Main symptoms:
- Involuntary eye fluctuations
- Absence of iris
- Increased intraocular pressure
- Corneal opacity
- Photophobia
- Decreased vision
Aniridia is an ophthalmological disease characterized by the complete or partial absence of the iris of the eye. This disease is most often genetically determined and can be transmitted either in an autosomal dominant or autosomal recessive manner. In some cases, the disease is a consequence of a spontaneously manifested mutation.
- Etiology
- Classification
- Symptoms
- Diagnostics
- Treatment
This eye disease does not have a clear division by age and gender. Clinically manifested in decreased visual acuity, photophobia, and horizontal nystagmus.
To make an accurate diagnosis, in addition to a visual examination, certain instrumental examinations are also carried out. Genetic studies are required if a congenital form is suspected. Therapy is based in most cases on the installation of an iris prosthesis.
There is no specific prevention for this eye disease, since it is a genetic pathology. Provided that all recommendations are followed and therapeutic measures are started in a timely manner, the prognosis will be favorable and there is no threat to life. According to the ICD classification of the tenth revision, the disease is coded Q13.2.
Thiology
The main reason for the development of such a pathology in a child is a mutation in the PAX6 gene, which is localized. It is noted that in 65% of cases the disease is genetically determined, and the pathology is transmitted in two types:
- autosomal recessive; autosomal dominant.
In approximately 35%, the gene mutation is spontaneous, however, in diseases, as well as in general clinical cases, caerthonic diseases.
The absence of the iris can also be caused by external negative factors affecting the visual organ, namely mechanical damage, which results in the separation of the iris from the root.
There are no predisposing external etiological factors regarding this disease. However, if there are cases of the development of such an ophthalmological disease in the family, then before conception you should consult a medical geneticist.
Anomalies and diseases of the choroid (Part 1) | Guide to Pediatric Ophthalmology
Description
Pathology of the choroid in the structure of the general pediatric eye morbidity is about 5%. Congenital anomalies of the choroid, inflammatory diseases of an infectious or toxic-allergic nature, dystrophic processes, tumors and injuries are observed (Table 26).
ANOMALIES OF THE VACUOSUS
Anomalies of the choroid, which are occasionally found in newborns, include: aniridia, coloboma of the iris, ciliary body and choroid, polycoria, ectopia pupil, albinism, aplasia. Only a few of them are of practical importance.
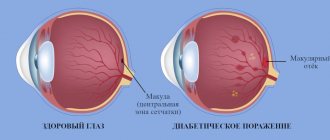
Aniridia. Aniridia
- absence of the iris. In this case, behind the cornea there is a picture of a maximally dilated pupil. Even with lateral lighting, the contours of the lens and ciliary band (ligament of Zinn) are visible. Sometimes the rim is a remnant (rudiment) of the iris root and ciliary processes. The most clear picture of aniridia is with biomicroscopy and examination in transmitted light.
Aniridia leads to constant photophobia. Visual acuity in such children is very low and difficult to correct even with a diaphragm. Nystagmus is often observed. This anomaly is sometimes combined with congenital glaucoma due to underdevelopment or absence of the anterior chamber angle, through which the main outflow of aqueous humor from the eye occurs.
The treatment consists of creating an artificial pupil - a custom-made cosmetic (appropriately colored) contact lens.
Coloboma of the iris.
Congenital coloboma of the iris is located, as a rule, at the bottom - at 6 o'clock, resembling a pear or keyhole; artificial coloboma can have any localization, but more often - at 12 o'clock. Congenital coloboma is almost always incomplete, with an intact pupillary margin visible throughout. There is a relatively lively reaction of the pupil to light.
Possible bilateral involvement
. Vision in an eye with coloboma is usually somewhat reduced. Coloboma can be eliminated surgically, but more often with this pathology a cosmetic contact lens is used. Coloboma of the ciliary body. Coloboma of the ciliary body can only be detected by cycloscopy. An indirect sign of this anomaly is weakening or absence of accommodation. Treatment is futile.
Coloboma of the choroid.
Choroidal coloboma is detected during ophthalmoscopy in the form of a white area of various sizes and shapes with distinct and uneven edges, over which the retinal vessels pass without changing. Coloboma of the choroid, depending on its location, can have a more or less pronounced effect on visual functions (acuity and field of vision). Treatment is futile.
Polycoria.
Polycoria is an abnormality of the iris, characterized by the presence of several pupillary holes in it. Such an anomaly can also occur in the choroid - chorioderemia (white holes, spots). With polycoria, visual discomfort and some loss of vision are observed. Choroideremia is manifested mainly by defects in the visual field, but with central localization of holey zones, a sharp decrease in visual acuity can be observed. Treatment of polycoria consists of performing plastic surgery. Choroideremia cannot be treated.
Pupil correction
. Correctopia is a displacement of the pupil, i.e. its pronounced eccentric location. This anomaly may result in decreased vision. Treatment is only surgical, but the results are sometimes questionable.
