Structure
The outer zone of the anterior chamber is limited to the inner part of the cornea, and the inner zone is limited to the anterior side of the iris and lens capsule. The thickness of the chamber section, which is located near the pupil, is the largest (about 3.5 mm), and towards the edges it gradually decreases. After surgery to remove the lens, it becomes thicker, and when the choroid is peeled off, it becomes thinner.
Intraocular moisture nourishes the eye tissue with valuable substances and removes metabolic products from the organs of vision into the bloodstream.
The eye chambers have the same volume, which ranges from 1.23 to 1.32 cm³ of intraocular fluid. For proper functioning of the eyes, uniform production and removal of produced moisture is very important. If this balance is disturbed, intraocular pressure is disrupted. It can increase, provoking the development of glaucoma, or decrease, causing subatrophy of the eyeball. These diseases are very dangerous and can cause blindness.
Diagnostics
Photo: depositphotos.com
Typical clinical symptoms are subjective and can accompany various eye pathologies. Therefore, to clarify the diagnosis and correct treatment, various diagnostic methods are additionally used:
- examination of the eye in transmitted light;
- biomicroscopy - study of ocular media using a slit lamp;
- gonioscopy - examination of the angle of the anterior eye chamber using magnifying lenses, especially important for diagnosing the form of glaucoma;
- Ultrasound;
- OCT - optical coherence tomography of the anterior parts of the eye;
- pachymetry - measurement of the depth of the anterior ocular chamber;
- tonometry - determination of the pressure of the eye chambers;
- analysis of the fluid of both eye chambers (produced and drained).
Anterior chamber angle
In medicine, the place where the cornea joins the sclera and the iris joins the ciliary body is called the angle of the anterior chamber of the eye. This is a kind of drainage channel that removes moisture into the blood. This drainage system consists of:
- trabecular diaphragm - a special network with loose multilayer tissues;
- scleral sinus;
- collector channels.
The trabecular meshwork drains fluid into Schlemm's canal, located in the sclera near the limbus and eyeball. Approximately 15% of the moisture exits through the uveoscleral canal, passing by the trabecular meshwork. This part of the fluid from the angle of the chamber moves into the ciliary body, and then into the suprachoroidal space through Schlemm’s canal or sclera.
Eye protective apparatus
Eye socket
The orbit is part of the skull and is the container for the eye. Its shape resembles a tetrahedral truncated pyramid, the top of which is directed inward (at an angle of 45 degrees). The base of the pyramid faces outward. The dimensions of the pyramid are 4 by 3.5 cm, and the depth reaches 4-5 cm. In the cavity of the orbit, in addition to the eyeball itself, there are muscles, choroid plexuses, a fatty body, and the optic nerve.
Eyelids
The upper and lower eyelids help protect the eye from external influences (dust, foreign particles, etc.). Due to the high sensitivity, when the cornea is touched, the eyelids immediately close tightly. Due to blinking movements, small foreign objects and dust are removed from the surface of the cornea, and tear fluid is distributed. During closure, the edges of the upper and lower eyelids are very tightly adjacent to each other, and additional eyelashes are located along the edge. The latter also help protect the eyeball from dust.
The skin in the eyelid area is very delicate and thin, it gathers into folds. Under it there are several muscles: the levator of the upper eyelid and the orbicularis, which ensures rapid closure. The conjunctival membrane is located on the inner surface of the eyelids.
Conjunctiva
The conjunctival membrane has a thickness of about 0.1 mm and is represented by mucosal cells. It covers the eyelids, forms the fornix of the conjunctival sac, and then passes to the anterior surface of the eyeball. The conjunctiva ends at the limbus. If you close your eyelids, this mucous membrane forms a cavity that has the shape of a bag. With open eyelids, the volume of the cavity is significantly reduced. The function of the conjunctiva is primarily protective.
Functions of eye cameras
The purpose of the chambers is to produce aqueous humor. This process occurs in the ciliary body, which consists of a large number of vessels and is located in the posterior chamber. The priority task of the anterior chamber is to regulate the process of removing moisture from the organs of vision. Its other functions include:
- Refraction of light (focusing of rays on the plane of the retina).
