Structure and functions of the choroid
The choroid has four main parts:
- First part. The outer layer of the choroid is the suprachoroid, it is adjacent to the sclera (the white layer of the eye) and consists of many connective tissue cells, between which pigment cells are located
- The second part, the choroid itself, contains large arteries and veins, which are separated from each other by pigment and connective tissue cells
- The third part is the choriocapillary membrane, consisting of small capillaries; the walls of these vessels allow oxygen, nutrients, as well as breakdown and metabolic products to pass through
- The fourth part is Bruch's membrane. This is a thin plate that is tightly adjacent to the choriocapillary membrane.
The main function of the choroid is trophic, that is, regulating metabolism and providing nutrition to the tissues of the eye. In addition, the choroid performs a number of the following tasks:
- Regulates intraocular pressure
- Participates in thermoregulation of the eye, as it produces thermal energy
- Controls the flow of solar radiation entering the eye
- Delivers substances necessary for the production of visual pigment in rods and cones.
Anatomy of the choroid
- Structure of the choroid
- Structure of choroidal vessels
- Innervation of the choroid
The choroid proper (choroid) is the largest posterior section of the choroid (2/3 of the volume of the vascular tract), along the line from the dentate line to the optic nerve, formed by the posterior short ciliary arteries (6-12), which pass through the sclera at the posterior pole of the eye .
Between the choroid and the sclera there is a perichoroidal space filled with flowing intraocular fluid.
The choroid has a number of anatomical features:
- is devoid of sensitive nerve endings, therefore the pathological processes developing in it do not cause pain
- its vascular network does not anastomose with the anterior ciliary arteries; as a result, with choroiditis, the anterior part of the eye remains intact
- an extensive vascular bed with a small number of drainage vessels (4 vorticose veins) helps to slow down blood flow and settle pathogens of various diseases here
- limited connection with the retina, which in diseases of the choroid, as a rule, is also involved in the pathological process
- due to the presence of the perichoroidal space, it is quite easily exfoliated from the sclera. It is maintained in its normal position mainly due to the draining venous vessels that perforate it in the equator region. Vessels and nerves that penetrate the choroid from the same space also play a stabilizing role.
Functions
- nutritional and metabolic - delivers food products with blood plasma to the retina to a depth of up to 130 microns (pigment epithelium, retinal neuroepithelium, outer plexiform layer, as well as the entire foveal retina) and removes metabolic reaction products from it, which ensures the continuity of the photochemical process. In addition, the peripapillary choroid nourishes the prelaminar region of the optic nerve head;
- thermoregulation - removes with the blood flow excess thermal energy generated during the functioning of photoreceptor cells, as well as when light energy is absorbed by the retinal pigment epithelium during the visual work of the eye; the function is associated with a high blood flow rate in the choriocapillaris, and presumably with the lobular structure of the choroid and the predominance of the arteriolar component in the macular choroid;
- structure-forming - maintaining the turgor of the eyeball due to the blood supply to the membrane, which ensures a normal anatomical relationship between the parts of the eye and the required level of metabolism;
- maintaining the integrity of the external blood-retinal barrier - maintaining a constant outflow from the subretinal space and removing “lipid debris” from the retinal pigment epithelium;
- regulation of ophthalmotonus, due to:
- contraction of smooth muscle elements located in the layer of large vessels,
- changes in the tension of the choroid and its blood supply,
- influence on the rate of perfusion of the ciliary processes (due to the anterior vascular anastomosis),
- heterogeneity in the size of venous vessels (volume regulation);
- autoregulation - regulation by the foveal and peripapillary choroid of its volumetric blood flow with a decrease in perfusion pressure; the function is presumably associated with nitrergic vasodilator innervation of the central choroid;
- stabilization of the level of blood flow (cushioning) due to the presence of two systems of vascular anastomoses, the hemodynamics of the eye are maintained in a certain unity;
- light absorption - pigment cells located in the layers of the choroid absorb light flux, reduce light scattering, which helps obtain a clear image on the retina;
- structural-barrier - due to the existing segmental (lobular) structure, the choroid retains its functional usefulness when one or more segments are affected by the pathological process;
- conductive and transport function - the posterior long ciliary arteries and long ciliary nerves pass through it, and carries out the uveoscleral outflow of intraocular fluid through the perichoroidal space.