It should be noted that the listed anomalies can be combined with other congenital changes of the eye (microphthalmos, microcornea, etc.).
INFLAMMATION OF THE VACUOSUS
Inflammation of the choroid (uveitis) is most often caused by its rich blood supply and slow blood flow, which favors the retention of microbes, viruses and other pathological agents in it.
To a certain extent, separate blood supply to different parts of the choroid: the choroid itself - from the posterior short ciliary arteries, and the iris and ciliary body - from the anterior and posterior long ones, contributes to the fact that the anterior and posterior parts of the choroid can be affected in isolation.
Accordingly, anterior uveitis, or iridocyclitis (iritis and cyclitis separately are rare) and posterior uveitis, or choroiditis, occur. At the same time, and due to the presence of vascular anastomoses between all parts of the choroid, the possibility of the occurrence of their total damage - uveitis, or iridocyclochoroiditis, involving the retina and optic nerve (neurochorioretinitis) in the process - is not excluded.
Endogenous diseases of the choroid can be either metastatic (when an infection enters its vascular fusula) or toxic-allergic (when the body and eye are sensitized). Exogenous uveitis is secondary and occurs only with perforated wounds of the eyeball, corneal ulcers and other corneal diseases after operations.
There are also so-called granulomatous uveitis, in the clinic and pathomorphology of which a specific granuloma can be detected (tuberculosis, syphilis, toxoplasmosis, etc.), non-granulomatous, in which there are no granulomas (influenza, Still's disease, etc.).
According to the course of uveitis, like other eye inflammations, it is advisable to characterize them as acute, subacute, chronic and recurrent. In this case, one should also take into account the pathomorphological features of uveitis, i.e. their exudative, exudative-proliferative, alterative varieties (forms). If we take into account all these factors, the diagnosis of uveitis can be formulated, for example, as follows: bilateral, chronic, anterior, endogenous, exudative-proliferative uveitis (Still's disease).
Naturally, diagnosis should be based on the results of ophthalmological, general clinical, clinical and laboratory studies and anamnestic data.
All children suspected of having uveitis must be urgently hospitalized and examined in an eye hospital. When the diagnosis of uveitis is confirmed, all children should be under active clinical supervision and, if necessary, receive preventive, anti-relapse treatment either in an eye institution or in a specialized dispensary.
Iridocyclitis
(anterior uveitis) are characterized, as a rule, by the following cardinal symptoms: pericorneal injection, change in iris color, constriction of the pupil, change in its shape, slower reaction of the pupil to light, the presence of polymorphic precipitates on the endothelium of the cornea or exudate (hypopyon, hyphema) in the anterior chamber, posterior commissures (fusion of the pupillary edge of the iris with the anterior capsule of the lens). Patients may complain of eye pain and decreased visual acuity (in older children).
When palpating the eye, pain may be noted. Depending on the severity, severity, duration, form and etiology of the process, the clinical picture of iridocyclitis can be different and the listed symptoms are not always found in it.
It should be noted that pain can be not only in the eye, but also in the same half of the head. They are accompanied by reflex lacrimation, photophobia, and blepharospasm. In young children, pain syndrome is usually mild or completely absent.
As a result of exudation, cloudiness of the moisture in the anterior chamber occurs, and pus appears in it. The hypopyon usually descends to the bottom of the chamber and settles as a yellowish horizontal stripe. Hyphema appears in the hemorrhagic form of anterior uveitis and is characterized by a horizontal red stripe.
Precipitates, as a rule, consist of lymphocytes, macrophages, plasma cells, and pigment “dust” freely floating in the chamber moisture. All these elements stick together and settle on the posterior epithelium of the cornea. Precipitates can be of different sizes and shapes, with clear or blurred edges. Most often, precipitates are located in the lower part of the cornea in the form of a triangle with the base downwards, but they can also cover its entire posterior surface.
Changes in the iris occur due to vasodilation and inflammatory edema. This, combined with a reflex spasm of the sphincter of the pupil, leads to its narrowing and slower response to light. Due to the phenomena of exudation from the vessels of the iris, its color and pattern change. Posterior adhesions of the iris arise due to the deposition of exudate in the region of the pupillary edge and the anterior surface of the lens (Fig. 112).
These adhesions are isolated or can merge, forming circular adhesions of the pupillary edge of the iris with the lens. If the exudate covers the entire surface of the lens corresponding to the pupil, then pupillary fusion occurs (vescizu). Since this disrupts the nutrition of the lens of the eye, cataracts can develop.
Circular adhesions prevent communication between the anterior and posterior chambers of the eye, thereby increasing intraocular pressure, as a result of which the iris protrudes into the anterior chamber in the form of a roller.
Severe and prolonged cyclitis causes changes in the vitreous body. It becomes cloudy, connective tissue cords can form in it, which leads to a sharp decrease in vision.