- Regulation of processes occurring in different structures of the visual organs.
- Transportation of light rays to the retinal area.
Anatomy of the orbit in the light of CT
Part No. 2. Soft tissues
O.Yu.
Yatsenko Department of Ophthalmology GBOU DPO RMAPE Ministry of Health of Russia Knowledge of the normal anatomy of the bony orbit and its soft tissue contents significantly expands clinicians’ understanding of the topographic relationships of orbital structures, they can be useful for understanding the pathogenesis of pathological processes occurring in this area, and can also be used for differential diagnosis orbital diseases and patient treatment planning.
Intravital study of the soft tissues of the orbit using CT and MRI has been going on for more than 25 years [1]. It should be noted that some structures have received more attention in the literature (EOM, optic nerve, orbital tissue), while others have received less work (lacrimal gland, orbital vessels) [2-9]. And yet, despite a fairly long period of studying normal orbital structures in the specialized literature, there is still no consensus on this matter. Thus, when studying the volume of extraocular muscles (EOM), G. Forbes et al. note that the upper limits for EOM are normally 6.5 cm3 [1]. According to other authors, the volume of EOM in men is on average 2.31 cm3, in women - 1.19 cm3 [10]. Interesting is the work of S. Tian et al., who found that the volume of muscles of horizontal action is smaller compared to muscles of vertical action [9].
There is no single view on the volume of orbital tissue. Normally, according to the literature, the volume of fiber ranges from 17.21 cm3 in men and 15.63 cm3 in women [10] to 20.0 cm3 without significant differences by gender [1].
Separately, it should be noted the difficulties of studying tissues at the apex of the orbit. This is due both to the complexity of the structure and topographical identification of the apex itself, and to the determination of the volume of orbital tissues in it [11, 12]. Meanwhile, it is the defeat of this zone that causes a number of severe conditions leading to loss of vision and, in many cases, disability of patients [13-15].
Taking into account the importance of this issue, we considered it appropriate to study the characteristics of the normal soft tissues of the orbit.
Materials and methods of examination
Normal parameters of orbital soft tissue were studied from computed tomography scans in 210 subjects (266 orbits).
In 56 patients with no orbital pathology, both orbits were studied (112 orbits). In 154 patients with unilateral orbital lesions, the intact orbit (154 orbits) was examined to determine normal values. Among them are 86 men and 124 women. The average age of the subjects was 41.2±10.4 years.
Computed tomography was performed using a standard technique, obtaining axial and frontal sections. The thickness of the sections was 1.0 mm, the pitch was 1.0 mm.
Processing of the obtained data was carried out according to methods previously described in the literature and part No. 1 [7, 10, 12].
Results and discussions
We found that the muscular infundibulum in men is approximately 0.9 cm3 larger than in women and averages 9.96±0.24 cm3 and 9.03±0.14 cm3, respectively (Table 1). As follows from the table. 1, the volume of fiber in the internal surgical space accounts for 42.0% of its total volume in men and 43.87% in women. When calculating the total volume of the EOM, it was found that their volume in men is on average 2.36 ± 0.03 cm3 (indicators vary from 1.24 to 3.67 cm3), in women the volume of the EOM is approximately 0.3 cm3 less and is 2.02±0.02 cm3 (with fluctuations from 1.11 to 3.22 cm3) (Table 1).
When calculating the volume of the EOM of the eye and the levator muscle of the upper eyelid separately (with the exception of the inferior oblique muscle - its volume was calculated together with the inferior rectus muscle), it turned out that the external and superior rectus muscles had the smallest volume. The largest muscles of the orbit are the inferior and internal rectus muscles, as well as the levator of the upper eyelid (Fig. 1, Table 2). Perhaps this circumstance can explain the more frequent initial detection of changes in the inferior and internal rectus muscles in some diseases of the orbit (for example, endocrine ophthalmopathy). There is reason to assume that, under equal conditions, an increase in the initial volume of the EOM by a certain amount leads to a more significant increase and, accordingly, better visualization of initially large muscles.
