Causes
Code according to the international classification of diseases ICD-10:
- H20 Iridocyclitis;
- H21 Other diseases of the iris and ciliary body;
- H30 Chorioretinal inflammation.
The disease is characterized by severe redness of the conjunctiva and deformation of the pupil.
Many different factors can cause the disease. Below we list the main ones:
- allergic reaction, diseases of the autoimmune system;
- eye injuries;
- impaired metabolism, as well as hormonal levels;
- viruses and infections that cause inflammation;
- the presence of fungal microorganisms and parasites;
- sepsis;
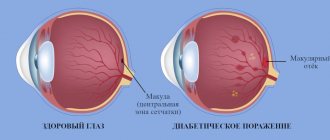
- diabetes;
- chronic inflammatory diseases;
- intoxication of the body;
- the presence of a genetic predisposition.
The disease can occur in people of different ages. In the elderly and children, infectious uveitis is observed in most cases.
Let's make life easier - learn about the causes and treatment of pain in the eyes from the article.
Diabetes mellitus often provokes the development of the disease
In almost half of cases, the disease is caused by pathogenic microorganisms:
- fungi;
- streptococcus;
- toxoplasma;
- treponema pallidum;
- herperviruses.
The disease may be a consequence of a progressive pathology in the body. Most often, the disease is diagnosed in patients with:
- ulcerative colitis;
- psoriasis;
- spondyloarthrosis;
- rheumatoid arthritis;
- multiple sclerosis;
- reactive arthritis;
- autoimmune thyroiditis.
Uveitis is also caused by ophthalmological diseases: conjunctivitis, blepharitis and scleritis.
Psoriasis can also cause uveitis
An effective medication for the treatment of bacterial infections in ophthalmology - instructions for Fucithalmic eye drops.
Kinds
The disease can be classified according to various criteria. Depending on where the disease is located, uveitis is divided into:
- Front. The most common form. It can be divided into cyclitis and iritis. In the first case, the inflammation affects the cicatricial body, in the second - the iris. If both of these elements are affected, then this pathology is called iridocyclitis. During the cold season, the disease may recur.
- Peripheral. In this form, both eyes become infected. Diagnosis is quite difficult, since inflammation affects an area that is difficult to study using standard methods. Namely the central region, retina, choroid, vitreous body.
- Rear. This form develops over a long period of time and appears quite late, since the symptoms are mild and do not worsen the general condition of the patient. Posterior uveitis is complicated by macular ischemia, macular edema, retinal detachment, and retinal vasculitis.
- Diffuse. It is less common than other types and is the most dangerous, since inflammation affects the entire choroid of the eye.
Only an ophthalmologist can accurately diagnose the disease and only using special diagnostic methods (visometry, ophthalmoscopy, visual examination).
When the prescription of Hilabak eye drops is indicated, read here.
Iridocyclitis
Based on the nature of the course, uveitis is divided into:
- Spicy. Occurs for the first time. The symptoms are quite pronounced.
- Chronic. The disease can develop into this form if symptoms persist for a long time and there is no treatment. There is a change in periods of time during which the symptoms worsen and subside.
- Recurrent. In this case, the disease often worsens, and the patient again develops quite pronounced symptoms.
- Sluggish. In this case, the symptoms are mild and may last for more than 2 months.
Let us separately highlight rheumatoid serous uveitis. As a rule, it has a chronic course, the clinical picture is quite blurred. It is a rare form. During the disease, corneal precipitates and posterior adhesions of the iris are formed, the ciliary body is destroyed, and the lens darkens. It lasts quite a long time and is difficult to treat. May be complicated by the development of similar eye diseases.
There are many types of uveitis. In addition to those listed, they are also distinguished according to the nature of inflammation: purulent, exudative, fibrinous-lamellar, mixed type.
First of all, treatment is aimed at avoiding complications that can lead to vision loss.
A broad-spectrum antibiotic from the aminoglycoside group - instructions for Tobropt eye drops.
Diffuse variety
Why daily eye tonometry is performed, find out at the link.
Tuberculous uveitis
The disease is more common in school-age children and older people.
Tuberculous iridocyclitis (anterior tuberculous uveitis)
clinically manifested by mild corneal syndrome and minor mixed injection of the eyeball. Children often do not experience pain. In the iris, in the area of the small arterial circle, against the background of edematous and hyperemic stroma, small grayish-pink nodules the size of a millet grain, surrounded by vessels, can be found. The structure of the nodules is true tubercles. Merging, they can form a conglobed tubercle. Subsequently, reactive inflammation in the tissues around the tubercle leads to the formation of adhesions, fusion and fusion of the pupil.
When the ciliary body is involved in the process, precipitates
. This form of the disease is nodular (granulomatous) uveitis.
In the diffuse form of granulomatous uveitis, the inflammation is plastic in nature. Already at the very beginning of the disease, large “greasy” precipitates are visible. On the pupillary edge of the iris, “guns” resembling flakes of cotton wool appear and quickly disappear. This form of iridocyclitis lasts longer and with frequent relapses.
Gentle opacities appear on the posterior capsule of the lens and in the anterior parts of the vitreous body, and its structure coarsens. In the fundus, mild symptoms of papillitis are detected (hyperemia of the optic disc, some blurring of its contours and vasodilatation).
Nongranulomatous tuberculous uveitis
develop in cases where tuberculous mycobacteria enter the choroid of the eyeball with a well-formed immune system, more often in adults. Bacteria are destroyed in the tissues of the eye, and their breakdown products cause increased tissue sensitivity. Repeated exposure to mycobacteria causes an allergic reaction. The ocular process is characterized by a slight pericorneal injection, hyperemia of the iris, “sweating” of the endothelium and the formation of individual precipitates on the cornea.
