The vitreous body is one of the liquid eye tissues, gel-like in consistency, normally completely transparent and filling the entire space between the retina and the lens (about two-thirds of the internal volume of the eyeball). The filling should initially be dense and uniform, without any bubbles, cavities or gaps. This is ensured by the presence in the vitreous body of such a well-known substance (from aesthetic medicine) and having a unique set of properties as hyaluronic acid. Even a minimal concentration of this natural polymer - and the otherwise healthy vitreous body consists almost entirely of water with a small admixture of fibril fibers - is sufficient for reliable lubrication and filling of the intraocular space.
However, with age, as well as under the influence of certain unfavorable factors, the composition of the vitreous body may change; it begins to move away from the inner walls, which leads to specific disturbances in visual functions and may be a harbinger of serious problems for vision in general. Depending on the location, there are two main types of such detachment – anterior and posterior. In the first case, which is most often associated with purely age-related changes, voids form between the vitreous body and the lens. By posterior vitreous detachment, or PVD, we mean its “departure” from the back wall of the eye; this option is usually clinically less favorable and has a wider range of possible causes.
Symptoms:
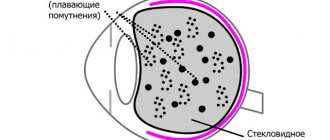
- floating opacities in the form of transparent or black dots, lines or figures with inertial movement, which arise when the eyes turn and settle, like “a mule in a glass of water.” Patients often describe their complaints as the appearance of “floaters” in their field of vision. Blurred vision does not affect vision; rather, it is irritating. They are clearly visible against the background of snow cover, a white wall, and a cloudless sky. Such complaints arise over time in almost all people.
- flashes or lightning that are clearly visible in a dark room. They are caused by the fact that when the vitreous body detaches from the retina, it stretches and stimulates the photoreceptors. Actually, the appearance of these complaints indicates the beginning of posterior vitreous detachment. Over time, the brain identifies these phenomena as additional and cuts off the unnecessary image.
Causes of PVD
Newborns have a homogeneous structure of the vitreous body, which fits tightly to the retina. As the body ages, the tissues of the vitreous body are divided into 2 fractions - liquid (almost water) and fibrous, which is protein molecules glued together - it is this that peels off from the retina. This process is very common and, as a rule, not dangerous. PVD is typical for almost every person. However, with myopia, this phenomenon is especially common and occurs earlier by about 10 years, compared to people with normal vision. However, it is believed that PVD occurs somewhat more often in women, which is associated with hormonal changes inherent in menopause.
Posterior detachment has different heights, lengths and shapes, and can be complete or partial. The vitreous body is firmly attached to the retina in several places. Age-related liquefaction usually provokes a complete posterior vitreous detachment, which is detected along the entire length of the posterior pole of the eye, and has a more or less pronounced shift to the center. In this case, there is a separation of the vitreous body from the optic nerve head, which does not cause damage to the retina, while the subvitreal space is filled with intraocular fluid.
Partial PVD, with the attachment of vitreous fibers to the retina in several places (fixation points), is the most dangerous, as it is associated with a large number of complications that occur with this condition. When the vitreous body decreases in volume, which occurs due to abnormal growth of the eye (usually caused by myopia), inflammation or injury, partial detachment from the retina often occurs. Due to excessive traction of the entire mass of the detached body, as well as swaying of the vitreous body during eye movements, a hole in the retina or its complete detachment in limited areas may occur. When a retinal tear occurs, fluid from the space in the vitreous begins to leak through the hole, flowing between the retina and the back wall of the eye. This aggravates the process by separating the retina from the back wall of the eye, causing retinal detachment.
Differential diagnosis of opacities:
In addition to point opacities, massive coarse opacities may appear in the vitreous body, caused by hemorrhages or vitreous cords. These changes are unfavorable and can significantly affect vision. Only an ophthalmologist can distinguish them. With atherosclerosis and other metabolic disorders, there may be deposits of brown pigment in the vitreous body, as well as cholesterol, opalescent inclusions in the form of “golden” or “silver” rain. Such inclusions are opaque and affect visual acuity. They cannot be treated, but if they interfere significantly, symptomatic removal of the vitreous is possible. You should consult an ophthalmologist about the advisability of surgical intervention.