The extracellular matrix of the choroid contains a high concentration of plasma proteins, which creates high oncotic pressure and ensures the filtration of metabolites through the pigment epithelium into the choroid, as well as through the supraciliary and suprachoroidal spaces. From the suprachoroid, the fluid diffuses into the sclera, scleral matrix and perivascular clefts of the emissaries and episcleral vessels. In humans, uveoscleral outflow is 35%.
Depending on fluctuations in hydrostatic and oncotic pressure, aqueous humor may be reabsorbed by the choriocapillaris layer. The choroid, as a rule, contains a constant amount of blood (up to 4 drops). An increase in choroidal volume by one drop can cause an increase in intraocular pressure of more than 30 mmHg. Art. The large volume of blood continuously passing through the choroid provides constant nutrition to the retinal pigment epithelium associated with the choroid. Choroidal thickness depends on blood supply and averages 256.3±48.6 µm in emmetropic eyes and 206.6±55.0 µm in myopic eyes, decreasing to 100 µm in the periphery.
The choroid becomes thinner with age. According to B. Lumbroso, the thickness of the choroid decreases by 2.3 microns per year. Thinning of the choroid is accompanied by impaired blood circulation in the posterior pole of the eye, which is one of the risk factors for the development of newly formed vessels. There was significant thinning of the choroid associated with increasing age in emmetropic eyes at all measurement points. In people under 50 years of age, the thickness of the choroid is on average 320 microns. In persons over 50 years of age, the thickness of the choroid decreases on average to 230 microns. In the group of people over 70 years of age, the average choroidal value is 160 µm. In addition, a decrease in choroidal thickness was noted with an increase in the degree of myopia. The average thickness of the choroid in emmetropes is 316 µm, in individuals with low and moderate myopia – 233 µm, and in individuals with high myopia – 96 µm. Thus, normally there are large differences in the thickness of the choroid depending on age and refraction.
Structure of the choroid
The choroid extends from the dentate line to the optic foramen. In these places it is tightly connected to the sclera. Loose attachment is present in the equator region and at the entry points of blood vessels and nerves into the choroid. Throughout the rest of its length, it is adjacent to the sclera, separated from it by a narrow gap - the suprachoroidal space. The latter ends 3 mm from the limbus and at the same distance from the exit point of the optic nerve. Ciliary vessels and nerves pass through the suprachoroidal space, and fluid outflows from the eye.
The choroid is a formation consisting of five layers, the basis of which is a thin connective stroma with elastic fibers:
- suprachoroid;
- layer of large vessels (Haller);
- layer of middle vessels (Sattler);
- choriocapillaris layer;
- vitreous plate, or Bruch's membrane.
On a histological section, the choroid consists of lumens of vessels of various sizes, separated by loose connective tissue; process cells with a crumbly brown pigment, melanin, are visible in it. The number of melanocytes, as is known, determines the color of the choroid and reflects the nature of pigmentation of the human body. As a rule, the number of melanocytes in the choroid corresponds to the type of general pigmentation of the body. Thanks to the pigment, the choroid forms a kind of camera obscura, which prevents the reflection of rays entering the eye through the pupil and ensures a clear image on the retina. If there is little pigment in the choroid, for example, in fair-skinned people, or none at all, as is observed in albinos, its functionality is significantly reduced.
The vessels of the choroid make up its bulk and represent branches of the posterior short ciliary arteries that penetrate the sclera at the posterior pole of the eye around the optic nerve and give further dichotomous branching, sometimes before the arteries penetrate the sclera. The number of posterior short ciliary arteries ranges from 6 to 12.
The outer layer is formed by large vessels , between which there is loose connective tissue with melanocytes. The layer of large vessels is formed mainly by arteries, which are distinguished by the unusual width of the lumen and the narrowness of the intercapillary spaces. An almost continuous vascular bed is created, separated from the retina only by the lamina vitrea and a thin layer of pigment epithelium. In the layer of large vessels of the choroid there are 4-6 vorticose veins (v. vorticosae), through which venous outflow occurs mainly from the posterior part of the eyeball. Large veins are located close to the sclera.
The layer of middle vessels follows the outer layer. It contains much less melanocytes and connective tissue. Veins in this layer predominate over arteries. Behind the middle vascular layer is a layer of small vessels , from which branches extend into the innermost layer - the choriocapillaris layer (lamina choriocapillaris).