In some cases, so-called flying nodules appear on the iris near its pulmonary circulation. They have a round shape, grayish color, disappear relatively quickly and leave no trace behind. Often, opacities of the posterior capsule of the lens and vitreous body come to the fore. Intraocular pressure rises and falls, which is associated with the accumulation and resorption of exudate in the angle of the anterior chamber. Histologically, the process is of the nature of nonspecific inflammation. The disease is sluggish, long-term, with remissions and exacerbations. Opacities in the vitreous body and lens progress, do not resolve, and visual acuity decreases sharply.
Consequently, tuberculous anterior uveitis (iridocyclitis) is most characterized by an inconspicuous onset, a sluggish chronic course, most often affecting one eye, exacerbations and relapses, minor phenomena of irritation, the appearance of newly formed vessels in the iris, the appearance of “fuzzes” on the pupillary edge of the iris and “flying” nodules in the area of its pulmonary circulation, “greasy” precipitates on the endothelium of the cornea, pronounced exudation, wide and powerful posterior adhesions of the iris, massive opacities in the vitreous body, often lesions of the cornea, sclera and lens. There is always a decrease in visual acuity.
Tuberculous choroiditis (posterior tuberculous uveitis) occurs in the form of conglobed tubercle, miliary choroiditis, and diffuse choroiditis.
Conglobed tuberculosis is more common in children with the progressive course of the primary tuberculosis complex in the stage of generalization. At the onset of the disease, inflammatory phenomena may be absent. Then eye irritation appears, sometimes chemosis of the conjunctiva, deposition of precipitates on the posterior surface of the cornea, and exudate in the vitreous body. In the fundus, a grayish-yellowish lesion is found, sometimes up to three times the diameter of the optic disc, located in the choroid. The retina over this lesion becomes cloudy.
With the reverse development of the process, atrophic changes occur in the choroid and retina and round whitish-yellowish lesions with distinct contours and pigment deposition appear. The process may be accompanied by exudative retinal detachment. Depending on the location and extent of damage to the choroid and retina, various visual disorders occur: distortion of objects, scotomas, decreased central vision, narrowing of the boundaries of the visual field, etc. Often, visual impairment is the first sign of the disease.
With miliary tuberculous choroiditis, the eyes are calm in appearance. Ophthalmoscopy reveals pinkish-yellow lesions of different sizes with unclear boundaries, scattered throughout the fundus. The lesions appear simultaneously, and this is a sign that distinguishes this process from disseminated choroiditis, in which they appear in different places at different times. The appearance of tuberculosis is always caused by an outbreak of intrathoracic tuberculosis, and therefore serves as a poor prognostic sign of the general disease. With a favorable course of the main process, chorioretinal lesions quickly undergo reverse development.
In their place, rounded yellowish-grayish atrophic areas of the choroid are formed. Pigment rims do not form, since the retinal pigment epithelium is not involved in the inflammatory process. Other fundus changes in miliary choroiditis include mild hyperemia and blurred outlines of the optic nerve head. Perimetry reveals microscotomas. Patients may notice distortion of the shape of objects (metamorphopsia).
Disseminated tuberculous choroiditis in its clinical course does not differ from miliary tuberculous choroiditis, however, it manifests itself in the absence of an active tuberculous process in the lungs or lymph nodes. Lesions located on the periphery may go unnoticed. The most common occurrence is paramacular localization of lesions involving the retina, which is accompanied by a decrease in acuity and the formation of defects in the visual field.
To diagnose tuberculous uveitis, it is necessary to apply a complex of studies, since it is not always possible to differentiate tuberculous eye damage from a disease of another etiology based on the clinical picture alone.
The complex of diagnostic studies includes:
collection of anamnestic data taking into account contacts with tuberculosis patients and past lung diseases (pleurisy, bronchitis, pneumonia); objective, comprehensive, thorough examination of the eyes (biomicroscopy, ophthalmoscopy, calimetry, angioscotometry, function studies); conducting skin-allergic tuberculin tests (graded Pirquet reaction, Mantoux reaction); general blood test (pay attention to lymphocytosis and monocytosis, ESR) before and after tuberculin tests; study of protein fractions before and after tuberculin tests (pay attention to changes in the content of albumin, a- and γ-globulins); examination of sputum, gastric lavages, cerebrospinal fluid, etc.
A focal test is also carried out in the eye in response to the Mantoux reaction and to the subcutaneous injection of 0.1 tuberculin at a dilution of 1:100000000, i.e., they observe changes in visual acuity, an increase in the blind spot, a decrease in dark adaptation, the appearance of new precipitates, and an increase in swelling of the iris , the formation of new vessels in it, the appearance of exudate in the anterior chamber, increased retinal edema, the appearance of new foci, movement of pigment around the foci, changes in the caliber of retinal vessels, a decrease in intraocular pressure, etc. The appearance of such changes 24-72 hours after intradermal or cutaneous administration tuberculin is evidence of the tuberculous etiology of the process.
The use of focal tests is contraindicated in case of allergies, the presence of an active extraocular lesion, hemorrhagic forms of tuberculous chorioretinitis.
Treatment of tuberculous uveitis is general and local. Due to the high sensitization and intoxication of the body during acute processes, desensitizing nonspecific therapy is carried out before specific therapy and in parallel with it (intravenous infusions of 10% calcium chloride solution, calcium gluconate, suprastin, diphenhydramine, etc.).
