- Retinal detachment: statistics and risk group
- Myopia and retinal detachment
- Retinal detachment: causes
- Retinal detachment: symptoms and diagnosis
- The importance of timing of surgery for retinal detachment
- What happens if you don't have surgery?
- Retinal detachment: disability
- How is the operation performed?
- Rehabilitation after surgery
- Silicone or gas?
- Prescriptions after surgery
- Restrictions after surgery
- Contraindications for surgery
- Retinal detachment in children
- Prevention
- Retinal detachment: folk remedies
We met with a famous ophthalmic surgeon, professor, MD.
Arseny Aleksandrovich Kozhukhov to talk about such a problem as retinal detachment.
— Arseniy Alexandrovich, how common is the problem of retinal detachment?
According to analytical data, 1-2% of people
. Most often it occurs in people who have suffered an eye injury, in those who have myopia, with retinal dystrophy, and intraocular tumors. Moreover, the degree of myopia in such cases is from -1 to -5. You will be surprised, but even a high degree of myopia (even -20) less often leads to retinal detachment.
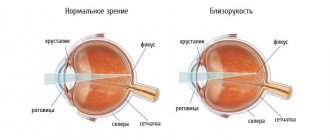
— Many people today have myopia... Why can myopia become one of the causes of retinal detachment?
Retinal detachment involves the separation of the vitreous humor, a gel-like substance that fills the inside of the eye, pressing the retina against the uvea. With myopia, the eye stretches in length, but the vitreous body partially remains in place. It begins to contract and gradually tear off, peeling off from the retina. And this is a very important point, because if the vitreous body does not gradually separate from the retina, but literally tears out a piece of it, then a rupture of the retina will occur, and then its detachment. Therefore, anyone with myopia is at risk.
— Will people be able to prevent retinal detachment if they eliminate myopia with laser vision correction?
No, they will not solve or prevent the problem, because myopia occurs due to the fact that the eye elongates in length, and laser correction is carried out on the cornea, we cannot shorten the eye. Therefore, after surgery for laser correction of myopia, the patient also remains at risk.
In view of this, people suffering from myopia need to see an ophthalmologist once a year, in particular, to check for retinal dystrophy and retinal tears. In situations where the doctor detects signs of severe retinal dystrophy, its ruptures, it is necessary to perform laser coagulation of the retina - microscopic laser burns that are applied to the retina around dangerous lesions in order to strengthen them and so that intraocular fluid does not flow into the resulting gap and does not detach the retina .
— Does age play any role in terms of retinal detachment?
To a large extent - yes, with age the likelihood of retinal rupture and detachment increases, because over time many organs and tissues undergo degenerative changes, including the retina. However, retinal detachment is also observed in young people leading an active lifestyle, especially when two risk factors occur - myopia and injury.
— What are the symptoms of retinal detachment?
There are several warning signs of retinal detachment.
First of all, this is the flashing of lightning and flashes before the eyes - an effect when the vitreous body pulls and twitches the retina. But this may not be the case. The classic symptom of retinal detachment is the appearance of a “curtain” - a translucent veil - on one side, which gradually increases until it covers the entire field of vision. Then the eye practically ceases to see at all. As soon as you notice flashes, you need to immediately run to an ophthalmologist, because the sooner you seek help, the greater the chance of maintaining your vision and avoiding major surgery.
— How is retinal detachment diagnosed?
The main tools in diagnosing retinal detachment are the slit lamp and special lenses for reverse ophthalmoscopy with different diopters. They allow you to clearly see the fundus with all the small details. Some ophthalmologists use a reverse forehead ophthalmoscope, which also allows one to accurately diagnose retinal detachment. If doubts remain, then there is, among other things, a three-mirror Holman lens, as well as various options for wide-angle lenses that allow you to see all the smallest nuances on the retina. But if there is clouding of the lens, cornea or vitreous body, then ultrasound comes to the rescue, with the help of which gross changes and retinal detachment can be recognized.