The choriocapillary layer dominates over the first two in diameter and number of capillaries per unit area. It is formed by a system of precapillaries and postcapillaries and has the appearance of wide lacunae. The lumen of each such lacuna can accommodate up to 3-4 red blood cells. In terms of diameter and number of capillaries per unit area, this layer is the most powerful. The densest vascular network is located in the posterior part of the choroid, less intense - in the central macular region and poor - in the area of exit of the optic nerve and near the dentate line.
The arteries and veins of the choroid have the usual structure characteristic of these vessels. Venous blood flows from the choroid through the vorticose veins. The venous branches of the choroid flowing into them connect with each other within the choroid, forming a bizarre system of whirlpools and an expansion at the confluence of the venous branches - an ampulla, from which the main venous trunk departs. Vorticose veins exit the eyeball through oblique scleral canals on the sides of the vertical meridian behind the equator - two above and two below, sometimes their number reaches 6.
The inner shell of the choroid is a vitreous plate, or Bruch's membrane , which separates the choroid from the retinal pigment epithelium. Electron microscopic studies show that Bruch's membrane has a layered structure. The vitreous plate contains retinal pigment epithelial cells firmly connected to it. On the surface they have the shape of regular hexagons; their cytoplasm contains a significant amount of melanin granules.
From the pigment epithelium, the layers are distributed in the following order: the basement membrane of the pigment epithelium, the inner collagen layer, the elastic fiber layer, the outer collagen layer and the basement membrane of the choriocapillaris endothelium. Elastic fibers are distributed across the membrane in bundles and form a network-like layer, slightly shifted to the outside. In the anterior sections it is denser. The fibers of Bruch's membrane are immersed in a substance (amorphous substance), which is a mucoid gel-like medium, which includes acidic mucopolysaccharides, glycoproteins, glycogen, lipids and phospholipids. The collagen fibers of the outer layers of Bruch's membrane extend between the capillaries and are woven into the connective structures of the choriocapillaris layer, which promotes tight contact between these structures.
Suprachoroidal space
The outer border of the choroid is separated from the sclera by a narrow capillary gap, through which suprachoroidal plates, consisting of elastic fibers covered with endothelium and chromatophores, go from the choroid to the sclera. Normally, the suprachoroidal space is almost not expressed, but under conditions of inflammation and edema, this potential space reaches significant sizes due to the accumulation of exudate here, pushing apart the suprachoroidal plates and pushing the choroid inwards.
The suprachoroidal space begins at a distance of 2-3 mm from the exit of the optic nerve and ends approximately 3 mm short of the insertion of the ciliary body. Long ciliary arteries and ciliary nerves, enveloped in the delicate tissue of the suprachoroid, pass through the suprachoroidal space to the anterior part of the vascular tract.
The choroid easily moves away from the sclera throughout its entire length, with the exception of its posterior section, where the dichotomously dividing vessels included in it fasten the choroid to the sclera and prevent its detachment. In addition, choroidal detachment can be prevented by vessels and nerves along the rest of its length, penetrating into the choroid and ciliary body from the suprachoroidal space. With expulsive hemorrhage, the tension and possible separation of these nerve and vascular branches causes a reflex disturbance in the general condition of the patient - nausea, vomiting, and a drop in pulse.
Structure of choroidal vessels
Arteries
The arteries do not differ from arteries of other localizations and have a middle muscle layer and adventitia containing collagen and thick elastic fibers. The muscle layer is separated from the endothelium by an internal elastic membrane. The fibers of the elastic membrane are intertwined with the fibers of the basement membrane of endothelial cells.
As the caliber decreases, the arteries become arterioles. In this case, the continuous muscle layer of the vessel wall disappears.
Vienna
The veins are surrounded by a perivascular membrane, outside of which there is connective tissue. The lumen of veins and venules is lined with endothelium. The wall contains unevenly distributed smooth muscle cells in small numbers. The diameter of the largest veins is 300 µm, and the smallest, precapillary venules, are 10 µm.
Capillaries
The structure of the choriocapillary network is very unique: the capillaries that form this layer are located in the same plane. There are no melanocytes in the choriocapillaris layer.