Specific therapy consists of intramuscular and subconjunctival injections of streptomycin, oral administration of tubazide or ftivazide, PAS. A 5% saluzide solution is also injected under the conjunctiva. For choroiditis, drugs are injected into the episcleral space, retrobulbar and even into the suprachorionic space. Sometimes tuberculin therapy is performed. The effect is achieved by forced instillation of cyclophosphamide for 3-5 days. Angioprotectors are also used.
Against the background of specific therapy, if there are indications in the subsiding stage, general and local treatment with corticosteroids (cortisone, dexazone) is carried out. Locally - instillations or electro- and phonophoresis of streptomycin, calcium chloride, atropine, dionine, etc.
Proper nutrition is of exceptional importance in the treatment of tuberculous uveitis:
It is necessary to consume foods high in vitamins A, B and C, proteins and fats, as well as a large amount of vegetables and fruits, but limit the intake of table salt and carbohydrates into the body. It is necessary for patients to stay in the fresh air.
After a course of treatment in a hospital for 1.5-3 months, the patient is advised to stay in a sanatorium for 7-9 months, where the course of specific treatment is continued. In the future, for 3 years, it is necessary to carry out an anti-relapse course of treatment lasting up to 4 months in the spring and autumn.
All children and adults with ocular tuberculosis must be registered at a phthisiological dispensary. These patients are treated by an ophthalmologist and a phthisiatrician. Outpatient treatment is free regardless of its duration. All children whose parents have tuberculosis are actively prevented by the use of tubazide (ftivazide), calcium chloride, vitamin and diet therapy, as well as a regime (dry and warm climate). The main measure for early prevention of tuberculosis is vaccinating children with the BCG vaccine.
Symptoms
What the symptoms will be depends on the form and severity of the disease. The main manifestations of anterior uveitis are:
- Pain in the eyes;
- decreased vision;
- blurred vision;
- photophobia;
- hyperemia;
- increased lacrimation;
- feeling of a foreign body in the eye;
- decreased sensitivity of the cornea.
This form has the most striking manifestations. The pupil is narrow, poorly responsive to light and has an irregular shape. Lymphocytes, plasmacides, and pigments accumulate on the cornea and float in the chamber moisture.
In the peripheral form, “floating spots” appear in front of the eyes, and a noticeable decrease in vision is observed. Posterior uveitis is characterized by the absence of symptoms at the onset of the disease; vision decreases gradually. The diffuse form can combine all the symptoms.
In addition to the above, headaches, increased intraocular pressure, itching and burning, distortion of objects, and purulent discharge may be added.
If the patient ignores the first symptoms, the color of the iris will subsequently change and degeneration will occur; ultimately, everything may end in disintegration.
An effective antiglaucoma drug is Travatan eye drops.
Pain in the eyes may be a consequence of the development of the disease
How to recognize the onset of central retinal vein thrombosis is described in detail in the article.
Uveitis in sarcoidosis
Sarcoidosis, or Besnier-Beck-Schaumann disease
, occurs in the form of chronic generalized benign granulomatosis of unknown etiology. With this disease, there is an increase in all (especially endothoracic) lymph nodes, small flat, often pinkish-purple infiltrates; reversible destructive lesions in the bones; iridocyclitis; swelling of the parotid gland; the liver and spleen are involved in the pathological process; leukopenia, lymphopenia, eosinophilia and monocytosis are often detected. The prognosis is favorable. It should be noted that eye disease may precede general symptoms in 1/3 of patients.
Sarcoid iridocyclitis is characterized by a painless course with mild inflammatory phenomena and early formation of posterior adhesions of the iris. A typical picture is of granulomatous iritis, in which the nodules are usually located superficially, but can also be located deep in its stroma. They are bright pink in color, equipped with a large number of vessels, and have irregular outlines, which distinguishes them from miliary nodules in tuberculous eye lesions.
With an almost asymptomatic course of the inflammatory process without a pronounced pericorneal injection, exudate in the anterior chamber, “greasy” precipitates and opacities of the vitreous body appear, as a result of which visual acuity sharply decreases. The development of posterior adhesions of the iris, closure of the pupil area with an exudative film, atrophy of the iris, consistent cataracts, and possible secondary glaucoma are observed. The cornea may be involved in the process, resulting in the development of keratitis with various clinical manifestations. The choroid and retina are affected much less frequently in sarcoidosis.
Small or large lesions appear along the periphery of the fundus, resembling an intraocular tumor in clinical picture. Periphlebitis of the retinal vessels may develop with their blockage and extensive hemorrhages into the vitreous body. Damage to the optic nerve in sarcoidosis manifests itself as neuritis or congestion.
Determining the etiology is difficult. The diagnosis of sarcoidous uveitis is confirmed by the results of a pathomorphological study (biopsy of a lymph node, nodule). To establish a diagnosis, it is important to have characteristic changes in the lungs, cough, joint pain, and typical skin rashes. Treatment consists of general and local use of corticosteroids in combination with desensitizing, anti-inflammatory and antibacterial therapy.
With heterochromic Fuchs cyclitis, the trabecular architecture of the iris disappears, movement of the pigment in it is observed, spot-like atrophy of the pigment epithelium occurs, a grayish-white spongy exudate is formed in the corner of the anterior chamber and multiple small gray non-pigmented precipitates with jagged edges along the entire posterior surface of the cornea. Destruction of the pigment layer of the iris is pronounced.
The pigment at the pupillary edge appears to be moth-eaten. Pigmentation is noted in the corner of the anterior chamber. There is no iris vascularization or posterior commissures. Diffuse opacification of the vitreous body is observed in the form of whitish round inclusions. In almost all cases, the lens gradually becomes cloudy, and secondary glaucoma often develops. The disease is most often unilateral, but can also be bilateral.
