Ophthalmoscopy is a diagnosis of the fundus of the eyeball, an overview of the internal structures of the visual organs from the inside. The procedure is carried out using ophthalmoscopic equipment. Diagnostics allows you to examine in detail the retina, the condition of the optic nerve, and the vascular network. In modern ophthalmology, fundus examination is carried out in two ways - direct and reverse. Let's consider both methods in detail.
What is direct ophthalmoscopy
Fundus examination is performed in an ophthalmology office. This is most often done using an ophthalmoscope, or at the slit lamp using a non-contact/contact diagnostic ophthalmoscopic lens. The lens resembles a magnifying glass. The ophthalmoscope illuminates the eyeball with a beam of light that penetrates the entire eyeball, allowing for a thorough examination. The light reaches the retina, optic nerve, macula and small blood vessels.
In some cases, it is necessary to instill eye drops to dilate the pupils. This will allow light to penetrate more accurately, as the pupil is the eye's natural shield and makes access more difficult.
It's a good idea to go to the test with a loved one because the drops temporarily impair vision. After instillation, it will be impossible to perform activities that require good vision, such as driving for adults or school duties for children, for approximately 3-4 hours.
Fundus ophthalmoscopy is performed every 5 years until age 40 and every 1-2 years after age 40. People with diabetes and other vascular diseases should be tested more often, at least once a year if there are no complaints and immediately if there is any decrease in vision.
OPHTHALMOSCOPE PROCEDURE
No preparation is required for ophthalmoscopy. But for the most thorough examination of the periphery of the fundus, preliminary dilation of the pupil is required, which is achieved by instilling a 1% tropicamide solution 15-20 minutes before the examination. The ophthalmoscopy procedure takes on average 10-15 minutes. It should be noted that during the examination, the patient may experience some discomfort in the eyes due to the bright light from the ophthalmoscope, and immediately after the examination, the patient may see various spots before the eyes for some time. If the patient’s pupil has been dilated, then he should not drive for 2-3 hours after the examination; in addition, when going outside, it is advisable for such a person to wear sunglasses, because a dilated pupil causes discomfort when looking at light. If you are allergic to anesthetics or other medications, you should tell your doctor about it.
What does fundus ophthalmoscopy reveal?
In the part of the eye that is invisible to us, an ophthalmologist can see many diseases, both visual and systemic:
- Optic nerve diseases such as glaucoma, optic atrophy and neurological disorders;
- Retinal diseases that cause decreased central vision and damage to the macula, such as age-related macular degeneration;
- A brain tumor that increases intracranial pressure, leading to swelling of the optic disc, visible under ophthalmoscopy;
- Diseases of the blood and blood vessels - anemia, hypertension, atherosclerosis, thrombosis, diabetes and leukemia. An ophthalmologist, based on the condition of the fundus vessels, can initially assess the extent of the disease.
- Pathology of the peripheral parts of the retina, such as peripheral breaks and dystrophies.
Indications for diagnosis
In what cases is fundus ophthalmoscopy prescribed? You need to be examined regularly to prevent eye diseases. Also, by examining the visual centers, you can see pathologies of internal organs - hypertension, diabetes, tuberculosis, kidney diseases, etc.
Important! Ophthalmoscopy allows you to identify hidden ailments of organs throughout the body.
A referral for diagnostics can be issued not only by an ophthalmologist, but also by a cardiologist, infectious disease specialist, gynecologist and other doctors. This is due to the fact that diseases of one organ can affect the patient’s entire body. Kidney diseases can affect the health of the visual organs, problems with the heart and metabolism too.
Osteochondrosis of the cervical spine can negatively affect the condition of the optic nerve and retinal vessels, so a neurologist can prescribe a referral for examination. An angioneurologist prescribes diagnostics in case of increased intracranial pressure.
Note! Fundus ophthalmoscopy is very important for pregnant women, as it helps identify the risk of retinal detachment during childbirth.