The capillaries of the choriocapillary layer of the choroid have a fairly large lumen, allowing the passage of several red blood cells. They are lined with endothelial cells, on the outside of which lie pericytes. The number of pericytes per endothelial cell of the choriocapillaris layer is quite large. So, if in the capillaries of the retina this ratio is 1:2, then in the choroid it is 1:6. There are more pericytes in the foveal region. Pericytes are contractile cells and are involved in the regulation of blood supply. A feature of choroidal capillaries is that they are fenestrated, making their wall permeable to small molecules, including fluoroscein and some proteins. The pore diameter ranges from 60 to 80 microns. They are covered with a thin layer of cytoplasm, thickened in the central areas (30 μm). Fenestrae are located in the choriocapillaris on the side facing Bruch's membrane. Typical closure zones are revealed between the endothelial cells of arterioles.
Around the optic nerve head there are numerous anastomoses of the choroidal vessels, in particular, the capillaries of the choriocapillary layer, with the capillary network of the optic nerve, that is, the central retinal artery system.
The wall of arterial and venous capillaries is formed by a layer of endothelial cells, a thin basal layer and a wide adventitial layer. The ultrastructure of the arterial and venous sections of the capillaries has certain differences. In arterial capillaries, those endothelial cells that contain the nucleus are located on the side of the capillary facing the large vessels. The cell nuclei with their long axis are oriented along the capillary.
On the side of Bruch's membrane, their wall is sharply thinned and fenestrated. The connections of endothelial cells on the scleral side are presented in the form of complex or semi-complex joints with the presence of obliteration zones (classification of joints according to Shakhlamov). On the side of Bruch's membrane, cells are connected by simply touching two cytoplasmic processes, between which there is a wide gap (backlash junction).
In venous capillaries, the perikaryon of endothelial cells is often located on the sides of flattened capillaries. The peripheral part of the cytoplasm on the side of Bruch's membrane and large vessels is greatly thinned and fenestrated, i.e. venous capillaries may have thinned and fenestrated endothelium on both sides. The organoid apparatus of endothelial cells is represented by mitochondria, lamellar complex, centrioles, endoplasmic reticulum, free ribosomes and polysomes, as well as microfibrils and vesicles. In 5% of the studied endothelial cells, communication between the channels of the endoplasmic reticulum and the basal layers of blood vessels was established.
In the structure of the capillaries of the anterior, middle and posterior sections of the membrane, slight differences are revealed. In the anterior and middle sections, capillaries with a closed (or semi-closed) lumen are quite often recorded; in the posterior sections, capillaries with a wide open lumen predominate, which is typical for vessels in different functional states. Information accumulated to date allows us to consider the endothelial cells of capillaries to be dynamic structures that continuously change their shape, diameter and length of intercellular spaces.
The predominance of capillaries with a closed or semi-closed lumen in the anterior and middle sections of the membrane may indicate the functional ambiguity of its sections.
Innervation of the choroid
The choroid is innervated by sympathetic and parasympathetic fibers emanating from the ciliary, trigeminal, pterygopalatine and superior cervical ganglia; they enter the eyeball with the ciliary nerves.
In the stroma of the choroid, each nerve trunk contains 50-100 axons that lose their myelin sheath when they penetrate it, but retain the Schwann sheath. Postganglionic fibers arising from the ciliary ganglion remain myelinated.
The vessels of the supravascular plate and stroma of the choroid are extremely abundantly supplied with both parasympathetic and sympathetic nerve fibers. Sympathetic adrenergic fibers emanating from the cervical sympathetic nodes have a vasoconstrictor effect.
Parasympathetic innervation of the choroid comes from the facial nerve (fibers coming from the pterygopalatine ganglion), as well as from the oculomotor nerve (fibers coming from the ciliary ganglion).
Recent studies have significantly expanded knowledge regarding the characteristics of the innervation of the choroid. In various animals (rat, rabbit) and in humans, the arteries and arterioles of the choroid contain a large number of nitrergic and peptidergic fibers, forming a dense network. These fibers come with the facial nerve and pass through the pterygopalatine ganglion and unmyelinated parasympathetic branches from the retroocular plexus. In humans, in addition, in the stroma of the choroid there is a special network of nitrergic ganglion cells (positive for the detection of NADP-diaphorase and nitroxide synthetase), whose neurons are connected with each other and with the perivascular network. It is noted that such a plexus is determined only in animals that have a foveola.
Ganglion cells are concentrated mainly in the temporal and central regions of the choroid, adjacent to the macular region. The total number of ganglion cells in the choroid is about 2000. They are unevenly distributed. The greatest number of them is found on the temporal side and centrally. Cells of small diameter (10 µm) are located along the periphery. The diameter of ganglion cells increases with age, possibly due to the accumulation of lipofuscin granules in them.