As presented in table. 1, the difference in the average volumes of the optic nerve in men and women is normally statistically significant, in contrast to the values of the volume of the lacrimal gland (0.242±0.031 and 0.242±0.031, respectively). The normal volume of the eye also has significant differences between men and women, but it should be noted that almost 2/3 of the normal eye in both men and women is located inside the orbit (Table 1).
When comparing the volumes of soft tissue contents of the right and left orbits, no statistically significant differences were found in any indicator, neither in men nor in women (Table 3).
When studying the density of EOM, it was found that normally their density ranges from 29.17±1.07 to 59.26±1.01 H units. and averages 44.23±0.97 H units. (Table 4).
The range of fluctuations in EOM density is insignificant (on average 30.04±0.99 H units).
When studying the density of individual EOMs, we identified some differences. Thus, the inferior and internal rectus muscles, as well as the levator of the upper eyelid, had the greatest density, which, in our opinion, can be explained by the large volume of these muscles. At the same time, no statistical differences in EOM density indicators were detected in men and women (Table 5).
Indicators of the volume of soft tissue contents of the right and left orbits are normal.
The density of the optic nerve did not have significant differences along its entire length, but there was a tendency towards a lower average density and a larger range of fluctuations in its anterior part compared to the posterior one. The lacrimal gland, in comparison with the normal orbital structures described above, has the lowest average density and the largest range of density fluctuations, which can be explained by the heterogeneity of its structure (glandular and connective tissue) (Table 4).
The orbital tissue was characterized by a low average density (–82.7±0.54 H units) and the most significant expansion of the oscillation interval among all the studied structures (on average 47.0±0.4 H units) (Table 4). These indicators can be explained by the presence of many small connective tissue structures in the orbit, as well as the initially low density of fatty tissue. The vitreous body appears to have a fairly homogeneous structure (the average density fluctuation range is 10.1 ± 0.4 units N). The density of the vitreous body was higher than the orbital tissue, but was significantly inferior to the rest of the soft tissue structures of the orbit (Table 4).
As noted above, no difference in the average volume of orbital tissue was detected (Table 3), but it was established that 47.61% of men and 51.42% of women had individual asymmetry that did not exceed 2.0 cm3 (Table 6).
The fiber of the internal surgical space at the apex of the orbit in men is approximately 0.6 cm3 larger than in women and is equal to 41.16% and 35.74%, respectively, of its total volume. It should be especially noted that the volume of fiber in the internal surgical space at the apex of the orbit accounts for 75.35% of its total volume at the apex of the orbit in men and 73.83% in women, which is significantly more compared to the orbit as a whole and emphasizes features of anatomical and topographic relationships at the apex of the orbit [5].
Despite the fact that the volume of the muscular funnel at the apex of the orbit in men is almost 0.6 cm3 larger than in women, this difference turned out to be statistically insignificant, which may require further study on more significant clinical material (Table 7).
As can be seen from table. 8, the volume of the EOM and the optic nerve in men and women at the apex of the orbit normally did not have statistically significant differences.
When comparing the volumes of soft tissue contents of the right and left apex of the orbit, no indicators were found in either men or women (Table 8).
Conclusion
Thus, the following conclusions can be drawn:
– the volume of the EOM is normally equal to an average of 2.36±0.053 cm3 in men, and 2.03±0.04 cm3 in women;
– the normal volume of orbital tissue is 17.07±0.35 in men and 15.11±0.2 in women;
– normal orbital soft tissue volume indicators in men and women have statistically significant differences;
– the fiber of the internal surgical space at the apex of the orbit makes up 75.35% of its total volume at the apex in men and 73.83% in women;
– asymmetry of the average volumes of soft tissues of the orbit normally occurs only within the limits of statistical error;
– individual asymmetry of the volume of orbital tissue normally occurs in 47.61% of men and 51.42% of women and ranges from 0.5-2.0 cm3.