Therapists and cardiologists, using eye mirror diagnostics, can distinguish between hypertension and atherosclerosis, so do not be surprised by a referral for a fundus examination.
This procedure is also important for endocrinologists. In the case of diabetes mellitus, the course of the pathology is determined by the vascular pattern.
Indications for diagnosis:
- headache;
- violation of movement coordination;
- myopia or color blindness;
- inflammatory processes of the eyes;
- epilepsy or seizure disorder;
- traumatic brain injuries.
Also, a referral for diagnostics is received after taking certain medications.
Contraindications include the following:
- photophobia;
- lacrimation;
- narrowness of the pupil;
- pupil pathology;
- cardiovascular diseases;
- clouding of the optical media of the eyeball.
Patients with glaucoma can also be diagnosed with pupil dilation and given short-acting medications. To prevent increased eye pressure, special medications are given. Immediately after the procedure, medications are administered to constrict the pupil.
Direct diagnosis is carried out in cases of existing pathology of the visual organs; it is characterized by greater detail and clarity. Indirect diagnostics are carried out for a general examination of the patient to identify pathologies.
Possible complications:
- allergy to eye drops;
- nausea with vomiting;
- dizziness;
- attack of glaucoma.
Ophthalmoscopy is not considered dangerous to the visual organs, however, a visit to the ophthalmologist after diagnosis is still advisable.
Fundus examination in a child
Fundus examination in children is one of the main ophthalmological tests. It is especially recommended for children with visual impairments, strabismus, and those with a family history of eye or brain tumors. Ophthalmoscopy should be performed on premature infants in the first month of life to rule out retinopathy of prematurity. This is retinal damage that affects low birth weight children.
The examination is safe and painless. However, its duration can reach up to an hour.
Ophthalmoscopy - why does pregnant women need it?
Since pregnant women are at risk, they must follow all the specialist’s recommendations and visit the clinic in a timely manner to receive consultations with an ophthalmologist.
Statistics show that the risk of retinal detachment during natural childbirth increases significantly. For this reason, the obstetrician-gynecologist refers pregnant women to qualified doctors who, after making a diagnosis, will be able to select effective and safe treatment.
For whatever reason you need to undergo an ophthalmoscopy, this can be done quickly and efficiently at the Optic Center clinic.
What is direct ophthalmoscopy?
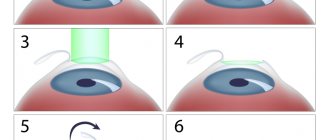
Direct ophthalmoscopy is performed using a special ophthalmoscope device, which the ophthalmologist brings close to the eye, but does not touch it. The light of the ophthalmoscope is sequentially focused on the vitreous body, the optic nerve head, blood vessels, the central zone of the retina - the macula, and the peripheral zone of the retina. The ophthalmoscope also has built-in filters to reduce light intensity, color filters:
- green – facilitates observation of nerve fibers and thin vessels of the retina;
- blue – helps when testing with fluorescein.
The resulting fundus image is simple and significantly enlarged.
Types of ophthalmoscopy
Ophthalmoscopy is divided into two types: direct and indirect (reverse). Both methods complement each other, and each of them can be chosen depending on the task assigned to the study. With indirect ophthalmoscopy, the image is inverted, but this method provides a wider view of all areas of the fundus. The method of direct ophthalmoscopy allows us to examine in more detail the areas with identified pathology under significant magnification.
A valuable additional method for studying the details of the fundus is ophthalmochromoscopy according to Vodovozov, using light filters. It allows you to identify the smallest pathological changes that are invisible during normal examination.
The most modern and high-tech method is scanning laser ophthalmoscopy, which allows examination even in cases where the transparency of the lens and vitreous body is reduced. The method is based on illuminating the retina with a laser beam and studying its reflection through the entire pupil. In this case, the image is displayed on the screen with the possibility of video recording. The disadvantages of this method are the inability to obtain stereoscopic and color images, as well as the high cost.
