Did you know that our eye has a protective layer of tissue that protects our eye from various microbes and foreign bodies getting there? Nerve fibers and muscles are attached to this protective sheath. The outer, densest layer of tissue is the conjunctiva, followed by the thin and transparent episclera and the inner, less dense part - the sclera (or white of the eye).
If the choroid of our eye is damaged by tuberculoma, granuloma and other similar infections, diseases of the upper layers of the sclera are possible.
Scleritis and episcleritis are inflammation of the superficial layers of the outer layer of the eye.
1
Structure of the eye and eyeball
2 Episcleritis
3 Treatment of scleritis
The structure of the sclera
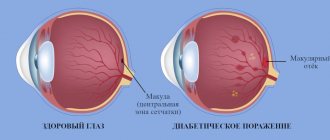
The picture shows a diffuse form of scleritis.
There are three layers in the eyeball: the inner retina, the middle vascular layer, and the sclera. The sclera is the outer layer of the eye and consists of chaotically arranged connective tissue fibers, which gives it a corresponding white color.
Directly contacts the following structures of the eye:
- ciliary body;
- cornea;
- iris;
- choroid.
It should be understood that the inflammatory process will spread to these formations primarily due to their anatomical proximity.
The outer shell itself also has three layers:
- superficial - episclera, which is represented by loose tissue; it has a rich network of blood vessels;
- middle - directly to the sclera, consists mainly of collagen fibers forming a tight bond;
- the inner layer is a dark or brown layer, which got its name due to the large number of cells that contain pigment substances - chromatophores.
Outside, the sclera is covered with a thin, transparent conjunctiva, consisting of stratified columnar epithelium.
Despite its small thickness, up to 1 millimeter, scleral tissue is relatively strong, which helps it perform a frame function for the internal elements of the eyeball, as well as withstand external mechanical and physical influences. 6 muscles responsible for eye movement are attached to it.
Eye
, an organ for the perception of light stimulation in some invertebrate animals (in particular, cephalopods), all vertebrates and humans.
In most invertebrates, the function of vision is performed by less complex organs of vision, for example compound eyes
.
In vertebrates, the eyeballs are paired, located in the eye sockets of the skull—the orbits—and consist of the eyeballs themselves, or the eyeballs connected through the optic nerve to the brain, and the accessory parts of the eyeballs: the eyelids, the
lacrimal apparatus, and the oculomotor muscles. All vertebrate animals have a common type of structure.
The eyeball has a spherical shape. The central point of the anterior surface is called the anterior pole of the eye, and the point located on the posterior surface, at the origin of the optic nerve, is the posterior pole. The line connecting the poles of G. is taken as the anatomical axis; it coincides with the geometric axis. In the front part of the eye, facing the light, there is a diopter (light refractive) apparatus (a system of refractive media, including the cornea
, a transparent biconvex lens -
the lens
, aqueous humor and the vitreous body that fills the cavity, as well as the ciliary body and the iris, or iris, which serves for accommodation, transmitting the image to the light-sensitive
retina
, or retina.
The wall of the back of the eyeball consists of three membranes that fit tightly together. The outer dense shell - the sclera - has a supporting and protective value; it gives G. its shape, being, as it were, his skeleton. On the anterior open side of the eye, the sclera passes into a thin and transparent cornea. Under the sclera there is a choroid abundantly supplied with blood vessels, the front part of which in the form of a thin plate forms the iris, which has a hole in the middle - the pupil
.
In the tissue of the iris in most vertebrates there are special muscles—the dilator and the sphincter, which, by dilating and constricting the pupil, regulate the entry of light rays into the eye, and the iris, therefore, plays the role of a diaphragm. The color of the iris depends on the pigmentation of the iris, which contains pigment cells—chromatophores—and is visible through the transparent cornea. If chromatophores are absent or the outer layer of the retina is devoid of pigment, then the blood vessels of the choroid are visible through the iris and the iris is red (see Albinism
).
The color of the iris sometimes changes depending on the age, sex, and habitat of the animals (dark color of the iris in many young birds and light in old ones, or milky white color of the iris in young birds and orange-yellow in old ones, for example, in the goshawk). Behind the iris is the ciliary body - an annular ridge containing muscle fibers. The lens bag is suspended from it using the fibers of the ligament of cinnamon. Contraction of the ciliary body causes a change in the curvature of the lens in most vertebrates, that is, accommodation
(adaptation of the eye to distant or near vision).