— Does retinal detachment need urgent surgery?
Absolutely right. The duration of the detachment and the timing of the operation for this problem are very important.
When the central zone of the retina (macula) is captured, a large accumulation of nerve receptors located in it begins to quickly atrophy - die. It is optimal to perform the operation before the macula is captured. If it nevertheless exfoliates, then it is not possible to completely preserve vision, but nevertheless, you can get fairly high vision, close to 100%, if surgery is performed at least during the first week. In cases where this period was missed, the result in a week will be twice as bad. After three months, it is possible to preserve no more than 30-40% of vision. And after six months, very often it no longer makes sense to have surgery at all, because only 1-2% of vision remains.
Retinal detachment needs to be operated on urgently!
— And if a person starts a problem, then he lives with a poorly seeing eye?
Yes, the eye stops seeing altogether. Moreover, this threatens the loss of the eye as an organ, because when the retina detaches, hypotension often develops - a decrease in pressure in the eye, as a result of which it begins to decrease in size, which leads to subatrophy. Often, this is just a cosmetic defect. However, it happens that over time, the body begins to produce antibodies to the tissues of the subatrophic eye, which can lead to the death of the second eye. Thus, sympathetic ophthalmia appears when, as a result of injury, retinal detachment, antibodies are produced to both the tissues of the affected eye and the tissues of the healthy eye. Then one eye begins to pose a threat to the second and must be removed as quickly as possible before it “ruins” the neighboring eye.
— Do they give you disability if you have a retinal detachment?
Yes, they do, but only if it is impossible to restore vision.
Basic principles of diagnosis for retinal pathology
- The patient should be examined for visual acuity. In this case, the doctor determines the preservation of the function of the central areas, which may be affected by retinal pathology.
- It is necessary to measure the level of intraocular pressure.
- All patients undergo determination of the boundaries of the visual field. For this purpose, computer perimetry is often used. This test helps diagnose peripheral retinal lesions.
- An electrophysiological examination of the patient helps to establish the integrity of the function of the optic nerve, determine the viability of retinal cells and the neurons themselves.
- During direct or indirect ophthalmoscopy, the doctor examines the features of the fundus of the eye; based on the examination, it is possible to determine the areas of retinal rupture, as well as their number and tendency to detachment. In addition, it is possible to determine the connection between the area of detachment and the substance of the vitreous body, and to identify areas of thinning, since they require special attention during surgical treatment of the eyes.
Why is preventive retinal examination necessary?
The earlier retinal pathologies are diagnosed, the greater the chance of restoring visual function and avoiding surgical intervention. Advanced diseases are more difficult to treat, and if left untreated for a long time, they inevitably lead to retinal ruptures and detachment. To avoid complications, it is recommended to regularly examine the retina. It is especially important to undergo preventive examinations for people who are at risk for developing retinal pathologies:
- pregnant women;
- older people over 50 years of age;
- patients with diabetes mellitus;
- people suffering from hypertension and diseases of the kidneys and adrenal glands;
- patients suffering from varying degrees of myopia.
It is also recommended to check the retina after suffering infectious diseases, traumatic brain injuries and mechanical damage to the eyes. You should always remember that preventing a serious disease or stopping its development at an early stage is much easier than dealing with a rapidly progressing pathology.
Diagnostic methods for retinal diseases
Patients with suspected retinal pathology undergo the following studies:
- Determination of the patient's visual acuity.
- The study of contrast sensitivity, which allows us to judge with high accuracy the condition of the central macular zone.
- Study of color perception and color thresholds.
- Ophthalmoscopy.
- Perimetry, the purpose of which is to determine the boundaries of the field of view.
- Electrophysiological examination techniques.
- Fluorescein angiography, which allows you to thoroughly study the pathology of the vascular system of the eye.
- Optical coherence tomography is aimed at qualitatively determining retinal pathology, as well as the severity of the process.
- Fundus photography is carried out to record pathological changes that can be assessed over time.