Literature
- Forbes G., Gehring DG, Gorman CA, Brennan MD, Jackson IT Volume measurements of normal orbital structures by computed tomographic analysis // Am. J. Roentgenol. – 1985. – Vol. 145. – N1. – R. 149-154.
- Tamboli DA, Harris MA, Hogg JP, Realini T, Sivak-Callcott JA Computed Tomography. Dimensions of the Lacrimal Gland in Normal Caucasian Orbits // Ophthal. Plast. Reconstr. Surg. – 2011. – Vol. 27. – N6. – P. 453-456.
- Aviv RI, Casselman J. Orbital imaging: Part 1. Normal anatomy // Clin. Radiol. – 2005. – Vol. 60. – N3. – R. 279-287.
- Kapur E., Dilberovic F. Computed tomography review of the osseous structures of the orbital apex // Bosn. J. Basic. Med. Sci. – 2003. – Vol. 3. – N3. – P. 50-53.
- Lee JM, Lee H., Park M., Lee TE, Lee YH, Baek S. The volumetric change of orbital fat with age in Asians // Ann. Plast. Surg. – 2011. – Vol. 66. – N2. – P. 192-195.
- Ji Y., Qian Z., Dong Y., Zhou H., Fan X. Quantitative morphometry of the orbit in Chinese adults based on a three-dimensional reconstruction method // J. Anat. – 2010. – Vol. 217. – N5. – P. 501-506.
- Yatsenko O.Yu. Asymmetry of the volume of the bone orbit and orbital tissue is normal // Issues of maxillofacial, plastic surgery, implantology and clinical dentistry. – 2010. – No. 2-3. – pp. 68-72.
- Ozgen A., Ariyurec M. Normative measurements of orbital structures using CT // AJR Am. J. Roentgenol. – 1998. – Vol. 170. – N4. – P. 1093—1096.
- Tian S., Nishida Y., Isberg B., Lennerstrand G. MRI measurements of normal extraocular muscles and other orbital structures // Arch. Clin. Exp. Ophthalmol. –
- – Vol. 238. – N5. – P. 393-404.
- Brovkina A.F., Karmazanovsky G.G., Yatsenko O.Yu. The volume of the bony orbit and its soft tissue contents is normal. Medical Visualization. –
- – No. 6. – P. 94-98.
- Nikolaenko V.P., Astakhov Yu.S. Orbital fractures. Guide for doctors. – St. Petersburg: Eco-Vector, 2012. – 436 p.
- Brovkina A.F., Karmazanovsky G.G., Yatsenko O.Yu., Moslekhi Sh. State of the optic nerve in edematous exophthalmos complicated by optic neuropathy (data from CT studies) // Medical visualization. – 2008. – No. 3. – P. 74-77.
- Valsky V.V., Panteleeva O.G., Tishkova A.P., Berezhnova S.G. Clinical and tomographic signs of various forms of endocrine ophthalmopathy // Scientific and practical conference diabetes mellitus and the eye. Moscow, September 29-30, 2006. – M., 2006. – P. 300-303.
- Giaconi JA, Kazim M., Rho T., Pfaff C. CT scan evidence of dysthyroid optic neuropathy // Ophthal. Plast. Reconstr. Surg. – 2002. – Vol. 18. – N3. – P. 177-182.
- Kashkouli MB, Imani M., Tarassoly K., Kadivar M. Multiple cavernous hemangiomas presenting as orbital apex syndrome // Ophthal. Plast. Reconstr. Surg. – 2005. – Vol. 21. – N6. – P. 61-63.
Pathologies
The occurrence of any pathological process in the chambers can cause decreased vision and the formation of one or another disease. Such diseases are divided into congenital and acquired.
Congenital ones include:
- lack of camera angle;
- its blockage with embryonic cells;
- abnormal fixation of the iris.
Acquired diseases include:
- Blockage of the camera corner with pigment particles.
- Uneven chamber depth. Such a disorder may occur due to displacement of the lens as a result of injury or insufficient strength and elasticity of the zonules of Zinn.