Etiology
The etiology of the disease is unknown.
It has been suggested that chronic irritation of the sympathetic nerve plays a major role in the development of the disease. Cases of heterochromia have been described in children whose mothers were exposed to radiation during pregnancy. Chronic viral infection is considered important in the occurrence of the disease, since patients suffering from uveitis of viral etiology often experience sector-shaped heterochromia.
Treatment of the disease is symptomatic and consists of the use of salicylates, corticosteroids, and absorbent agents.
Diagnostics
Recognizing the disease is not so difficult, since clinics are equipped with modern equipment. To make an accurate diagnosis, in addition to visual examination, use:
- ultrasound examination of the eyes;
- biomicroscopy;
- retinoscopy;
- gonioscopy;
- tonometry;
- ultrasonography;
- angiography;
- fluorescein angiography of the retina;
- rheoophthalmography;
- electroretinography;
- anterior chamber paracentesis;
- vitreal and chorioretinal biopsy.
It is also necessary to identify the true source of uveitis. To do this, the patient is examined, studies and tests are prescribed in order to collect as much data as possible and get the most accurate picture.
Very often uveitis is accompanied by headache
The medicine for mydriasis is Tropicamide eye drops.
Goldmann gonioscope will help to diagnose
A serious approach to glaucoma therapy - read the instructions for Trusopt eye drops here.
Uveitis in Reiter's syndrome
Reiter's syndrome (conjunctival-urethrosynovial syndrome) is characterized by a triad of symptoms:
urethritis, conjunctivitis, polyarthritis. It is believed that the causative agent of the disease is a virus. The disease most often manifests itself as follicular bilateral conjunctivitis. Keratitis, iritis, iridocyclitis, and neuroretinitis may develop. Iridocyclitis most often occurs acutely with severe photophobia, lacrimation, and abundant serous exudation into the anterior chamber. The course of uveitis is chronic; relapses are often observed, which can be more severe than the initial disease.
Differential diagnosis is made with Behçet's disease. Treatment is symptomatic, local and general (mydriatics, nonspecific desensitizing therapy, corticosteroids). For conjunctiva, ophthalmic ointment (tetracycline or erythromycin) is used topically, and sometimes general sulfonamide therapy is carried out.
Treatment
It is worth noting that the article is for informational purposes and before starting treatment, consultation with a specialist is necessary. Treatment of uveitis is selected for each patient individually based on the type and course of the disease. Therapy is divided into traditional, surgical and folk.
Under no circumstances should you self-medicate.
To help young mothers - how to treat stye on a child’s eye.
Immunosuppressant
In the first case, drugs that resolve inflammatory infiltrates are first used. The following is used as drug therapy:
- Antimicrobials, antibiotics. They can be administered intramuscularly, intravenously, intravitreally, or by administering the drug under the conjunctiva. These agents are selected based on the type of pathogen.
- Drugs against viruses. They are used for viral uveitis locally by mouth or by injection. The most used drugs are: Acyclovir, Zovirax. Together with them, Viferon and Cycloferon are prescribed.
- Anti-inflammatory drugs included in the groups of non-steroidal anti-inflammatory, cytostatic, glucocorticoid drugs. The following are used as eye drops: Prenacid, Dexapos; for oral administration – Ibuprofen, Indomethacin.
- Immunosuppressants are used in cases of ineffective use of anti-inflammatory drugs. These drugs act on immune reactions, inhibiting them. This is Cyclosporine, Methotrexate.
- In order to prevent the formation of adhesions, the following are prescribed: Atropine, Cyclopentolate, Tropicamide. They help relieve spasm of the ciliary muscle.
- Allergy remedies. The most common are Suprastin and Claritin.
- Vitamins.
Physiotherapeutic treatment is prescribed only after all inflammatory processes have subsided. Specific methods used are: vacuum pulse massage, electrophoresis, phonophoresis, etc.
Surgical treatment is prescribed in extreme cases, as well as when complications occur. In this case, surgical dissection of the adhesions between the lens and the iris of the eye occurs, the vitreous body, glaucoma, cataracts, and eyeball are removed, and the retina is soldered with a laser. The outcome of such operations is not always favorable; the inflammatory process may worsen.
Traditional medicine cannot replace basic treatment and should only be used with the approval of a doctor. Most often, decoctions of medicinal plants are used as eye washes and lotions. Every day the eyes are treated with a weak solution of potassium permanganate.
Effective for herpetic nature of the disease
An antihistamine that can be taken for a long time without interruption
Viral uveitis (Part 1) | Pathology of the choroid
Description
In the last two decades, the incidence of uveitis of viral etiology has increased in all age groups.
The incidence of viral uveitis ranges from 3 to 80%. This is explained by age, genetic, social, territorial characteristics, as well as the diagnostic capabilities of healthcare institutions. Uveitis due to viral infections is associated both directly with the action of the virus and with infectious and toxic-allergic reactions
The ability to cause uveitis has been established in many DNA and RNA containing viruses. These are herpes simplex viruses types 1 and 2, cytomegalovirus, herpes zoster virus, Epstein-Bar virus, influenza viruses, parainfluenza, measles, rubella, mumps, adenoviruses, lymphocytic choriomeningitis viruses , chickenpox, human T-cell leukemia, hepatitis B, hemorrhagic fevers
Over the past 20 years, uveitis caused by enteroviruses ECHO 11 and ECHO 19, as well as uveitis in AIDS, caused by the human immunodeficiency virus (HIV), have been described.
Uveitis in HIV infection. The first case of AIDS was described in May 1981 in the USA. Since that time, the incidence of HIV infection has grown exponentially.