The inner photosensitive membrane of G. is the retina. At the posterior pole of G. there is a yellow spot; somewhat closer to the midline from it there is an area that is insensitive to light - the blind spot. In this place, nerve fibers from the entire retina are collected, continuing further into the brain in the form of the optic nerve. G. has a number of characteristic features in different classes of vertebrates. In fish, G. are distinguished by a flat cornea and a spherical lens ( Fig. 1
).
A special crescent-shaped process protrudes into the cavity of the eye from the choroid, containing smooth muscle fibers attached to the lens bag. Thus, G.'s accommodation in fish is achieved by moving the lens. The posterior wall of the choroid often contains a special layer of cells filled with crystals of light pigment, the so-called. silver shell. Some fish have a shiny layer - a speculum (tapetum), which reflects light rays back to the retina, which causes the apparent glow of the eyes of some fish in almost complete darkness (for example, in sharks). In some deep-sea fish, the pupils are reduced; in others, they are well adapted for capturing the weak light of the underwater depths—huge, telescopic pupils. In the four-eyed fish
, the pupils are elongated in the vertical direction; The cornea is divided by a horizontal strip into upper and lower sections. When a fish swims on the surface, the upper part of its wing is capable of viewing the air environment, and the lower part is capable of viewing the aquatic environment.
In amphibians, the cornea is distinguished by a large convexity ( Fig. 2
). The iris and ciliary body have underdeveloped muscles; G.'s accommodation is carried out by moving the lens with the help of a special muscle that pulls the lens forward to the cornea, as well as due to the pressure of the ciliary muscle.
In reptiles ( Fig. 3
), excluding hatteria and turtles, and birds (
Fig. 4
), excluding kiwi, a characteristic outgrowth, abundantly supplied with blood vessels, protrudes into the vitreous from the site of entry of the optic nerve, the ridge. The visual apparatus of birds is in many respects superior to that of other animals. The eyeball is very large and has a unique structure, which increases the field of vision. In birds with especially acute vision (vultures, eagles), the eyeball has an elongated “telescopic” shape. There are up to 3 yellow spots in the retina.
The form of mammals is similar to that of amphibians. In aquatic mammals (for example, whales), it resembles the convexity of the cornea and the high refractive index of deep-sea fish. In carnivores, pinnipeds, and cetaceans, the inner surface of the choroid forms, as in a number of fish, a shiny pigment layer—a speculum.
Reduced gases are found in cave fish and amphibians (for example, proteas); in mammals living underground (for example, moles), they are distinguished either by their deep location under the skin, or by the absence of the lens, iris and some layers of the retina. See also Vision
,
Vision organs
.
Lit
.
see under art. Vision
.
Human eye
consists of the eyeball (actually the eyeball), connected by the optic nerve to the brain, and auxiliary apparatus (eyelids, lacrimal organs, and muscles that move the eyeball).
The shape of the eyeball ( Fig. 5
) has a not entirely regular spherical shape: the anterior-posterior size in an adult is on average 24.3
mm
, vertical - 23.4
mm
and horizontal - 23.6
mm
;
the size of the eyeball can be larger or smaller, which is important for the formation of the refractive ability of the eye - its refraction (see Myopia
,
Farsightedness
).
The walls of the wall consist of three concentrically located shells—outer, middle, and inner. They surround the contents of the eyeball - the lens, vitreous body, intraocular fluid (aqueous humor). The outer shell of the eye is the opaque sclera, or tunica albuginea, occupying 5/6 of its surface; in its anterior section it is connected to the transparent cornea. Together they form the corneal-scleral capsule of the eye, which, being the most dense and elastic outer part of the eye, performs a protective function, constituting a kind of skeleton of the eye. The sclera is formed from dense connective tissue fibers, its thickness is on average about 1 mm
.
The sclera is greatly thinned in the region of the posterior pole of the optic nerve, where it turns into a cribriform plate through which the fibers that form the optic nerve pass. In the anterior part of the sclera, almost at the border of its transition into the cornea, there is a circular sinus, the so-called. Schlemm's canal (named after the German anatomist F. Schlemm, who first described it), which is involved in the outflow of intraocular fluid. In front, the sclera is covered with a thin mucous membrane - the conjunctiva, which posteriorly passes to the inner surface of the upper and lower eyelids. The cornea has an anterior convex and posterior concave surface; its thickness in the center is about 0.6 mm
, at the periphery - up to 1
mm
.