Posterior vitreous detachment is a normal age-related process that occurs after the age of 40 in 70% of patients. Factors that contribute to this may be myopia, especially with correction of more than 6 diopters, surgery for cataracts, injuries, inflammatory processes of the organ of vision (uveitis, chorioretinitis, etc.).
Destruction of the vitreous body
There are two types of destruction of the vitreous body. In inflammatory diseases of the vascular tract, due to changes in the biochemical composition of the vitreous body, thin fibrils become coarsened, stick together, and thus filamentous destruction
in the anterior or posterior parts of the vitreous.
Granular destruction
develops most often in dystrophic diseases of the vascular tract, in diseases associated with metabolic disorders of connective tissue (polyarthritis, osteochondrosis, etc.). Biomicroscopy reveals “luminous opacities” in the anterior parts of the vitreous body. If the chemical composition of the particles turns out to be calcium salts associated with fatty acids, granular destruction of this nature is called “silver rain”. If the chemical composition of the vitreous particles contains cholesterol crystals, carbon dioxide and phosphoric acid salts of magnesium and calcium, such granular destruction is called “golden shower”. Granular destruction most often does not affect visual acuity and is not subjectively felt by patients.
Complications:
This is not a retinal detachment, but the two concepts may be related. The retina is an ultra-thin structure and is attached to adjacent tissues using only intercellular connections. In the presence of peripheral retinal degenerations, chorioretinal dystrophies, or traumatic injuries, the vitreous body may have a strong attachment to the retina and, when exfoliated, can pull it along with it. A retinal tear occurs. And this threatens irreversible vision loss and requires immediate surgical intervention.
Vascular defects are also possible, causing hemorrhage - hemophthalmos, which also requires immediate consultation with an ophthalmologist.
Retinal detachment and hemophthalmos are possible in 15% of cases. After posterior vitreous detachment, the increased risk (2-6%) of detachments remains for 3-6 months. Currently, patients should limit physical activity and, if new symptoms appear (massive floaters, sudden deterioration of vision, loss of half the visual field), immediately contact an ophthalmologist.
If you have similar complaints, but at the same time you do not feel a deterioration in visual acuity, there is no need to immediately consult an ophthalmologist, but for the purpose of prevention, it is advisable to undergo basic examinations. Posterior vitreous detachment is an age-related process that does not require therapeutic measures. Over time, we get used to floaters and do not pay attention to them. Only possible complications pose a threat, in particular hemophthalmos and retinal detachment, so their timely detection is a guarantee of vision preservation.
Treatment
Conservative treatment of vitreous detachment of the eye is almost never carried out. If the course is successful, the pathology does not require correction. After weeks or months, the fibers fall below the optical axis and illusory visions (floaters, transparent figures) disappear. Sometimes doctors prescribe a course of strengthening medications:
- Wobenzym is a tablet product. Relieves inflammation and swelling, relieves pain, strengthens the immune system. It also has antiplatelet and fibrinolytic effects. The dosage is determined individually by the attending physician.
- Taufon – stimulates metabolic processes in eye tissues, accelerates wound healing. The active substance is taurine. Use 1 to 2 drops 4 times a day. The therapeutic course can last up to 3 months.
- Emoxipine is an antioxidant. Helps strengthen blood vessels in the retina and mucous membrane, improves nutrition of the visual organs. The active ingredient is methylethylperidinol. Drip from 1 to 2 drops 3 r. per day.
- Potassium iodide - apply a 2% solution to the eyes. It has an antisclerotic effect and accelerates the resorption of hemophthalmos. Drop 1 drop up to 4 r. per day for no longer than 14 days.
Ophthalmologists recommend protecting your eyes from bright sunlight and reducing eye strain.
If the patient's work involves a computer, you should take a five-minute break every 30-60 minutes and rest your eyes. It is useful at this time to do gymnastics, lower your eyelids and relax. If visual acuity begins to decline and there is a risk of retinal detachment, surgery is recommended. There are the following surgical options for complications of the pathological process:
- Vitrectomy – removal of the vitreous body completely or partially. Instead, the eyeball is filled with a special saline solution. The procedure has been practiced since the 70s of the twentieth century, but it cannot be called absolutely safe. After surgery, there is a risk of developing glaucoma, cataracts, and hemophthalmos (extensive hemorrhage).