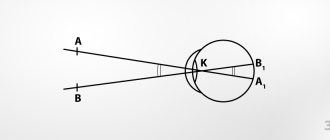
What is indirect ophthalmoscopy?
The examination is carried out in a slit lamp (biomicroscope) using either a focusing lens, which the doctor holds in front of the patient's eye under examination (non-contact), or a special triple Goldmann lens (a converging lens in the center, surrounded by three mirrors), which he places on the eye after local anesthesia with using a special protective gel. This method allows for a spatial (stereoscopic) view of the inside of the eye. Scattered light or light gap (narrow light beam) is used, which, thanks to the ability to adjust its height and width, improves the quality of viewing.
Using a Goldmann lens, the doctor can conduct a thorough examination of not only the central zone of the retina, but also its peripheral parts.
How is ophthalmoscopy performed?
The traditional technique is as follows: a mirror ophthalmoscope, which is most often used for examination, is a concave mirror with a hole in the center. To increase the visible area of the fundus, drops are sometimes placed into the patient's eye before the procedure to dilate the pupil. Using an ophthalmoscope, light from a nearby source is collected into a narrow beam and illuminates the fundus of the eye, which the doctor sees through a hole in the mirror.
Our center uses electronic ophthalmoscopes with built-in halogen light sources or fundus lenses, which allow the specialist to obtain a clearer image.
Indications for fundus examination:
- the occurrence of diseases during which changes in the fundus of the eye occur: arterial hypertension, diabetes, blood diseases (for example, leukemia, bleeding disorders, anemia), thrombosis and others;
- diseases of the central nervous system, with abnormal reaction of the pupils to light;
- the use of certain medications (for example, for cancer);
- head injuries;
- intracranial tumors;
- strabismus in children and adults;
- premature baby;
- imbalance;
- disturbances in color vision, visual acuity, defects in central or peripheral vision;
- after loss of consciousness;
- recurring headaches;
- imbalance;
- myopia more than 3.5 diopters;
- regular examinations every 2-3 years;
- flashes or floaters in the eye.
Services
Examination of the fundus of the eye (ophthalmoscopy) allows you to assess the condition of the retina, blood vessels, macula area, and optic nerve head.
TYPES OF OPHTHALMOSCOPE AT MY DOCTOR MEDICAL CENTER
- direct ophthalmoscopy – examination of the fundus using an ophthalmoscope (flashlight with multiple lenses) with 15x magnification
- reverse ophthalmoscopy - examination of the fundus of the eye in an inverted form using an ophthalmoscope (flashlight with several lenses) and two magnifying glasses with 2- or 3-fold magnification
- examination of the fundus with a Goldmann lens - examination of the fundus and anterior chamber of the eye in an inverted form using a lens with 3 mirrors and a slit lamp (a special microscope with built-in lighting)
SYMPTOMS THAT REQUIRE OPHTHALMOSCOPE
- floating opacities in the form of “flakes” and the appearance of a “dark curtain”
- distortion, blur, ghosting, blurred vision, deterioration of twilight vision, blurred vision, rapid decrease in visual acuity
- rapid eye fatigue, constant eye strain and, against this background, headaches, pain in the eye area
- sensitivity to bright light, decreased ability to distinguish colors, sometimes double vision in one eye when the other is closed
- difficulties when reading, the appearance of an opaque spot in the center of the visual field, distortion of the contours of objects, curvature of straight lines
INDICATIONS FOR FUNDUS EXAMINATION
- diseases of the retina and lens - retinal detachment, hemorrhage, changes in retinal vessels
- senile farsightedness (presbyopia)
- vascular atherosclerosis
- Amblyopia in children (decreased vision)
- eye injuries
- headaches of unknown etiology
- head injuries
HOW DIRECT OPHTHALMOSCOPE IS PERFORMED
Before the procedure, drops are instilled to dilate the pupil, which allows you to expand the visible area of the fundus. Ophthalmoscopy is performed in a dark room - the patient sits on a chair, the ophthalmologist is opposite him. The doctor illuminates the eye being examined with a beam of light from an ophthalmoscope. The distance between the ophthalmoscope and the eye should not be more than 4 cm.