In terms of its optical properties, the cornea is the strongest refractive medium of the eye. It is also like a window through which rays of light pass into the eye. There are no blood vessels in the cornea; its nutrition is carried out by diffusion from the vascular network located at the border between the cornea and sclera. Thanks to numerous nerve endings located in the superficial layers of the cornea, it is the most sensitive outer part of the body. Even a light touch causes a reflexive instant closing of the eyelids, which prevents foreign bodies from entering the cornea and protects it from cold and heat damage. Directly behind the cornea is the anterior chamber of the eye - a space filled with clear liquid, the so-called. chamber moisture, which is close in chemical composition to cerebrospinal fluid
.
The anterior chamber has a central (average depth of 2.5 mm
) and peripheral sections - the angle of the anterior chamber G. This section contains a formation consisting of interwoven fibrous fibers with tiny holes through which chamber moisture is filtered into Schlemm's canal, and from there - into the venous plexuses located in the thickness and on the surface of the sclera.
Due to the outflow of chamber moisture, intraocular pressure is maintained at a normal level. The posterior wall of the anterior chamber is the iris; in its center there is a pupil - a round hole with a diameter of about 3.5 mm
.
The iris has a spongy structure and contains pigment, depending on the amount of which and the thickness of the shell, the color of the iris can be dark (black, brown) or light (gray, blue). The iris also contains two muscles that dilate and constrict the pupil, which acts as the diaphragm of the pupil’s optical system; in the light it narrows (direct reaction to light), protecting the pupil from strong light irritation; in the dark it expands (reverse reaction to light). , allowing you to capture very weak light rays. The iris passes into the ciliary body, which consists of a folded anterior part, called the corona of the ciliary body, and a flat posterior part and produces intraocular fluid. In the folded part there are processes to which thin ligaments are attached, which then go to the lens and form its suspensory apparatus. The ciliary body contains an involuntary muscle involved in the accommodation of the eye. The flat part of the ciliary body passes into the choroid proper, adjacent to almost the entire inner surface of the sclera and consisting of vessels of different sizes, which contain about 80% of the blood that enters the eye. The iris, ciliary body, and choroid together make up the middle layer of the gland and are called the vascular tract. The inner shell of the retina is the retina, the perceptive (receptive) apparatus of the retina. According to its anatomical structure, the retina consists of ten layers, the most important of which is the layer of visual cells, consisting of light-perceiving cells—rod and cone cells, which also perform color perception. They transform the physical energy of light rays entering the brain into a nerve impulse, which is transmitted along the visual-nervous pathway to the occipital lobe of the brain, where the visual image is formed. In the center of the retina there is an area of the macula, which provides the most subtle and differentiated vision. In the nasal half of the retina, approximately 4 mm
from the macula, there is the exit point of the optic nerve, forming a disk with a diameter of 1.5
mm
.
Vessels emerge from the center of the optic disc - an artery and a vein, which are divided into branches distributed over almost the entire surface of the retina. G.'s cavity is filled with the lens and vitreous body. The lenticular lens - one of the parts of the diopter apparatus of the eye - is located directly behind the iris; between its anterior surface and the posterior surface of the iris there is a slit-like space - the posterior chamber of the eye; like the anterior one, it is filled with aqueous humor. The lens consists of a bag formed by the anterior and posterior capsules, inside of which are fibers that are layered one on top of the other. There are no vessels or nerves in the lens. The vitreous body - a colorless gelatinous mass - occupies most of the cavity G. In front it is adjacent to the lens, on the side and behind - to the retina. Movements of the eyeballs are possible thanks to an apparatus consisting of 4 rectus and 2 oblique muscles; they all start from the fibrous ring at the apex of the orbit
and, expanding in a fan-shaped manner, are woven into the sclera.
Contractions of individual eye muscles or their groups provide coordinated eye movements. For diseases of G., see Art. Eye diseases
.