In some organs, such as the choroid, nitrergic neurotransmitters are detected simultaneously with peptidergic ones, which also have a vasodilating effect. Peptidergic fibers probably arise from the pterygopalatine ganglion and pass into the facial and greater petrosal nerves. It is likely that nitro- and peptidergic neurotransmitters mediate vasodilation when the facial nerve is stimulated.
The perivascular ganglion plexus dilates choroidal vessels, possibly regulating blood flow as intra-arterial blood pressure changes. It protects the retina from damage from thermal energy released when it is illuminated. Flugel et al. proposed that ganglion cells located at the foveola protect from the damaging effects of light precisely the area where the greatest focusing of light occurs. It was revealed that when the eye is illuminated, blood flow in the areas of the choroid adjacent to the foveola increases significantly.
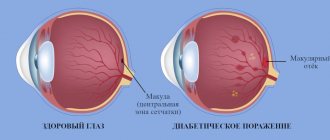
Symptoms of diseases of the choroid
It is not always possible to recognize choroidal diseases in the early stages: symptoms of choroidal diseases may not appear for a long time. However, among the clearly visible signs of pathologies of the choroid are:
- The appearance of flickers and flashes before the eyes
- Decreased visual acuity, blurred image
- Appearance of dark spots
- Distortion of the shape of objects
- Eye redness and pain may occur
The appearance of the above symptoms usually indicates one of the following diseases:
- Uveitis is an inflammatory lesion of the choroid
- Benign formations
- Choroidal detachment
- Traumatic injury.
Pathologies and their symptoms
There are malformations, injuries, diseases, tumors of the S. o. G.
Developmental defects. The most common developmental anomaly of the S. o. g. is kolobo-ma (see). Sometimes underdevelopment of the S. o. occurs. g. – chorioderemia, pigment spots S. o. g., which do not require special treatment.
Damage is observed with penetrating wounds, contusions, and surgical interventions (see Eye, injuries).
Detachment of the S. o. itself. g. can occur with damage to the eye, as well as after abdominal operations on the eyeball (anti-glaucoma, cataract extraction, etc.). At the same time, transudate accumulates in the perichoroidal space, exfoliating the actual S. o. from the sclera. Detachment of the S. o. itself. may also be the result of a blood disorder
treatment in it with a sharp decrease in intraocular pressure.
Wedge, signs of detachment of the S.o. itself. are a decrease in visual functions, a small and uneven anterior chamber of the eyeball, and a decrease in intraocular pressure. With ophthalmoscopy, a gray “bubble” of the exfoliated S. o. itself is visible. d. The diagnosis is made on the basis of a wedge, pictures, perimetry data, ultrasound examination (see.
Ultrasound diagnostics, in ophthalmology) and diaphanoscopy (see). Treatment is conservative: subconjunctival injections of caffeine, dexazone, orally digoxin, veroshpiron, asco-rutin. If there is no effect, surgical treatment is indicated: posterior trepanation of the sclera (see) or sclerotomy (see Sclera) to remove excess perichoroidal fluid. The prognosis with timely treatment is favorable.
Diseases. Inflammatory processes can develop in all parts of the choroid (see Uveitis) or only in its posterior part - posterior uveitis, or choroiditis (see).
Features of the structure and function of S. o. d. determine the uniqueness of inflammatory processes. The abundance of vessels, anastomoses between them, and the wide lumen of the capillaries cause a slowdown in blood flow and create favorable conditions for sedimentation in the system. bacteria, toxins, viruses, protozoa and other pathol. agents.
A large number of pigment cells, histiocytes, the presence of proteins, mucopolysaccharides (glycosaminoglycans) determine the high antigenic organ specificity of the S. o. itself. and creates the prerequisites for the development of allergies during inf. defeats. Immune conflict can manifest itself as delayed-type (more often) and immediate-type allergic reactions.
Tumors. Of the benign tumors, there are neurinomas (see), angiomas, and jevuses (see Neva s, eyes). Choroidal neuromas usually develop against the background of neurofibromatosis (see). Angiomas S. o. g. are observed rarely, they are regarded as a malformation of the vascular system of the eye. As a rule, they are combined with similar abnormalities of the facial skin and mucous membranes.
Malignant tumors of the S. o. g. are divided into primary and secondary. Primary tumors develop from elements of the S. lake itself. g., secondary – with metastasis from the primary focus located in the mammary gland, lungs, gland.-intestinal. tract.