During ophthalmoscopy, both of the patient's eyes are open. The patient is asked to look to the sides or to the tip of the nose, which allows a better view of the lens, vitreous body and fundus of the eye.
Duration – 5-10 minutes.
HOW IS REVERSE OPHTHALMOSCOPY PERFORMED?
Before the procedure, drops are instilled to dilate the pupil, which allows you to expand the visible area of the fundus. Ophthalmoscopy is performed in a dark room - the patient sits on a chair, the ophthalmologist is opposite him. The doctor illuminates the eye being examined with a beam of light from an ophthalmoscope and brings a biconvex magnifying glass to the eye. The distance between the magnifying glass and the eye should not be more than 7-8 cm.
During reverse ophthalmoscopy, both of the patient's eyes are open. The patient is asked to look to the sides or to the tip of the nose, which allows a better view of the lens, vitreous body and fundus of the eye.
HOW TO EXAMINATE THE EYE WITH A GOLDMAN LENS
Before the procedure, drops are instilled to dilate the pupil, which allows you to expand the visible area of the fundus. The patient's head is tightly fixed behind the slit lamp, with the chin on a special stand. The patient must sit upright during the entire procedure. The doctor places the lens on the surface of the eye, examines the fundus of the eye, rotating the lens 360⁰.
Duration – 10-15 minutes.
The effect of vasodilating drops ends in the evening. It is advisable to plan an ophthalmoscopy before the weekend; on the day of the procedure, refrain from driving a car, since the use of vasodilator drops contributes to a short-term decrease in visual acuity.
Thanks to the fundus examination, it is possible to:
- assessment of the progression of organ damage in patients with arterial hypertension and diabetes;
- retinal assessment – diagnosis of retinal detachment, Age-related macular degeneration (macular degeneration);
- optic disc assessment – glaucoma, papilledema may indicate neurological changes;
- vascular assessment;
- confirmation of the presence of atherosclerotic lesions or embolisms;
- Assessing the vitreous – for example, hemorrhage or opacities.
Examination of the fundus is necessary in the diagnosis of many diseases, including those that are initially asymptomatic and manifest only by changes in the fundus.
Contraindications
Inflammatory and infectious diseases in which lacrimation or photophobia are present make ophthalmoscopy difficult and completely exclude the use of contact ophthalmoscopic methods. Cardiovascular disease, which precludes the use of adrenergic agonists (pupil-dilating drops), as well as the inability to dilate the pupil with medications, are a contraindication to performing a fundus examination with a wide pupil. However, a “basic study” is possible with a small pupil. The use of ophthalmoscopy is not informative in case of pathological “sealed” pupil, which is called miosis. Insufficient transparency of the vitreous body and lens can also interfere with fundus examination.
Can everyone have an ophthalmoscopy?
Despite the safety and painlessness of ophthalmoscopy, it is not available to everyone. There are a number of contraindications. With the development of infectious and inflammatory ophthalmic pathologies, a fundus examination will most likely not be prescribed. Also, the procedure is temporarily not used to examine patients suffering from photosensitivity, lacrimation, miosis and diseases that lead to clouding of the lens and other optical media. Often, angle-closure glaucoma becomes an obstacle to ordering an examination. The examination may cause a sharp increase in pressure in the eyeball. In some cases, heart and vascular diseases also become the reason for searching for an alternative to ophthalmoscopy.
Ophthalmoscopy without artificial dilatation of the pupil
Description
A detailed examination of the fundus
is carried out only with a dilated pupil. It is often desirable to perform ophthalmoscopy without artificial dilatation of the pupil: this reduces the examination time, eliminates the patient’s temporary disability caused by impaired accommodation and photophobia that occurs during the administration of mydriatics, and makes the procedure less tiring for the patient and less labor-intensive for the doctor. This is especially important during preventive examinations.