L. A. Katsnelson.
In anthropology, the width of the palpebral fissure (the distance between the eyelids), its inclination, and the color of the iris are taken into account. In Mongoloids, the palpebral fissure is narrow and the outer angle of the eye is noticeably higher than the inner one, which is associated with the strong development of the epicanthus
. The palpebral fissure of Caucasians is horizontal and medium-wide, while in Negroid races it is wide. The color of the iris depends on the amount and depth of pigment; this determines the type of its color: dark (dark brown, light brown, yellow), mixed (brown-yellow-green, green, gray-green, gray with a yellow rim around the pupil), light (gray, gray-blue, blue , blue). Dark pigments are mainly possessed by darkly pigmented races; among Caucasians there is a large percentage of light and mixed colors. Gender and age variations in the color of the iris are insignificant; the latter boil down to a weakening of pigmentation.
T. D. Gladkova.
Table of contents
Scleritis - what is it, types of pathology
Many diseases can resemble scleritis, so only a specialist can distinguish them.
Scleritis is an inflammatory process that covers all layers of the outer layer of the eye. There is both unilateral and bilateral damage.
There are two options for classifying the disease: by morphological nature and by the affected department.
Fundamentally, the eyeball is divided by an invisible line, the equator, into two parts. Hence the logical conclusion is that there is:
- Anterior scleritis – the visible part of the sclera is affected.
- Posterior scleritis - inflammation develops in the area of the sclera that is inaccessible to inspection.
The second option is considered more rare and is characterized by a severe course. Note that these conditions can flow into one another with unsuccessful treatment, or the absence of it at all.
Depending on the substrate of the pathology, the following forms are distinguished:
- Nodular - characterized by the presence of one or several affected areas of the sclera in the form of nodules that do not move and rise slightly above its surface, often having a purple color.
- Diffuse – the disease affects large areas on the surface of the eye.
- Necrotic is the most serious type of scleritis. There are two variants of the course: inflammatory, which is a consequence of an advanced process of inflammation, and the second type is primary necrotizing, when destruction of scleral tissue immediately occurs, without a previous inflammatory component.
The nodular form is the most favorable; with adequate treatment, undesirable consequences can be avoided; vision deterioration occurs in 25% of patients.
Sclera
The white membrane of the eye is called the sclera. This is the larger, posterior section of the outer shell, making up about 1/6 of it. The sclera is a direct continuation of the cornea. However, unlike the latter, it is formed by fibers of connective tissue (dense) with an admixture of other fibers - elastic. The white membrane of the eye is also opaque. The sclera gradually passes into the cornea. A translucent rim is located on the border between them. It is called the edge of the cornea. Now you know what the white membrane of the eye is like. It is transparent only at the very beginning, near the cornea.
Causes of scleritis
The disease in the population occurs more often in women 35-40 years of age. This is explained by the high prevalence of rheumatological diseases in this category, which are characterized by damage to connective tissue; they account for 50% of the causes of all scleritis.
Other etiological factors are:
- autoimmune processes (collagenosis);
- systemic vasculitis (Wegener's granulomatosis, periarteritis nodosa);
- infectious diseases (tuberculosis, syphilis, brucellosis, etc.);
- cardiovascular pathology (with Dressler's syndrome, as a complication of myocardial infarction).
Scleritis in the vast majority of cases develops secondary to the presence of a severe background disease, both in the tissues of the eye and in the entire body as a whole.
Possible symptoms
The main group of drip medications is glucocorticosteroids, powerful drugs that will help eliminate severe inflammation of the sclera.
Due to the variety of types and variants of the course, scleritis manifests itself in different ways. Often the signs of the disease are so pronounced that the patient immediately consults a doctor, but sometimes the process may not cause severe discomfort. It all depends on the individual capabilities of the body.
It is customary to divide symptoms into general and local. The general one is observed in many diseases, therefore it is not specific and is characterized by:
- malaise;
- loss of appetite;
- headache.
Since scleritis for the most part develops secondarily, in addition to these symptoms there are usually additional ones caused by the underlying disease.
The second group of signs includes:
- Pain in the eyeball, which can “shoot” into the temporal region, chin.
- Burning, itching in the eye, photophobia.
- Lacrimation is caused by increased afferent impulses of nerve endings.
- Redness of the eye, both diffuse and in a specific area, which is facilitated by the effect of inflammatory mediators on the vessels and their dilation.
- With the nodular form, a purple focus may appear at the site of the pathological process; also, with this type of scleritis, abscesses can form, which most often open with the release of pus.
- A sign of the posterior version of scleritis is difficulty moving the eyes and exophthalmos; also, as it progresses, there may be deterioration in vision due to the development of inflammation in the retina or optic nerve.