Alternative examination methods
Even in ancient times, doctors were able to determine the presence of diseases by the eyes, or rather by the iris. As a result of the examination, the doctor has the most complete picture of the patient’s health status and can determine the presence of diseases that have not yet manifested symptoms that are unpleasant for the person. People at risk are advised to constantly monitor their eye health. So, to check the retina, there are special tests in the form of cards and tables that will help identify pathologies of the visual organs in the early stages of development.
In case of suspicions or complaints about eye health, a remote consultation with an ophthalmologist is available.
Telemedicine opens up enormous opportunities and allows you to consult regarding a complaint at any convenient time. An accurate diagnosis cannot be made remotely, but such a consultation will help determine whether a detailed examination is needed in the clinic or not. Take care of your eyesight, monitor your health and remember that preventing a disease is easier than treating its advanced form. Yakovleva Yulia Valerievna
Cost of retinal diagnostics
- Initial consultation with a retina specialist (laser surgeon) - 3,000 .
- Repeated consultation with a retina specialist (laser surgeon) - 1,000 .
- Fundus examination with a narrow pupil - 1,000 .
- Examination of the fundus with a wide pupil - 1,200 rubles.
- Amsler test (for macular degeneration) - 500 rubles.
- Electrophysiological study of the retina and optic nerve (EFS) - 500 rubles.
- Ultrasound of the eyeball - 1,500 rubles.
- Optical coherence tomography of the retina - 2,000 .
Above are the prices for the main diagnostic services of our ophthalmology center at the time of publication of the material. You can find out the exact cost of services and make an appointment by calling the numbers listed on our website.
TREATMENT OF RETINA DETACHMENT
Treatment is necessary, and only surgical, there is no other way out.
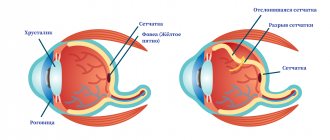
No drops, ointments, tablets, injections, or absorbable agents help, but only take time, which allows the detachment to develop further and further. The earlier competent surgical treatment is carried out, the better results it gives and the more vision can be restored. The goal of surgical treatment was formulated more than 100 years ago and is to close (block) the retinal tear. At the initial stage of the disease, there is usually no need to go inside the eye, and surgery consists of local external indentation in the projection of the rupture. For this purpose, special fillings made of soft silicone are used, which press against the area of the rupture, thus blocking it.
Scheme of episcleral filling
As soon as the hole in the retina closes, everything miraculously improves, the “curtain” disappears, and vision begins to be restored. Peripheral vision is restored first; the person discovers that the “vision” is almost normal; later it actually becomes normal. The periphery of the retina is quite stable, and as soon as it returns to its anatomical place, it immediately begins to “work” and recovers well even with long-term retinal detachment. With central vision, things are not so simple. The most favorable cases are when the detachment has not had time to “crawl” to the center. For example, if vision in the center remained 1.0, and half of the field of vision was already covered by a “curtain,” after a successful operation, vision can be restored to 1.0, and the curtain will disappear.
If the detachment has managed to close the central zone, after a successful operation, central vision, unfortunately, cannot be fully restored. What visual acuity will be after surgery in this case depends on a number of factors. The most important of them are the time during which the central zone of the retina was detached, and the state of the blood supply to the retina, which directly depends on age and the degree of myopia (if any).
Recovery of central vision occurs slowly and is usually almost complete by 3 months. In the future, improvement may continue, but at an even slower pace, and we observe that both after a year and after 3 years, visual acuity improves slightly.
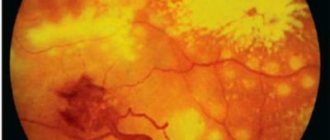
Changes in the structure of the retina after detachment, worsening the “picture”
If a person with a retinal detachment is not operated on in time or is operated unsuccessfully, then the detachment persists and continues to develop, in addition, the so-called “proliferative process” begins in the vitreous body.