The most common malignant tumor is actually S. o. g. is melanoma (see). To treat malignant tumors, laser coagulation (see Laser), tumor resection, cryodestructive operations (see Cryosurgery) are used, if indicated - radiation therapy, chemotherapy, and sometimes they resort to removal of the eyeball (see Enucleation of the eye).
Excision of the peripheral parts of the S. lake itself. g. in combination with cryotherapy is performed when removing tumors. Dissection of the actual S. o. g. is carried out for introducing various instruments into the eye cavity during the removal of foreign bodies (see), operations on the vitreous body (see), retina (see).
Bibliography: Arkhangelsky V.N. Morphological foundations of ophthalmoscopic diagnosis, p. 132, M., 1960; B u-n and A. Ya. Hemodynamics of the eye and methods of its study, p. 34, M., 1971; In o-dovozov A. M. Light reflexes of the fundus, Atlas, p. 160, M., 1980; Zaitseva N. S. et al. Immunological and biochemical factors in the pathogenesis and rationale for the treatment of uveitis, Vestn. ophthalm., No. 4, p. 31, 1980; Salzmann M.
Anatomy and histology of the normal human eye, its development and decline, trans. with German, p. 53, M., 1913; Kovalevsky E.I. Pediatric ophthalmology, p. 189, M., 1970; aka, Eye diseases, p. 275, M., 1980; Krasnov M. L. Elements of anatomy in the clinical practice of an ophthalmologist, M., 1952;
Multi-volume guide to eye diseases, ed. V. N. Arkhangelsky, vol. 1, book. 1, p. 159, M., 1962; N e-sterov A.P., Bunin A.Ya. and Katsnelson L.A. Intraocular pressure, Physiology and Pathology, p. 141, 244, M., 1974; Penkov M. A., Shpak N. I. and Avrushchenko N. M. Endogenous uveitis, p. 47 and others, Kyiv, 1979; Samoilov A. Ya., Yuzefova F. I. and Azarova N. S.
Tuberculous eye diseases, L., 1963; Fort-schritte der Augenheilkunde, hrsg. v. EB Streiff, Bd 5, S. 183, Basel - NY, 1956; Frangois J., Rabaey M. et Vandermeerssche G. L'ult-rastructure des tissus occulaires au microscope electronique, Ophthalmologica (Basel), t. 129, p. 36, 1955; System of ophthalmology, ed. by S. Duke-Elder, v. 9, L., 1966; Woods A. S. Endogenous uveitis, Baltimore, 1956, bibliogr.
https://www.youtube.com/watch?v=ytpolicyandsafetyru
O. B. Chentsova.
Diagnosis and treatment of choroid diseases
The danger of diseases of the choroid is that disorders may not be noticeable for a long time. Therefore, it is very important to be attentive to your vision, pay attention to even minimal changes in the condition of your eyes and regularly visit an ophthalmologist, 1-2 times a year.
If a disease of the choroid is suspected, the attending physician performs a visual examination, as well as an ultrasound examination.
You can undergo a full diagnostic examination, including the choroid, at the Eye Clinic of Dr. Belikova. We use modern types of research and effective methods of treating eye diseases of varying degrees of complexity.
Anatomy
anatomy of the eye
Actually S. o. extends from the serrated edge (ora serrata) to the optic nerve (see). Outside, it borders on the sclera (see), separated from it by a narrow gap - the perichoroidal space (perivascular space, T.; spatium perichoroide-ale), which is finally formed only by the second half of the child’s life.
The vascular system of the S. o. itself. g. is represented by 8-12 posterior short ciliary arteries (aa. ciliares breves), which are branches of the ophthalmic artery (a. ophthalmica) and penetrate into the S. o. itself. at the posterior pole of the eyeball, forming a dense vascular network. Venous blood from S. o. g. flows through the vorticose veins (vv. vorticosae), which exit the eyeball through oblique canals in the sclera with 4-6 trunks.
Innervates the S. o. d. long and short ciliary nerves (nn. ciliares longi et breves).
Diagnostic methods for lesions of the choroid
To diagnose a specific pathology, it is necessary to conduct an examination including the following methods:
- Ultrasonography;
- Angiography using a photosensitizer, during which it is well possible to examine the structure of the choroid, identify altered vessels, etc.
- Ophthalmoscopic examination includes visual inspection of the choroid and optic nerve head.