- Vitreolysis is an operation using YAG laser radiation. It is used to treat the vitreous body in order to change its chemical and physical properties and restore transparency. As a result of the procedure, the structures of the eye may be damaged and retinal or ventral hemorrhages may develop.
Read in a separate article: False myopia (myopia): what it is and how to treat it
Surgeries for this diagnosis are complex, and the risk of developing vision problems subsequently is quite high. However, if there is a possibility of damage to the retina, this is the only correct solution, otherwise blindness cannot be avoided. The type of surgical intervention is selected individually by the ophthalmologist.
If treated in a timely manner, the success rate of the operation is approximately 90%.
ethnoscience
Folk remedies provide only auxiliary treatment for vitreous detachment. The following recipes are used:
- Honey is dissolved in water in a ratio of 1:5 and dropped into the eyes 3 times a day for a month. The liquid is stored in the refrigerator for no longer than a week. Before instillation, the honey solution is heated in warm water to room temperature.
- A couple of aloe leaves are crushed and filled with water infused with silver (100 ml). after three hours, filter the product and add ½ tsp. honey Drop into the eyes for a month 3 times. in a day.
- 0.25 tsp Melt honey in a water bath, pour in the same amount of aloe juice. Dilute the mixture in 50 ml of boiled water, add 1 tsp. ground cloves. Leave for 48 hours, shaking occasionally. Then the infusion is filtered and instilled 3 times a day for a month.
You can use the products only if you are not allergic to honey or other recipe ingredients. Traditional medicine should be used to treat this pathology after the recommendation of an ophthalmologist.
Pathogenesis
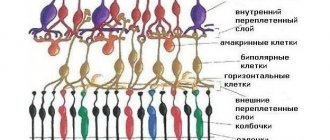
The main reason for the development of vitreous detachment is a disruption of the interaction between the posterior hyaloid membrane (PHM) of the vitreous body and the internal limiting membrane (ILM) of the retina. The hyaloid membrane of the vitreous body consists of collagen fibers, hyalocytes, a special protein fibronectin and laminin (they are the basis of the intercellular matrix).
It forms the outer layer of the vitreous humor, which is adjacent to the retina. The inner membrane of the retina contains collagen fibers, hyaluronic acid, and the plasma membrane of the Müller cells of the retina. The thickness of the limiting membrane of the retina varies. The thinnest thickness and stronger connection with the vitreous are observed around the vessels of the retina, optic disc and macular region. Along the remaining length, thickening of the membrane and a less strong connection are detected.
Depending on the penetration of vitreal fibrils into the layers of the retina, on the one hand, and the presence of fibronectin and laminin, on the other, the strength of contact between the vitreous body and the retina is determined. With age (usually after 50 years), the limiting membrane of the retina thickens, which reduces the ability of Müller cells to produce intercellular substance and maintain its normal level.
The development of this disease is based on a failure in the interaction of the posterior hyaloid membrane of the vitreous segment and the inner part of the membrane. With age or as a result of certain etiological factors, there is a decrease in vitreoretinal connection and subsequent separation of the limiting membrane, which leads to posterior vitreous detachment.
The main reason for the development of vitreous detachment is a disruption of the interaction between the posterior hyaloid membrane (PHM) of the vitreous body and the internal limiting membrane (ILM) of the retina. The hyaloid membrane of the vitreous body consists of collagen fibers, hyalocytes, a special protein fibronectin and laminin (they are the basis of the intercellular matrix).
We invite you to familiarize yourself with the muscles of the eye, structure, functions, symptoms and treatment.
It forms the outer layer of the vitreous humor, which is adjacent to the retina. The inner membrane of the retina contains collagen fibers, hyaluronic acid, and the plasma membrane of the Müller cells of the retina. The thickness of the limiting membrane of the retina varies. The thinnest thickness and stronger connection with the vitreous are observed around the vessels of the retina, optic disc and macular region. Along the remaining length, thickening of the membrane and a less strong connection are detected.