- Insufficient depth of the chamber - a violation can be caused by a closed pupil.
- Chamber angle recession is a disorder characterized by splitting or rupture of the ciliary body.
- Hypopyon is a disease characterized by the accumulation of purulent contents.
- Glaucoma is a serious disease accompanied by an increase in eye pressure.
- Hyphema is a hemorrhage that occurs in the anterior chamber.
- Goniosynechia is a pathology characterized by the formation of adhesions between the cornea and the root of the iris.
Symptoms of diseases
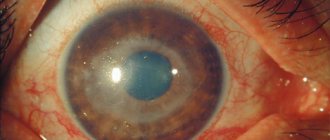
One of the most common pathologies of the organs of vision is clouding of the transparent part of the eyeball.
The following signs of violations occur:
- spasms;
- fog before the eyes;
- blurred vision;
- corneal cloudiness;
- change in iris color.
Pathologies can be congenital or acquired. Some people do not have a patent anterior chamber angle at birth or retain fetal tissue that should disappear after birth. Glaucoma occurs due to fluid imbalance. Trauma may cause pus (hypopyon) or blood (hyphema) to accumulate in the chamber. In addition, there are iris adhesions that block the anterior space.
M. M. Zolotarev in his work “Selected Sections of Clinical Ophthalmology” states that stagnation of pus or blood serves as symptoms of serious eye diseases: keratitis, corneal ulcers, iridocyclitis.
Diagnostic and treatment methods
Many of the diseases listed above occur without pronounced symptoms at first and are detected only when the pathology begins to progress, and it is very difficult to cure it.
Therefore, if any, even the most minor, symptoms appear that may indicate the presence of an ophthalmological disease, you must immediately consult a doctor.
When examining a patient, the specialist first of all identifies the presence of the following symptoms in the patient:
- Painful or uncomfortable sensations in the eyes.
- Blurred images, blurred vision.
- Decreased vision clarity.
- Presence of hemorrhages in the eyes.
- Change in eye color intensity.
- The presence of purulent discharge from the organs of vision.
- Cloudiness of the cornea.
If signs that may indicate a disease are identified, the patient is referred for an extensive examination. Common methods for diagnosing diseases caused by dysfunction of the anterior chamber include:
- Biomicroscopy.
- Ultrasound of the eyes.
- Coherence tomography.
- Gonioscopy.
- Pachymetry.
- Tonometry.
Treatment of both congenital and some types of acquired pathologies is carried out surgically. Some of them (eg, hypopyon, hyphema) can be cured with medications and other conservative therapeutic methods. Medicines are also used to treat glaucoma, but this serious pathology in most cases requires surgical intervention.
To eliminate purulent inflammatory processes, antibiotics and anti-inflammatory medications are used. If necessary, patients are prescribed physiotherapeutic procedures to improve local blood circulation in the eyes, reduce inflammation and swelling, improve the condition of blood vessels and the general health of the visual organs.
Glaucoma
When fighting glaucoma, the main task is to reduce IOP and eliminate the causes that caused the increase in pressure. This is achieved with the help of various medications (usually eye drops). However, the use of medications does not always allow for complete and permanent normalization of IOP. Therefore, patients suffering from glaucoma are advised to undergo surgery. It is carried out using a laser.
The danger of glaucoma is that increased pressure in the eyes can lead to an increase in the size of the eyeball and increased pressure on the optic nerve. This provokes its damage and subsequent death. The result is irreversible blindness.
Hyphema
If hemorrhage occurs, first of all, cold should be applied to the eyes, which allows you to quickly thrombose the damaged vessels. Then measures are taken to dissolve the blood clots that have formed in the eyes. For this purpose, eye drops and injections are used that have a resolving and vasoconstrictor effect. Antiseptics, antibiotics, and physiotherapy are also used.
If there is no positive result from the use of medications, they resort to surgery, during which the surgeon removes the formed blood clot. Lack of treatment for this pathology can provoke an increase in eye pressure and decreased vision.
