive errors. With their help, deviation is reduced and accommodation and convergence are stimulated. Sometimes wearing glasses is enough to completely get rid of divergent strabismus.
Also, during treatment, the use of special bandages is often required to cover the healthy eye.
On average, treatment lasts 2-3 years and is performed in several stages.
It is important that treatment of divergent strabismus in children continues not only in the hospital, but also at home. You must carefully follow all the doctors’ instructions and do not ignore the prescribed exercises.
At the first stage, a specialist may prescribe the use of traditional medicine. They help strengthen the eye muscles, stop the progression of the disease, and in some cases even avoid surgery.
Among such remedies is taking decoctions of cabbage leaves, pine needles, and rose hips. It is important that all this is prescribed by a doctor: you should not self-medicate.
It is often recommended to send your child to specialized kindergartens. In such institutions, everything is aimed at correcting the defect. In addition, the child is much more comfortable being around children with a similar defect, especially when he needs to wear a bandage.
If it is not possible to send the child to a specialized institution, eye exercises should be done at home. You can teach your baby to do it independently: move his eyes to the sides, rotate them, squeeze and unclench his eyelids. Classes must be regular.
Medicinal treatments
Today, there are no medicinal ways to get rid of divergent strabismus in children. Typically, drugs are prescribed as adjuncts that help maintain health and get rid of a number of symptoms. The effect is enhanced by a therapeutic diet, which is full of vitamins and microelements necessary for the proper functioning of the visual apparatus.
Surgical methods for treating strabismus
Usually surgery is prescribed if other methods of eliminating the pathology do not work. Its essence is the correction of damaged muscles. Most often, the operation is performed on preschool children if strabismus is congenital. The optimal age is 4-5 years.
Before the operation, the ophthalmologist conducts a sensory-motor examination, during which all variants of eye position, the angle of divergence of the axes, and possible movements of the visual organs are identified.
Sometimes it makes sense to have surgery on both eyes, even if one eye is squinting. The correction is carried out under general anesthesia. During the operation, a micro-incision is made through the conjunctiva. Through the opened access to the muscle, it is relaxed, strengthened or displaced. The operation takes no more than two hours.
Prevention
Prevention is important primarily for children whose family has a history of strabismus or other ophthalmological problems. It consists of the following steps:
- Regular visits to the ophthalmologist.
- Timely optical correction of ametropia.
- You should definitely pay attention to visual hygiene.
- Load your eyes in dosed form.
- Conduct timely treatment of eye injuries and infectious diseases.
- Prevent skull injuries.
- Pregnant women should be attentive to their health.