Posterior hyaloid membrane (PHM) and its detachment: symptoms, diagnosis and treatment, clinics
The posterior hyaloid membrane (posterior limiting membrane) is a structure that is attached along the periphery of the optic nerve head in the area of its base. This structure is less firmly connected in the area of attachment to the sclera of the extraocular muscles, in the area around the macula, and in the area of some retinal vessels.
In healthy individuals, it is adjacent to the internal limiting membrane throughout its entire length.
In pathology accompanied by destruction of the vitreous body or its partial loss (due to injuries and surgical interventions), the posterior hyaloid membrane is already loosely attached to the retina, as a result of which there is a high risk of vitreous detachment.
If the posterior hyaloid membrane is torn away from the retina along its entire length (except at the base), total vitreous detachment occurs. This is a favorable factor that prevents the development of proliferative vitreoretinopathy. In this case, the vitreous body shifts to the anterior base.
In this case, the patient sees “floaters” before the eyes, ring-shaped spots (this is what a torn section of the membrane looks like), Moor’s stripes (sparkling stripes) in case of detachment of attachment zones to the retina. When performing ophthalmoscopy, a ring-shaped clouding is determined. Vitreous detachment is sometimes discovered accidentally during a B-mode ultrasound scan or fundus examination.
If the attachment of the posterior hyaloid membrane to the retina is preserved in the areas of projection of the oblique muscle attachments, in the area of blood vessels, around the macula, in areas of fibrosis and dystrophy, total vitreous detachment does not occur. In this case, tractions are formed, causing retinal tears. This condition is unfavorable. The formation of retinal folds, the development of hemophthalmos, and retinal detachment are possible.
Detachment of the posterior hyaloid membrane has features, in particular, related to its excess area relative to the residual volume of the vitreous body.
The membrane forms crypts, folds that create vitreovitreal cavities. Over time, the folding of the posterior hyaloid membrane is lost, and it takes on the appearance of a smooth membrane pulled towards the lens.
This is the cause of the so-called invisible detachment of the posterior hyaloid membrane.
Degree of detachment of the posterior hyaloid membrane
There are four degrees of posterior hyaloid membrane (PHM) detachment:
- First: the membrane is visible only with a Gruby lens.
- Second: the membrane is visualized without a lens at maximum proximity to the eye.
- Third: folding of the posterior hyaloid membrane is easily determined without a Gruby lens.
- Fourth: the foldless membrane is close to the lens of the eye (less than the depth of its optical section from the posterior capsule).
Macular edema is believed to be a consequence of vitreoretinal traction. This condition is also possible with partial detachment of the posterior hyaloid membrane and vitreous body. In such cases, in order to prevent the formation of retinal cysts, posterior vitrectomy and removal of the posterior hyaloid membrane are performed.
Posterior hyaloid membrane: relationship with vitreoretinal proliferation
Pathological adhesions of the retina and posterior hyaloid membrane are an unfavorable prognostic sign of many eye diseases. This condition is accompanied by vitreoretinal proliferation.
The appearance of a proliferating tissue is largely determined by the integrity of the posterior hyaloid membrane of the vitreous body. If there is a defect on the anterior surface of the membrane, proliferating tissue layers on it.
There are five types of proliferating tissue:
- Hypocellular, or glial (with inclusions of free cells).
- Glial-vascular (has growing interstitial thin-walled vessels).
- Glial-vascular fibrous (in addition to vessels, contains growing fibrous membranes in glial tissue).
- Fibrovascular (contains predominantly fibrovascular tissue).
- Fibrous (compact connective tissue with few or no vessels).
Treatment of posterior hyaloid membrane detachment and vitreoretinal proliferation
Currently, specialists have developed various methods of laser, drug and surgical treatment of conditions that provoke vitreoretinal proliferation. As a rule, complex treatment with pharmacological agents is aimed at resolving hemophthalmos, including recurrent ones.
Surgical treatment consists of vitrectomy with removal of the posterior hyaloid membrane, which is in contact with different parts of the retina and the optic disc ring. Various vitreous substitutes are used, and therapeutic and preventive laser coagulation of the retina is performed.