Clinical anatomy and physiology of the organ of vision
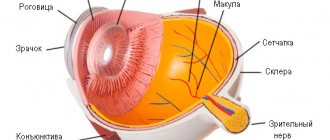
The eyeball with its auxiliary apparatus is the perceptive part of the visual analyzer. The eyeball has a spherical shape. It consists of 3 membranes and intraocular transparent media
1. Outer shell of the eye . This fibrous capsule provides turgor to the eye, protects it from external influences and serves as an attachment point for the extraocular muscles. This shell consists of two sections: the transparent cornea and the opaque sclera. The junction of the cornea and sclera is called the corneal edge or limbus. The cornea is the transparent part of the fibrous capsule, which is a refractive medium when light rays enter the eye. Its refractive power is 40 diopters (D). It contains many nerve endings; any speck that gets into the eye causes pain. The cornea itself is quite dense, but has good permeability. Through it, medicinal substances are absorbed from the conjunctival sac. Normally, the cornea does not have blood vessels, and is covered on the outside with epithelium.
The sclera is the opaque part of the fibrous capsule. It has a white or white-blue color. The muscular apparatus of the eye is attached to it, and the vessels and nerves of the eye pass through it.
2. The middle layer of the eye. It is a choroid and consists of 3 sections:
1st section - iris . It is located behind the cornea, between them there is a space - the anterior chamber of the eye, filled with aqueous fluid. The iris is clearly visible from the outside. The color of her eyes depends on her color. In the center of the iris there is a round hole - the pupil, the diameter of which depends on the level of illumination and the work of two antagonist muscles (constricting and dilating the pupil.)
2nd section - ciliary body . It is the middle part of the choroid, a continuation of the iris. From its processes extend the ligaments of Zinn, which support the lens. Depending on the condition of the ciliary muscle, these ligaments can stretch or contract, thereby changing the curvature of the lens and its refractive power. The ability of the eye to see near and far equally well depends on the refractive power of the lens. The adjustment of the eye to see clearly and best at any distance is called accommodation .
The 3rd section is the choroid itself . located between the sclera and the retina, consists of vessels of different diameters and supplies the retina with blood.
3. The inner lining of the eye (retina ). It is a specialized brain tissue located in the periphery. Vision is achieved with the help of the retina. This thin transparent membrane is connected to the other membranes of the eye in only two places: at the serrated edge of the ciliary body and around the optic nerve head. Throughout the rest of its length, the retina is tightly adjacent to the choroid, which is mainly facilitated by the pressure of the vitreous body and intraocular pressure, therefore, when intraocular pressure decreases, the retina can detach. The location where the optic nerve exits the retina is called the optic disc. This disc is visible in the fundus through the transparent structures of the eye. Outside the optic disc there is a rounded yellow spot with a depression in the center. A large concentration of cones is concentrated here. This is a retinal spot. This area determines the visual acuity of the eye, and all other parts of the retina determine the field of vision. The optic nerve passes into the orbit through the optic nerve canal; in the cranial cavity in the area of the optic chiasm, a partial crossing of its fibers occurs. The cortical representation of the visual analyzer is located in the occipital lobe of the brain.
Transparent intraocular media are necessary for the transmission of light rays to the retina and their refraction.
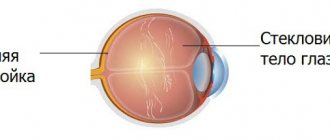
1.Anterior chamber of the eye. It is located between the cornea and the iris. In the corner of the anterior chamber there is a channel through which aqueous humor flows into the venous network of the eye. Impaired outflow leads to increased intraocular pressure and the development of glaucoma.
2. Posterior chamber of the eye. This is the space between the front surface of the lens and the iris. Both cameras communicate with each other through the pupil.
3. Lens . This is an intraocular lens that can change its curvature due to the work of the ciliary muscle. It does not have blood vessels or nerves, and inflammatory processes do not develop here. Its refractive power is 20 diopters. It contains a lot of protein; during a pathological process, the lens loses its transparency. Clouding of the lens is called a cataract. Accommodation is the ability of the human eye to increase its refractive power when moving the gaze from distant objects to near ones, that is, to see well both far and near. The mechanism of the process is associated with the work of the ciliary muscle. Depending on the muscle, these ligaments can stretch or contract, changing the curvature of the lens and its refractive power.