Sometimes ophthalmoscopy with a narrow pupil is the only way to observe the fundus. The resolution in this case inevitably decreases, and it is almost impossible to see small details. The same difficulties as with a narrow pupil arise in cases where the central part of the cornea or lens is opaque.
Fundus examination is fundamentally feasible with a pupil diameter of 1.5–2 mm. Smaller pupil sizes do not provide any useful information. Fundus photography without pupil dilation presents even greater difficulties. Illumination and resolution with a narrow pupil.
During ophthalmoscopy with a narrow pupil, a decrease in image illumination, a decrease in resolution and an increase in corneal reflexes are noted.
In order for the entrance pupil of the ophthalmoscope and the image of the light source to be simultaneously placed on a narrow pupil without overlapping each other, the areas of the latter must be significantly reduced. So, if on a pupil dilated to a diameter of 5 mm, you can place an entrance pupil with a diameter of 2 mm (area 3.14 mm2) and an image of a light source with an area of about 15 mm2, then with a narrow pupil with a diameter of 2-2.5 mm, the diameter of the entrance pupil can be no more than 1 mm, and the area of the source image is no more than 5 mm2. As follows from the formula, the image illumination will decrease by more than 10 times. However, this is not the insurmountable obstacle; the decrease in illumination can be compensated by increasing the brightness B of the light source. With modern high-intensity light sources, the required level of illumination is quite achievable. The main limitations are imposed by the increasing influence of diffraction. It follows from the formula that when the diameter of the entrance pupil decreases from 2 to 1 mm, the theoretical resolution of ophthalmoscopy drops from 200 to 100 lines per 1 mm. Thus, with a patient’s pupil with a diameter of about 1 mm, it does not make sense to use ophthalmoscopes with a magnification of more than 15 times, since details smaller than 0.01 mm will still not be distinguishable. Finally, with a narrow pupil, additional difficulties arise in eliminating reflexes. Light reflexes.
To completely eliminate corneal reflexes, it is necessary to strictly separate the images of the light source and the exit pupil of the optical system on the pupil of the eye being examined. It should be taken into account that usually the source image consists of a central bright part and a blurred halo, which can cause quite bright reflections. With a sufficiently wide pupil, with a diameter of 4-5 mm or more, such separation is easy to achieve. In this case, it is possible to allow that the source image together with the halo does not lie close to the exit pupil. The zone formed between these two areas, which is not used for either illumination or observation, does not interfere with ophthalmoscopy. With a narrow pupil, the presence of such a “dead” zone leads to the fact that both areas cannot simultaneously fit into the pupil of the eye and ophthalmoscopy becomes impossible. Thus, with a narrow pupil, it is necessary to achieve particularly rational use of the pupil area. This requires greater than usual elimination of ghosting, which occurs partly as a result of aberrations of the optical system, partly as a result of reflection of light by the surfaces of lenses, metal frames, spacer tubes and other parts of the device.
Reflective prism shape.
When examining the fundus of eyes with a narrow pupil, modern hand-held ophthalmoscopes are used, in which the shape of the reflective prism has been changed. When designing a prism used in. In older models, its upper edge partially obscures from the observer the beams of rays emerging from the eye being examined. Only that part of the light flux that exits through the upper part of the wide pupil can enter the observer's eye. The light coming out through the area closely adjacent to the source image & does not reach the observer's eye. Thus, the input; the edge of the prism creates a “dead” zone. This form of prism does not allow ophthalmoscopy with a narrow pupil. In the latest models of hand-held ophthalmoscopes, for more rational use of the pupil area, the upper part of the reflective prism, which falls into the path of the lighting rays, is cut off. In this case, the zone of the cornea intended for observation is close to the image of the light source. These zones no longer extend beyond the narrow pupil. Ophthalmoscopy becomes available with a pupil with a diameter of 2.5-3 mm.