In the history of mankind, there has never been such a massive pandemic that developed in such a short time. Currently, more than 40 million people are infected with HIV. Of the 6,000 new cases of HIV infection registered daily, according to WHO, half are among adolescents.
HIV was described in 1983 simultaneously in France and the USA. This virus from the group of retroviruses has very high variability. Currently, several main types of HIV have been described. HIV is unstable in the external environment, so its transmission is possible only when tissues and mucous membranes are damaged. HIV is transmitted through the blood of an infected person.
Currently, the main route of HIV infection is the use of medical instruments contaminated with infected blood. Infection is possible through sexual contact, through drugs and blood components, from an infected mother transplapentarly and during childbirth.
Ophthalmological manifestations of AIDS are uveitis, retinovasculitis, neuroretinitis. Optic neuritis is largely associated with autoimmune reactions. In more than 80% of cases, AIDS begins asymptomatically. Some patients develop lymphadenopathy with fever after HIV infection. Suspicion of AIDS is caused by a symptom complex that includes weight loss, fever, profuse sweating, widespread lymphadenopathy and recurrent infections.
In many patients, symptoms of damage to the central nervous system predominate. Among opportunistic infections, the most commonly observed are cytomegatovirus infection, herpes, toxoplasmosis, histoplasmosis, and fungal diseases. Tumors often occur, in particular Kaposi's sarcoma is typical.
In children, the earliest symptom of HIV infection is a primary lesion of the nervous system—autoimmune acute aseptic meningitis. progressive HIV-associated encephalopathy. It includes developmental delay, muscle hypertension, microcephaly, and basal ganglia calcification.
Clinical manifestations of eye damage directly related to HIV infection and pathological conditions due to immunodeficiency - opportunistic diseases, in most cases have common features and require special additional diagnostic methods. Uveitis is quite common in patients with HIV infection. The prevailing picture is iridocyclitis with symptoms of retinitis, which indicates the autoimmune nature of the inflammatory process.
The phenomena of angioretinovasculitis are observed in almost 50-70% of patients. The most typical are cotton wool-like exudates, retinal hemorrhages, and microaneurysms of retinal vessels.
The frequency of these changes increases if there are less than 100 T lymphocytes per 1 ml of blood. HIV-associated retinomicroangiopathy is usually asymptomatic and transient. However, with pronounced changes, it leads to the development of optic nerve atrophy, the appearance of scotomas in the visual field, loss of color vision, and decreased contrast sensitivity.
Cytomegalovirus chorioretinitis occurs in 30-40% of HIV-infected people, usually with a lymphocyte count of less than 100 per ml, which indicates severe immunodeficiency. In the clinic of retinitis, the phenomena of retinovasculitis with hemorrhages predominate. The optic nerve is affected in 5% of cases (neuritis and neuroretinitis).
Antiretroviral therapy in recent years has led to a decrease in the incidence of cytomegalovirus chorioretinitis, and in some cases to its milder course and even spontaneous recovery.
Chorioretinitis caused by the herpes zoster virus ranks 2nd among the causes of necrotizing retinitis in HIV-infected people (up to 4%). Retinitis quickly develops and generalizes with involvement of the deep layers of the retina, damage to the second eye, often with retinal detachment, and rapid and significant loss of vision. Local and general therapy for this disease is long-term, including the combined use of acyclovir and ganciclovir or foscarnet. Toxoplasmic retinochoroiditis develops in 1-2% of patients with HIV infection. Both eyes are affected and multiple lesions develop. In 30-50% of cases, the nervous system is also affected.
Syphilitic uveitis occurs in 2% of AIDS patients. Most cases of choroiditis reported in the literature were identified at autopsy, reflecting the severity of systemic infectious complications.
In HIV-infected, weakened children in the first months of life, against the background of interstitial pneumonia caused by the protozoan Pneumocystis carini, choroiditis caused by this infection often occurs.
Treatment of eye damage in AIDS includes the fight against HIV, symptomatic treatment of eye pathology, treatment of opportunistic infections and diseases.
Specific treatment includes antiviral and immunomodulatory therapy. In recent years, many new drugs have appeared, and attempts are being made to develop a vaccine against AIDS.
More than 30 drugs with antiviral activity are known: zidovudine (Retrovir, azidothymidine), ribavarin. foscarnet, etc. Indications for prescribing retrovir are a decrease in the level of T-helper cells below 250-500 in 1 ml. The use of retrovir within 24 hours after suspected infection is promising as disease prevention.
Doses depend on the condition of the patients and laboratory parameters and range from 500 to 1500 mg per day. Retrovir and its analogues block reverse transcriptase (a retroviral enzyme that promotes the penetration of viral RNA into the genomic material of a human cell), thereby stopping the formation of proviral RNA.
Immunostimulants are used in the treatment of AIDS. These are alpha and beta interferons, granulocyte-macrophage colony-stimulating factor, intravenous administration of immunoglobulins. Recombinant cytokines, hematopoietic growth factors, and erythropoietin are used, which also makes it possible to reduce the toxic effect of antiviral drugs on the bone marrow and, accordingly, increase the doses of chemotherapeutic agents.
Enteroviral uveitis caused by ophthalmotropic strains of the ECHO 19 and ECHO 11 viruses. Enteroviral uveitis is a new and relatively little-studied form of endogenous uveitis, observed exclusively in young children. The etiological role of enteroviruses in the development of uveitis was first established in 1980-1981. when more than 700 cases of unknown infection with uveitis occurred in Krasnoyarsk and the Krasnoyarsk Territory.