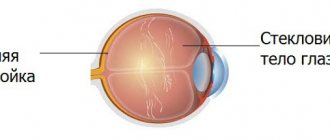
The eye, as you know, has the shape of a ball, and we already know that it has a lens, a photographic retina, and in addition, the inside of the eye is filled with liquids. These liquids are almost 98-99% water, but with very significant additives. The anterior part of the eye is limited by the cornea on one side and the iris-lens unit on the other. This part of the eye is more responsible for optics and is filled with anterior chamber intraocular fluid. In its properties and appearance, it is almost no different from simple water with the addition of a complex set of minerals and salts.
Another thing is the fluid in the posterior part, limited by the lens, ciliary body and retina. This fluid is called vitreous humor and has the consistency and appearance of a gel or frozen jelly. In addition, the vitreous body is based on a frame in the form of a three-dimensional lattice of collagen fibers.
In case of retinal detachment, the vitreous body never remains indifferent. In the initial period, only slight disturbances in its structure are observed, manifested in the form of various inclusions floating in the field of view. With a long-term detachment, strands develop in the vitreous frame, which, like ropes, are attached to the surface of the retina and, slowly contracting, pull the retina to the center of the eyeball. This process is called vitreoretinal proliferation, which ultimately leads to the formation of the so-called “funnel-shaped” retinal detachment. In such a situation, reconstructive surgery is required, the quality of which is of a much higher level. It is almost impossible to close such a gap with fillings, and it is not enough. The main task is to cleanse the surface of the retina from vitreous cords, straighten it, and then block the tear.
Picture of a severe form of proliferative retinopathy.
For this purpose, special methods are used, the so-called vitreoretinal surgery. Its essence lies in the fact that through pinpoint punctures with long and thin instruments, the surgeon enters the inside of the eye and removes the strands, freeing the retina and straightening it. The process itself is very reminiscent of the painstaking work of a master who, through the neck of a bottle with long tweezers and scissors, assembles a model of an 18th-century sailing ship inside the bottle.
Schematically, this is what a vitrectomy operation looks like
. This operation is very delicate and complex, if you remember that the retina is extremely delicate and fragile nervous tissue, and almost every part of it is responsible for some area of vision. During the operation, the doctor looks inside the eye through its anterior segment, looking “through the pupil.” This requires high transparency of the optical media, that is, the lens-cornea and lens must be as transparent as possible. If the lens is cloudy, that is, the patient has a cataract, then, as a rule, at the initial stage, the lens is replaced with an artificial one, and only then the “repair” of the retina begins.
We discussed how this is done in these posts:
- Cataract: it awaits you personally (if you live, of course)
- We implant an artificial lens (you will need this after 60 years)
In addition, the natural lens, due to its anatomical location, often interferes with working on the peripheral parts of the retina.
In these cases, it is also necessary to change the lens to an artificial one, otherwise the uncleaned areas of the peripheral retina may not allow it to achieve its anatomical fit. The operation is performed in a “dark room”, that is, only a light guide in the surgeon’s hand or an additional light source “chandelier” illuminates the working field like a chandelier, the microscope light is turned off.
Externally, it happens like this (photo from the operating room)
After complete cleansing of the retinal surface from the vitreous strands, it must be straightened and placed on the choroid, that is, its anatomically correct position inside the eye must be obtained. For these purposes, so-called “heavy water”—a liquid perfluoroorganic compound (PFOS)—is often used. This substance in its properties is almost no different from ordinary water, but due to its higher molecular weight it acts like a press on the surface of the retina, smoothing and pressing it. “Heavy water” copes with detachment very well, in addition, it is absolutely transparent, and the eye filled with this liquid begins to see almost immediately. The main disadvantage is that the eye cannot tolerate it for a long time. A maximum of a couple of weeks, but in practice it is not advisable to leave this liquid in the eye for more than 7-10 days. This means that immediately after straightening the retina, it is necessary to close, “seal” all the breaks in the retina, so as not to get a detachment again after removing the “heavy water”.