Diseases and symptoms
Since the sclera is the outer shell of the eyeball, it is often negatively affected by adverse factors. The tunica albuginea performs a number of important functions, so diseases of this part of the eye can lead to a rapid decrease in visual acuity and even cause blindness. Normally, the scleral formation has a light blue tint, which is more pronounced in childhood.
Read in a separate article: Methods for examining the cornea: microscopy, keratography and others
Any change in the shade of the sclera indicates the presence of pathological conditions. If, as a person grows older, the bright blue color of the shell does not disappear, then a diagnosis of “blue sclera syndrome” is made. This disease is congenital and indicates a violation of the formation of the eyeball in the womb.
Blue sclera is associated with iron deficiency in the body.
Also, the sclera often acquires a yellowish tint. Such changes may indicate liver problems or melanosis, a congenital disease that indicates a disorder in carbohydrate metabolism and manifests itself in early childhood. In old age, yellowness of the membrane may be normal, due to thickening of the pigment layer and accumulation of fats.
In ophthalmology, the following acquired diseases of the sclera are often diagnosed:
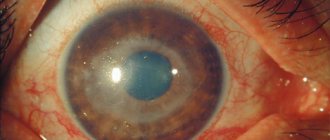
- Scleritis. Inflammation of the sclera, in which all layers of the sclera are affected. Accompanied by pain, tissue swelling and immunodeficiency. If an abscess develops, the eye capsule may rupture.
- Episcleritis. Inflammation of external fibrous tissues, characterized by the appearance of compactions in the form of nodules. Most often observed in women over 40 years of age.
- Staphyloma. Limited distension, characterized by thinning of the sclera and protrusion of the eyeball. Usually occurs as a complication of various destructive eye processes.
- Excavation of the optic disc. Deepening of the nerve disc often develops against the background of glaucoma and neuropathy. It can be both physiological and pathological in nature.
There are other pathologies of the tunica albuginea, which in the absence of timely treatment can lead to serious complications. To avoid serious consequences, you need to detect the problem in time. In general, you should pay attention to the following symptoms:
- soreness;
- sensation of a foreign body, sand;
- excessive tearing;
- increased photosensitivity;
- change in shade;
- scleral injection;
- change in the shape of the eyeball.
Various defects in the structure of the eyeball may also be observed, such as dilatation of blood vessels, protrusion, and so on.
Examination and differential diagnosis
In the absence of adequate therapy, perforation of the sclera may occur - a condition requiring urgent surgical intervention.
Symptoms of the disease develop within two days. It is important to suspect the onset of scleritis as early as possible, without confusing it with another, less dangerous process, and consult a doctor in time.
Scleral damage should be distinguished from:
- Conjunctivitis. It causes inflammation of the mucous membrane of the eye - the conjunctiva, which lines the sclera and the inner surface of the eyelids. A special feature is the feeling of “sand in the eyes”; with bacterial etiology, there is the possibility of a pronounced accumulation of pus in the conjunctival sac.
- Episcleritis. The symptoms are very similar to scleritis, but they bother the patient less, but it is less characterized by deterioration in visual function. To determine an accurate diagnosis, a test is performed with an adrenergic agonist solution, phenylephrine.
- Irita. The inflammatory process is localized in the iris, which is manifested by a change in its color, impaired reaction to light, and a ring-shaped rim of hyperemia around the cornea.
- Iridocyclitis. In addition to the iris, the ciliary body, which is responsible for accommodation, is also affected by changing the curvature of the lens. In addition to the symptoms of iritis, blurred vision occurs.
It should be understood that clinical signs cannot reliably determine the nosological unit; a high-quality examination by an ophthalmologist using instrumental methods will help with this.
In establishing a final diagnosis using additional methods of examining the patient, one should follow the principle from simple and safe to complex, possibly invasive, options for recognizing the disease.
Let's consider diagnostic methods:
- medical history and visual examination of the eye;
- visometry;
- ophthalmoscopy;
- biomicroscopy – through a slit lamp you can examine in detail the elements of the anterior sclera;
- coherence tomography and ultrasound will provide information about posterior scleritis;
- smear and biopsy - can be used in cases of unclear and protracted course of the process that is difficult to treat.