Epidemiological studies have shown that the disease occurs exclusively in young children: 88-91% of patients are children of the 1st year of life. Enteroviral uveitis usually develops against the background of another disease (pneumonia, sepsis, acute intestinal infection, acute respiratory infection, etc.), and infection occurs more often as a result of nosocomial contacts.
The infection spreads by airborne droplets and fecal-oral routes, the incubation period is 4-7 days. Diseases occur throughout the year with a predominance in the autumn-winter months.
The disease begins acutely, manifested by a deterioration in general condition, fever up to 38 ° C and above, symptoms of intoxication, enlarged lymph nodes, usually cervical and occipital, moderate catarrhal symptoms. gastrointestinal disorders such as enteritis, polymorphic maculopapular, quickly disappearing rash, slight enlargement of the liver in diarrhea patients and the spleen in a third of children (without compromising their functions), the development of uveitis
Uveitis develops on the 1-10th (usually on the 3-5th) day after identifying symptoms of an infectious disease, occurs in the form of acute iridocyclitis and in 60-70% of cases is unilateral Signs of eye irritation are mild, especially in children under 3 months , sometimes there is slight hyperemia of the conjunctiva of the eyelids with slight serous discharge
The leading symptoms of uveitis are hyperemia and swelling of the iris, its darkening due to diffusion and deposition of pigment on the anterior surface, narrowing and rigidity of the pupil. In 25-30% of cases, endothelial edema is observed, and no precipitates are formed.
Uveitis quickly leads to the development of focal destruction of the pigment layer and stroma of the iris of varying degrees (from the destruction of the pigment border and the formation of single defects of the pigment layer to subtotal iridolysis)
Posterior synechiae are often pigmented; early formation of prelenticular films is observed. Cyclitis is manifested by exudation into the anterior layers of the vitreous body, small gray-yellow foci in the area of the flat part of the ciliary body and hypotension. In 25% of cases, swelling of the optic nerve head is observed; macular edema and exudate in the retinal area are less common.
The course of enteroviral uveitis varies from mild (7-14 days) to severe (2-3 months) with the development of gross changes in the anterior segment of the eye, persistent hypotension, resulting in subatrophy of the eyeball in isolated cases. Relapses are observed in 10% of cases in the first 6 months from the onset of the disease. At a later date, relapses are rare.
Against the background of clinical remission in enteroviral uveitis, destruction of the iris continues, clouding of the lens develops, often followed by resorption of the lens substance, and secondary glaucoma develops. Uveitis caused by the ECHO 11B virus is the most severe: prolonged hypotension, recurrent hyphemas, retinal hemorrhages, successive cataracts are observed in a third of patients, and in a third of cases, prelenticular films are formed after 2-3 months.
Persistent intraocular enterovirus infection plays a role in the pathogenesis of late complications of uveitis. The diagnosis of enteroviral uveitis is made based on the detection of high titers of neutralizing antibodies to the causative virus in the serum and the detection of viral antigen in scrapings from the conjunctiva.
Treatment. In the acute period of enteroviral uveitis, active long-term (1-1.5 months) antiviral therapy using interferons, interferonogens, and globulin drugs is advisable, which can reduce the likelihood of developing a persistent enteroviral infection.
In the early stages (up to 6-8 months), when membranes form in the optical zone and the angle of the anterior chamber, it is advisable to prescribe absorbable therapy (collalysin, topical lidase 2-3 courses). In case of subatrophy or retarded growth of the eyeball, progression of destruction of the iris, corneal dystrophy, partial cataracts, dystrophic changes in the retina and optic nerve head, treatment is aimed at improving the trophism of the eye.
For children who have had enteroviral uveitis, early detection and correction of refractive errors are indicated, and with the development of refractive or obscuration amblyopia, pleoptic treatment. In cases of cataracts and/or dense lens film that reduce visual acuity, surgical treatment is performed.
Contraindications to surgery are a pronounced reduction in the eyeball (antero-posterior size less than 15 mm), hypotension (less than 14 mm Hg), severe fibrosis of the vitreous, retinal detachment, especially with unilateral lesions.
The optimal time for surgical intervention is 6-8 months after the development of cataracts with stable remission of uveitis. since longer visual deprivation at an early age leads to poor functional treatment results. Excision of the retrocorneal membrane is carried out for optical or organ-preserving purposes within a period of up to 1 year of the membrane’s existence, since secondary opacification of the cornea subsequently develops.
When intraocular pressure increases and drug therapy is ineffective, surgical interventions on the drainage system of the eye are indicated. Due to the development of intraocular persistent enteroviral infection, accompanied by the progressive formation of severe complications, all children who have had enteroviral uveitis should be constantly under medical supervision, identifying risk groups for the development of various clinical forms of complications, primarily secondary glaucoma.
Herpetic uveitis (uveitis caused by herpes simplex virus types 1 and 2. Herpes simplex virus (HSV) is the most common cause of viral uveitis. Herpetic keratoiridocyclitis is more common. The possibility of herpetic uveitis in the form of isolated peripheral uveitis and panuveitis has been established.
Herpetic isolated chorioretinitis is most often congenital and caused by HSV type 2. It is possible for a child to be infected with HSV in utero, as well as during different periods of postnatal development.
There are various changes in the eyes - conjunctivitis, keratitis, cataracts, chorioretinitis, panuveitis. They are combined with skin rashes, but can also be isolated. The syndrome of intrauterine HSV infection is similar to congenital toxoplasmosis and cytomegalovirus infection and includes microcephaly, brain calcifications, mental retardation, and disseminated chorioretinitis. Children with intrauterine HSV infection often experience zoster-like skin rashes at birth, and sometimes keratitis is detected, which can be a recurrence of infection at birth.