In order to eliminate traction, laser and surgical schwartotomy and laser vitrectomy are performed (a non-invasive method of removing the vitreous body, which makes it possible to cause vitreous detachment in patients with progressive diabetic retinopathy, to achieve resorption of hemophthalmos and preretinal hemorrhage.
Currently, promising developments are being carried out on non-invasive methods for the prevention and treatment of proliferative vitreoretinopathy, traction of the posterior hyaloid membrane, based on the relationship of hemostatic, immunological, neurohumoral and humoral mechanisms, the influence of biologically active substances coordinating these mechanisms.
Moscow clinics
Below are the TOP 3 ophthalmological clinics in Moscow, where you can undergo diagnosis and treatment of detachment of the posterior hyaloid membrane.
Source: https://mosglaz.ru/blog/item/1336-zadnyaya-gialoidnaya-membrana-i-ee-otslojka.html
Detachment of the posterior hyaloid membrane
It has been proven that changes in the structure of the vitreous body with compaction of its frame in older people, as well as violations of the integrity of the anterior hyaline membrane shell, have an important role in the occurrence of posterior vitreous detachment, which is provoked by displacement of the vitreous body to its anterior base. Posterior vitreous detachment, accompanied by partial or complete vitreal collapse, develops due to the transfer of fluid from the vitreous to the preretinal space.
When diagnosing vitreous detachment, it is customary to distinguish 4 degrees of its development:
- Grade I – MH is visible only with the use of a Gruby lens.
- Degree II – the MH is visible without a lens, when approaching the eye.
- Degree III – folding of the cervical membrane can be easily detected without a Gruby lens.
- Degree IV - the PGM, already devoid of folds, is adjacent to the lens very close: less than the depth of its optical section from the posterior capsule.
The study organizers also believe that macular edema occurs as a result of vitreoretinal traction. This condition often occurs when the vitreous body is detached incompletely. Now, to reduce edema and also prevent the formation of retinal cysts, posterior vitrectomy is performed with removal of the cervical mass.
The occurrence of pathological fusion of the cerebral tumor with the retina is unfavorable in terms of the prognosis of many eye diseases accompanied by vitreoretinal proliferation. Naturally, the question arises about measures aimed at eliminating such contact.
Numerous methods for treating complications leading to the development of proliferative vitreoretinopathy, developed by domestic and foreign specialists, include medication, laser and surgical methods. Complex drug treatment is usually aimed at the rapid resolution of hemophthalmos, which often recur.
Techniques have been developed in detail for complete, partial, and also posterior vitrectomy with excision of the cervical disc in contact with any parts of the retina, the optic disc ring or the base of the vitreum.
The introduction of vitreous substitutes is provided, and therapeutic and preventive laser coagulation of the retina is used.
Surgical or laser suturing is performed to eliminate existing local tractions.
conclusions
Vitreous detachment is a common disease, which is largely determined by the functioning of the visual organs throughout life. In order to avoid the development of this disease, it is worth paying due attention to your health from an early age, and in case of injuries or damage to the eye, contact a specialist in a timely manner, since some visual impairments may not appear immediately, but only after a long time.
The information on the site is presented for informational purposes; be sure to consult an ophthalmologist.
Symptoms
The nature of the clinical picture, as a rule, depends on the type of disorder. The following symptoms may be present:
- “lightning” when rotating the eyes.
- light flashes, without external negative factors.
- floating film in the eye.
- various visual hallucinations – geometric shapes, “floaters”.
It is noteworthy that at the initial stages of development of the pathological process, a decrease in visual acuity is not observed.
Quite often, fibroplastic syndrome is combined with other ophthalmological diseases, so the overall clinical picture may be supplemented by the following signs:
- hypersensitivity to light stimuli;
- “dry eye syndrome” or, on the contrary, increased lacrimation;
- redness of the affected organ of vision;
- hemorrhage, which leads to redness of the eyeball;
- symptoms of diplopia.
In some cases, the clinical picture includes a syndrome such as “glass eyes.” The patient has an unnatural shine in the eyes and dilated pupils.
Posterior hyaloid membrane and its detachment - causes and treatment
Vitreoretinal proliferation can develop against the background of various eye diseases. As a result of the studies, it was possible to establish that the main role in the development of this pathology, as well as its complications (preretinal fibrosis, vitreoretinal traction, traction retinal detachment) belongs to the anatomical structure and condition of the vitreous body itself.