The use of mirrors in a narrow pupil ophthalmoscope.
Another design solution was used in the
Schepens binocular narrow pupil ophthalmoscope (L. Schepens)
.
This device, according to the company, allows for reverse ophthalmoscopy with a pupil diameter of about 1.5 mm. The Schepens ophthalmoscope
uses a mirror instead of a reflective prism. The same mirrors were introduced to project the device’s entrance pupils onto the cornea (two, since the device is binocular). Mirrors, just like in manual ophthalmoscopes, cut off part of the source image and part of the area of the entrance pupils. Despite the fact that most of the light flux is lost, the details of the fundus can still be seen.
Dilatation of the pupil in a non-medicinal way.
Another way to avoid drug dilation of the pupil during ophthalmoscopy and photography is a “bypass”.
The pupil is dilated using physiological rather than medicinal means. For this purpose, dark adaptation of the patient's eye is used. The method is proposed in a number of inventions, including domestic ones. The method received practical application in a camera for photographing the fundus of the eye (Japan).
The patient is placed in a darkened room, after 1-2 minutes his pupils dilate to a size sufficient for photography. In this condition, the eye is illuminated with low-intensity infrared rays, which the patient does not notice and which do not cause a pupillary dilation reaction. The infrared image of the fundus generated in the device is converted into a visible image using a television monitor. Based on the image obtained on the monitor screen, the area to be photographed is selected and focused. Photography is carried out in visible light using a conventional flash lamp. Due to the short duration of the flash, the pupil does not have time to contract. Immediately after the shooting, the patient can begin normal activities. However, this method is not always effective. For example, in elderly patients, pupil dilation in this way is usually not sufficient for photography. —
Article from the book: Optical instruments for eye research | Tamarova R.M.
Ophthalmochromoscopy
How is fundus ophthalmoscopy performed in this case? They use a light source of not one, but different colors. The specialist switches them, the light is reflected from the fundus of the eye. This procedure is considered more highly informative than direct and indirect ophthalmoscopy. In particular, switching a filter of different colors allows you to identify pathologies that are not visible under normal lighting.
For ophthalmochromoscopy, the equipment already described above is used. Only in this case, ophthalmoscopes are additionally equipped with light filters that allow you to switch shades of light.
What can be seen during the examination
During this diagnosis, the following is considered:
- The optic disc should be round or oval and pale pink. Its edges are clearly defined, and in the center there is a vascular funnel. Most often, its uneven color is lighter towards the temple, and slightly darker towards the nose. Changes in color, uneven edges, expansion of the funnel - all this will indicate pathologies.
- The vessels of the optic disc should extend from the center of the disc, be uniform, without expansion or contraction. Their size and ratio, color, as well as the pulsation of blood in them are assessed.
- Yellow spot (macula). It looks like a horizontal oval of dark red color, usually the macula is surrounded by a light (foveal) reflex. At a young age, the macula has a shiny point, but with age (after 30 years) the brightness of the glow decreases.
- The retina of the eye. In a healthy eye, it is transparent, pink (at a young age), over time its color becomes darker, right up to dark red (in older people). The vessels are clearly visible on it. If there are diseases, then there will be hemorrhages, ruptures, detachments, and areas of depigmentation.
Ophthalmochromoscopy - what is it?
This method was developed by the Soviet scientist Vodovozov in the 80s of the 20th century. Ophthalmochromoscopy is a type of direct ophthalmoscopy. The essence of the technique is the same: the doctor uses a direct stream of light to illuminate the inside of the eye through the dilated pupil. But Vodovozov suggested using colored baits. They are mounted on the ophthalmoscope. The system includes several filters: green, red, cobalt, blue, yellow, magenta. When you install the green attachment, the red color is retained, making the retina, the pattern of nerve fibers and other structures of the inside of the eye easier to see. Also, such a filter will detect hemorrhages. Depending on the indications and symptoms, the color of the nozzle is selected. They are easy to change, so you can use several pieces during one inspection.