Chorioretinitis with herpetic infection can be congenital. It is accompanied by severe retinal damage with massive yellowish-white exudate, reaction of the adjacent vitreous body and perivasculitis. The inflammatory process can be localized in the posterior pole, but the foci are more often located in the equatorial zone.
During recovery, chorioretinal scars with pigmentation form, as with toxoplasmosis. In severe cases, chorioretinitis becomes necrotizing.
Acquired herpetic uveitis often occurs as keratouveitis. Isolated iridocyclitis is a serous or serous-fibrinous process and can be acute, subacute and sluggish.
With indolent herpetic iridocyclitis there is no pain in the eye. There are mild pericorneal injection, polymorphic grayish precipitates, sometimes “greasy”, changes in the color and pattern of the iris, focal atrophy of the predominantly mesodermal layer in the area of granulomas (agrophic spots of the iris), posterior synechia, goniosynechia, vitreous opacities and hypertension.
With herpetic iridocyclitis, retinal perivasculitis, peripapillary and perivascular edema of the retinal vessels, and hemorrhages along the veins may occur. Such vasculitis leads to serous papilledema and serous maculitis.
With relapses and exacerbations of the disease, changes in the cornea characteristic of herpes may appear. Diagnosis of herpetic iridocyclitis is extremely difficult due to the lack of a clear and specific clinical picture
Focal chorioretinitis is rare. Fresh light yellow lesions can occur with recurrent herpes against the background of old choroidal lesions bordered with pigment. The sensitivity of the cornea of the patient, and sometimes of the healthy eye, is absent or sharply reduced.
The etiological diagnosis of herpetic uveitis is made on the basis of a characteristic clinical picture, active keratitis or residual changes after it, decreased sensitivity of the cornea and based on the results of laboratory and clinical laboratory diagnostic methods.
One of the most convenient rapid diagnostic tests is to detect the herpes virus antigen in a scraping of the conjunctiva of the affected eye using the fluorescent antibody (MFL) method. The appearance of specific antibodies and antibodies to very early proteins is important for diagnosis.
The most reliable and sensitive diagnostic test remains an intradermal focal test with a herpetic polyantigen (herpetic polyvaccine). For therapeutic purposes, the vaccine is administered intradermally at 0.01-0.05 ml with an interval of 3 days. Conducting focal tests is not advisable in acute uveitis.
Treatment should be comprehensive and include the use of antiviral and immunotropic drugs, non-steroidal anti-inflammatory drugs, angioprotectors and symptomatic drugs. According to indications, laser coagulation of chorioretinal lesions is performed.
Antiviral treatment is carried out in several directions.
The chemotherapy drug acyclovir is used. virolex. Zovirax in drops, ointments, injections under the conjunctiva, parabulbar, intravenously; 0.1% solution of hydroxuridine (kerecid, etc.) and as part of ophthalmic medicinal films; 0.25-0.5% florenal ointment, gossypol, 0.5% bonafton ointment during the period of viremia; Poludanum in instillations and for administration under the conjunctiva, etc.
Interferon and interferonogens are indicated: concentrated interferon (50,000 units/ml) for administration under the conjunctiva, 0.2-0.5 ml daily or every other day, for a total of 5-10 injections, as well as in the form of forced installations. Interferonogens include pyrogenal, polyacrylamide, prodigiosan, poladan. A solution of pyrogenal is prescribed at a concentration of 100 μg/ml in instillations, prodigiosan intramuscularly according to the scheme; Poludanum in instillations and under the conjunctiva, 0.3-0.5 ml. Interferonogens can be used in the form of phonophoresis. It is advisable to combine the administration of interferon and interferonogenic drugs.
Gamma globulin (anti-influenza, anti-measles) is used in the form of forced installations and for administration under the conjunctiva, 0.2-0.5 ml 2 times a week in combination with intramuscular administration.
Vaccination with herpes vaccine is carried out during the inter-relapse period in order to prevent relapses of the disease and stimulate the immune system. Vaccination increases the production of immunoglobulin A. stimulates cellular immunity, reduces sensitization to HSV
In order to stimulate cellular immunity, which plays an important role in protection against viral infections, levamisole is used orally in tablets of 20-50 mg/day in 1 or 2-3 doses, 3 days a week for 4-5 weeks. Other drug prescription regimens are also possible.
Nonsteroidal anti-inflammatory drugs butadione, brufen, etc. are prescribed in age-specific doses. Corticosteroid drugs (0.4% dexamethasone solution under the conjunctiva 0.2-0.5 ml daily or every other day. 0.1% dexamethasone phosphate eye drops, as well as this drug in the form of electrophonophoresis) are widely used in the treatment of viral uveitis under cover antiviral agents.
Cytomegalovirus uveitis can be congenital or acquired. Infection of the fetus occurs at different stages of intrauterine development, since the virus easily penetrates the placenta, as well as when passing through the birth canal. At an early age, infection of children increases slowly, but in the first school years it quickly reaches 40-80%.
Eye damage with congenital cytomegalovirus infection can be part of the syndrome, as well as isolated. Congenital cytomegalovirus infection syndrome includes jaundice with splenomegaly, prematurity, thrombocytopenia, pneumonia, central nervous system lesions, and mental retardation.
Eye changes are most often represented by chorioretinitis; other lesions are also found: dacryocystitis, conjunctivitis, keratitis, scleritis, cataracts, atrophy and congenital defects of the optic nerve, retinal hemorrhages, perivascular retinal exudate.
Chorioretinitis in children with congenital cytomegalovirus infection is often combined with damage to the central nervous system and brain calcifications.