4. Vitreous body . This is the light-conducting medium of the eye, located between the lens and the fundus of the eye. This is a viscous gel that provides turgor (tone) of the eye. The blood supply to the eye and orbit is provided by the ophthalmic artery from the internal carotid artery. Venous drainage is carried out by the superior and inferior ophthalmic veins. The superior ophthalmic vein carries blood to the cavernous sinus of the brain and anastomoses with the veins of the face through the angular vein. The veins of the orbit do not have valves. Consequently, the inflammatory process of the facial skin can spread into the cranial cavity. Sensitive innervation of the eye and orbital tissues is carried out by 1 branch of the 5th pair of cranial nerves.
Most cones are concentrated in the center of the retina, and most rods are located at its periphery. Therefore, a distinction is made between central and peripheral vision. Central vision is provided by cones and is characterized by two visual functions: visual acuity and color perception. Peripheral vision is vision provided by rods (twilight vision) and is characterized by a visual field and light perception.
The appendage apparatus of the eye includes: the orbit, eyelids, conjunctiva, lacrimal and oculomotor apparatus.
The orbit serves as a container for the eyeball and is shaped like a pyramid. The orbit has 4 walls: The inner one is the thinnest, it is formed by the lacrimal bone, the frontal process of the upper jaw, the orbital plate of the ethmoid bone, and the sphenoid bone. Due to the small thickness of the plate, it is called “paper”. Through it, the inflammatory process passes to the orbital tissue. In the posterior part of the orbit there are muscles, fiber, and blood vessels.
The eyelids are movable flaps that cover the front of the eyeball. The top is covered with very thin skin, with loose fiber, eye muscle and cartilage located deeper. Along the edges of the eyelids there are eyelashes, in the thickness of the eyelids there are cartilage glands and sebaceous glands.
Conjunctiva. This is a thin connective tissue membrane. It lines the back surface of the eyelids and the front surface of the eyeball to the cornea, is richly innervated, and performs a protective function. Normally it is pink, smooth, shiny.
The lacrimal apparatus is represented by the lacrimal gland and lacrimal ducts. Tears are produced in the lacrimal gland. This gland occupies the upper outer corner of the eye. From it, the tear enters the conjunctival sac, from there it flows along the lacrimal stream on the lower eyelid to the inner corner of the eye (tear lake), from there through the lacrimal puncta at the inner corner of the eye it enters the lacrimal sac. From there it enters the nasal cavity through the nasolacrimal duct.
The oculomotor system is represented by 2 oblique and 4 rectus muscles. They move the eyeball.
Eye diseases
Removing fragments from the eye using an electromagnet.
1915 The science of ophthalmology studies eye diseases.
There are many diseases that damage the organ of vision. In some of them, the pathology occurs primarily in the eye itself; in other diseases, the involvement of the organ of vision in the process occurs as a complication of already existing diseases.
The first include congenital anomalies of the visual organ, tumors, damage to the visual organ, as well as infectious and non-infectious eye diseases in children and adults.
Eye damage also occurs with such common diseases as diabetes mellitus, Graves' disease, hypertension and others.
Infectious eye diseases: trachoma, tuberculosis, syphilis, etc.
Parasitic eye diseases: eye demodicosis, onchocerciasis, ophthalmomyasis (see Myiasis), thelaziosis, cysticercosis, etc.
Some of the primary eye diseases are:
- Cataract
- Glaucoma
- Myopia (Nearsightedness)
- Retinal detachment
- Retinopathy
- Retinoblastoma
- Colorblindness
- Demodicosis
- Eye burn
- Blennorea
- Keratitis
- Iridocyclitis
- Strabismus
- Keratoconus
- Destruction of the vitreous body
- Keratomalacia
- Eyeball prolapse
- Astigmatism
- Conjunctivitis
- Lens luxation