Prevention
To prevent scleritis, you need to monitor your health and treat infectious and autoimmune diseases in a timely manner. It is recommended to undergo a medical examination every six months by specialized specialists, including an ophthalmologist, immunologist, and rheumatologist.
Inflammation of the sclera of the eye causes significant discomfort to a person. The disease does not go away on its own; a delayed visit to the doctor increases the risk of complications.
Timely comprehensive treatment and compliance with specialist recommendations will help preserve vision.
Author of the article: Mager Irina Yuryevna, specialist for the website glazalik.ru Share your experience and opinion in the comments.
Treatment of scleritis
There are fundamentally two approaches to therapy: medication and surgery. The first is used more often, while the second is used for unfavorable outcomes or complex forms of pathology, for example necrotic.
Medication method
Taking drugs orally is no less important than local drip installations, especially with concomitant systemic pathologies.
With this treatment option, there are also two types of drugs taken, they are distinguished by the method of administration: internal - oral/parenteral, and external - intraconjunctival.
The following groups of drugs for oral administration are distinguished:
- Antibiotics: aminoglycosides (Gentamicin, Streptomycin), fluoroquinolones (Ofloxacin, Levofloxacin, Ciprofloxacin).
- Cytostatics suppress the body's immune response. Use: chlorethylamines (Cyclophosphamide, Melphalan), folic acid antagonists (Methotrexate).
- Steroids have a pronounced anti-inflammatory effect: Dexamethasone, Prednisolone.
- Nonsteroidal anti-inflammatory drugs: Diclofenac, Indomethacin, Meloxicam.
The second group of drugs, for local use:
- Steroids. They come in the form of ointments (Hydrocortisone-POS) and drops (Diprospan, Dexapos).
- Drip antibacterial drugs: Tobradex, Miramistin, Maxitrol.
- Enzyme agents help speed up the process of lysis of necrotic masses: Lekozim, Papain, Protolysin.
- Narcotic analgesics for severe pain: Ethylmorphine.
- Mydriatics, in case of iridocyclitis: Mezatone, Atropine.
Most of the listed drugs have a very powerful effect, so it is strictly forbidden to use them without the prescription of an appropriate specialist.
You need to understand that scleritis therapy alone is not enough. Treatment of both the main disease involved in the pathogenesis of scleral damage and concomitant pathologies is within the competence of doctors of individual profiles and the patient should receive adequate attention to it.
Surgical method
It is often used when a process is running. For example, when inflammation deeply affects the scleral tissue and a transplant from a donor is necessary. Also, when the infection spreads to the cornea, with the aim of replacing it, when the light transmission function is impaired. Another option for intervention is the formation of an abscess, which must be opened.
We also note that surgery is often indicated for complications of scleritis, which we will indicate below.
Complications and prevention
If the doctor recommends surgery, do not hesitate, intervention when the process is advanced is fraught with a large number of postoperative complications.
Severe course, serious concomitant pathology, untimely treatment - all this contributes to the development of complications. As is already clear from the article, scleritis is not a simple disease, with serious medications in the therapy program. Accordingly, complications are no less dangerous:
- Keratitis.
- Abscessation of the lesion.
- Iridocyclitis.
- Staphyloma.
- Cloudiness of the cornea and/or vitreous.
- Retinal detachment.
- Swelling of the macular area.
- Astigmatism.
Among the primary prevention measures, it is important to note the treatment of concomitant, underlying pathology, be it rheumatological, systemic or other diseases, without waiting for damage to the sclera. Secondary prevention is aimed at preventing complications and involves promptly contacting an ophthalmologist when the first signs of scleritis appear and following all prescriptions and recommendations in full.
To summarize, we note that scleritis, although rare, is a serious disease that needs to be given more attention. Therapy for scleritis may include drugs with increased toxicity, so it is important to use preventative prescriptions.
You will find a lot of useful information from an ophthalmologist about the causes, symptoms and treatment of scleritis in this video:
Varieties of scleritis
Scleritis of the eye is classified according to the depth of damage to the membrane and the extent of inflammation. There are the following types:
- Episcleritis - damage to the upper loose layer of the sclera is observed.
- Scleritis - inflammation covers all layers of the membrane.
- Diffuse scleritis - the disease spreads to large areas of the eyeball.
- Nodular - the focus of inflammation is limited, located between the equator and the limbus of the eye, looks like a reddened, swollen spot.
The treatment methods used and the duration of treatment depend on the type of disease.