Chorioretinitis with cytomegalovirus infection is similar to toxoplasmosis and manifests itself in the form of large chorioretinal lesions in the posterior pole of the eye (Fig. 69, see incl.). In the acute phase of the disease, the lesions are grayish-white in color and extend into the vitreous body with significant effusion into it and hemorrhages into the retina. In the scarring stage, lesions differ from toxoplasmosis lesions in less pronounced pigmentation.
Congenital uveitis can be in the form of iridocyclitis or panuveitis, ending at the time of birth or during the first months of life.
To diagnose cytomegalovirus infection, virus isolation is used in cell cultures from saliva, urine and eye tissue. Express diagnostics include detection of the virus antigen in scrapings of the conjunctiva and eye tissue using the fluorescent antibody method.
Information about the cellular and humoral response of the body to a viral infection is provided by the blast transformation reaction with the cytomegalovirus antigen, as well as the indirect hemagglutination reaction
For the treatment of cytomegalovirus chorioretinitis, ganciclovir, foscarnet, cidovir, etc. are used; they are prescribed orally and administered intravenously and into the vitreous body.
Influenza uveitis
. Conjunctivitis is most typical for influenza; keratitis, iridocyclitis, panuveitis, neuroretinitis, and vitreous hemorrhages are also possible. The process arises and proceeds acutely, with pronounced subjective phenomena and pain. Pericorneal injection is pronounced, serous exudate may appear in the anterior chamber, and small precipitates are deposited on the endothelium of the cornea.
Fusion of the pupillary edge of the iris with the anterior capsule of the lens quickly occurs in the form of separate pigmented posterior synechiae and opacification of the vitreous body. The outcome is often favorable, but relapses are possible. As a rule, one eye is affected. Detection of influenza viral antigen in conjunctival scrapings using immunofluorescence. like its absence, does not always serve as a basis for the etiological diagnosis of uveitis, but it is necessary to take these data into account.
Information about high titers of antibodies to influenza A and B viruses in these patients should be taken into account. Treatment of eye damage due to influenza depends on the nature and severity of the disease. Antiviral agents are recommended for topical use: acyclovir, Zovirax. virolex, leukocyte interferon in the form of forced installations and subconjunctival injections; eye ointments: florenal 0.5%, bonafton 0.5%, tebrofen 0.5%.
When a secondary bacterial infection occurs, a 10% solution of sulfapyridazine is additionally prescribed into the conjunctival cavity;
Symptomatic treatment is aimed at dilating the pupil and relieving pain (anaesthetics, dry heat). Uveitis in Behcet's syndrome
. Ophthalmostomatogenital syndrome, described by Behçet in 1937, is a severe viral disease and is manifested by recurrent iridocyclitis with hypopyon, aphthous stomatitis and ulcerative lesions of the mucous membranes and skin of the genital organs. The disease is more common in males. Symptoms of uveitis may appear at different times.
The inflammatory process in the anterior part of the choroid is characterized by an extremely severe course and is complicated by neuroretinitis, exudative chorioretinitis, and retinal periphlebitis. The disease is acute, bilateral; A hypopyon quickly appears, powerful posterior synechiae are formed, the pupil becomes overgrown, and subsequently secondary glaucoma occurs.
Vitreous opacities are evident. The process often recurs and often ends in blindness. Treatment consists of local and general anti-inflammatory therapy: broad-spectrum antibiotics, corticosteroids hydrocortisone or dexamethasone (Dexasone) are prescribed in the form of forced instillations of 0.1% solutions, retrobulbar injections of 0.3 ml, 0.4% solution of prednisolone or dexamethasone; tissue therapy, vitamins, mydriatics, anesthetics, enzymes, etc. are indicated.
To combat swelling of the optic nerve that occurs with neuroretinitis, dehydration therapy is used (25% magnesium sulfate solution 5 ml intramuscularly, 1% Lasix solution 0.2 ml intramuscularly or furosemide 1 time per day).
Dehydration is carried out on average 12-15 days. In order to stimulate lytic processes in the rupture of newly formed posterior synechiae and the resorption of opacities in the vitreous body, fibrinolysin is used in the form of forced instillations. In case of positive RSC with toxoplasmosis antigen (a number of authors consider Behçet's disease in connection with toxoplasmosis, staphylococcal infection, weakening of the immune system), anti-toxoplasmosis chemotherapy is performed: chloridine in age-related doses 2 times a day, sulfadimezin 0.5 g 4 times a day orally, folic acid acid.
Prognosis and prevention
Preventive measures include:
- Compliance with personal hygiene rules (daily eye care, use of a personal towel, etc.)
- Avoiding hypothermia;
- Prevention of eye injuries;
- Timely treatment of various diseases, especially ophthalmological, as well as allergic reactions.
If the treatment was comprehensive and timely, the recovery process takes no more than 6 weeks. The prognosis is less favorable if a complication of uveitis occurs, namely, cataracts, glaucoma, heart attack, retinal detachment or dystrophy develop, in which case blindness may occur.
Chronic uveitis is prone to relapses due to a general decrease in immunity.
GCS for local use in ophthalmology
Most often, the reason lies in the uncontrolled proliferation of streptococcus
Uveitis in children
In children, the disease can be caused by food allergies, vaccinations, and also occur through blood transfusions. Most often, infectious-allergic inflammation of the choroid is observed in children with impaired metabolism.
Treatment is similar to therapy in adults; it is necessary to carefully select drugs according to age and the form of the disease.
Metabolic disorders in babies can manifest themselves in the development of uveitis
Even the slightest redness of the eyes, itching, decreased vision, etc. should arouse suspicion. In this case, it is necessary to immediately consult a doctor, because the sooner treatment is started, the higher the prognosis for a favorable outcome.