The posterior hyaloid membrane is attached to the optic disc along its radius. At the same time, its connection with the area of the retinal vessels, around the macula area and in the area of attachment of the oblique muscles of the eye to the sclera, this connection is much less strong.
In young patients, the posterior hyaloid membrane is in contact with the internal limiting membrane along its entire length.
If diseases occur that are accompanied by destruction of the vitreous, including surgical removal of part of it, then the density of the posterior hyaloid membrane to the retina decreases. This sometimes causes partial and complete detachment.
Symptoms and diagnosis
During the process of displacement of the vitreous body to the anterior base, the patient experiences flashing spots, a ring-shaped spot, and sparkling stripes in front of the eyes. During ophthalmoscopy, the doctor pays attention to a ring-shaped clouding that is displaced relative to the optic nerve disc.
Quite often, detachment is an accidental finding that is identified during the examination of the patient. If some areas of the posterior hyaloid membrane are firmly connected to the retina, then the development of total vitreous detachment is impossible.
In this case, traction occurs, leading to retinal rupture and tractional detachment.
Some scientists believe that normally there should not be a posterior hyaloid membrane in the eyeball. Instead, there are high-density collagen fibers.
A significant role in the formation of posterior vitreous detachment is played by changes in its structure, compaction of the frame, and loss of integrity in elderly patients. As a result, fluid is transferred from the vitreous cavity to the preretinal space.
Classification
In this case, the detachment of the posterior hyaloid membrane has characteristic features, since its area exceeds the surface of the vitreous body (crypts and folds are formed). Over time, these folds smooth out, and the membrane itself moves closer to the lens.
There are four degrees of vitreous detachment:
- The membrane can only be identified using a Gruby lens.
- MPH can be determined even without a lens, but you need to get as close to the eye as possible.
- The folding of the posterior hyaloid membrane can be easily determined without the use of a Gruby lens.
- There are no folds in the structure of the posterior hyaloid membrane, and it itself is shifted towards the lens.
Vitreoretinal traction is often accompanied by macular edema. This usually occurs when the vitreous body is detached incompletely. To reduce these changes, posterior vitrectomy and removal of the posterior hyaloid membrane are performed.
Types of proliferation
Scientists believe that the risk of developing proliferating vessels depends on the integrity of the posterior hyaloid membrane, that is, if a defect occurs, proliferation can spread to the anterior surface of the membrane.
There are five types of this proliferation:
- Glial, including free cells;
- Glial-vascular, accompanied by the growth of thin-walled vessels inside the tissue;
- Glial-vascular-fibrous, in which a fibrovascular membrane grows in the glial tissue;
- Fibrovascular (mainly fibrovascular tissue);
- Fibrous, in which only hypocellular connective tissue and a small number of vessels are detected.
With the development of fibrous proliferation, a decrease in the number of pathological newly formed vessels occurs and the formation of retinal detachment.
Treatment and prognosis
The prognosis of the disease is adversely affected by the presence of pathological fusions of the retina with the posterior hyaloid membrane. In this regard, a large number of techniques have been developed aimed at eliminating this contact.
For these purposes, medication, laser and surgical interventions were used. Therapeutic techniques usually contributed to faster resolution of hemophthalmos.
The technology of posterior, partial and total vitrectomy was developed in great detail, in which the posterior hyaloid membrane was simultaneously removed. Instead of the removed vitreous substance, its substitutes are introduced. Additionally, preventive (or therapeutic laser coagulation of the retina) is performed.
To eliminate local traction, laser or surgical cordectomy can be used. There is also a non-invasive laser intervention technique in which vitreotomy is performed. As a result, the resorption of preretinal hemorrhages and hemophthalmos is accelerated, and vitreous detachment occurs.
This avoids the development of tractional retinal detachment and also keeps the optical media transparent.
A promising direction in the treatment of this pathology is the use of the relationship between immunological, neurohumoral, hemostatic, hormonal mechanisms, and lipid peroxidation processes.
Source: https://ophthalmocenter.ru/setchatka-glaza/zadnyaya-gialoidnaya-membrana.html