Choroiditis
(posterior uveitis) are characterized by the fact that during ophthalmoscopy in the fundus of the eye with granulomatous forms, prominent or flat, single or multiple foci of different sizes, shapes and colors are visible with symptoms of perifocal inflammation (edema and hyperemia). Most often, according to these focal changes (foci), the retina, and often the optic nerve head, is involved in the inflammatory process. The optic disc may be hyperemic and somewhat swollen (papillitis).
The phenomena of choroiditis are always reflected in the state of the visual field, since, according to focal processes, loss occurs in it (micro- and macroscotomas). If inflammatory foci are located in the center of the fundus, then visual acuity decreases down to light perception, and central absolute (dark) or relative (transparent) scotomas appear.
Older children with choroiditis may complain of curvature of objects and dark spots in front of the eyes when looking at white objects. The vitreous body may become cloudy, resulting in poor vision. There is no pain in the eye with choroiditis. The eyes are usually calm, the anterior part of the eyeball is not changed.
The most common causes of uveitis in children can be considered streptococcal and staphylococcal infections, nonspecific infectarthritis, toxoplasmosis, tuberculosis, and rheumatism. Occasionally, influenza uveitis occurs, and even more rarely, syphilitic uveitis.
Strepto- and staphylococcal uveitis. Strepto- and staphylococcal uveitis occurs as a result of infection entering the eye from the paranasal sinuses and teeth through metastasis. This occurs due to the close connection between the circulatory and lymphatic systems of the eyes, paranasal sinuses and teeth.
Uveitis can also develop with furunculosis and frequent sore throats. It is difficult to decide in which case the infection metastasized and in which the allergic component or reflex mechanism played a role. The commonality of the nerve connections of the organ of vision, paranasal sinuses and teeth is important: toxins located in the teeth or sinuses can cause irritation of the endings of the trigeminal nerve.
These uveitis often occur as a diffuse process, involving all parts of the choroid (panuveitis), and odontoten - in the form of iridocyclitis, sometimes with damage to the cornea (plastic or serous keratouveitis). The course of the disease is acute, with pronounced exudation, most often of the serous type.
It is difficult to determine the etiology of strepto-staphylococcal uveitis, since their clinical manifestations are no different from the symptoms of uveitis of other origins. In all cases, you need to pay attention to the condition of the paranasal sinuses, nasopharynx and teeth.
Rheumatoid uveitis. Rheumatoid uveitis is one of the manifestations of juvenile rheumatoid arthritis. Based on materials from the Clinic of Children's Eye Diseases of the II Moscow Medical Institute. N.I. Pirogov, the frequency of uveitis in this disease ranges from 5.5 to 17%, and a different combination of severity and prevalence of articular and ocular processes is noted.
In an acute generalized, systemic process (Still's disease), the eyes are involved in the process in 0.2-0.5% of children, in polyarthritis affecting five or more joints in 8%, and in mono- and oligoarthritis - 25-30%. The disease is 2 times more common in girls. It should be noted that eye damage in the form of uveitis is most often observed in children under 3 years of age (37–56%), somewhat less frequently in preschoolers (17%) and children of primary school age (8%), most rarely in children aged 11– 15 years (12%). In this regard, the diagnosis is often made already in advanced stages of the disease.
With rheumatoid uveitis, a sharp decrease in visual acuity occurs. On the cornea, corresponding to the palpebral fissure, a ribbon-like gray opacification with bays of clearing is detected. Vessels from the limbus are not suitable for clouding. On the endothelium of the cornea, deposits of “dry”, gray, different-sized precipitates are found.
The stroma of the iris is atrophic, its individual vessels, as well as newly formed vessels, are visible. Multiple powerful posterior adhesions of the iris are formed, and fusion and fusion of the pupil often occur. Significant opacities are visible in the lens and vitreous body. The fundus of the eye is usually unchanged. Most often both eyes are affected.
Eye symptoms of Still's disease can occur very early and be the first sign of this disease, when there are no signs of polyarthritis. The earliest manifestations of uveitis are often discovered by chance, during preventive examinations of preschool children. In this case, small dust-like precipitates are determined on the endothelium of the cornea and thin crescent-shaped opacities on the border of the cornea and the internal limbus at 2-4 and 8-10 hours, respectively, of the open palpebral fissure.
Subsequently, these opacities spread and cover the diameter of the cornea in the form of a ribbon 3-4 cm wide. In addition, lump-like deposits with a pearlescent tint can be found in the conjunctiva, also corresponding to the palpebral fissure. Sometimes the process in the cornea can begin with expansion of the limbus and clouding of the cornea in the area of the lower limbus.
The second earliest symptom indicating involvement of the eye in the pathological process is the occurrence of destruction of the vitreous body. Later, the posterior commissures of the iris are formed. At the same time, the lens becomes cloudy, starting from the anterior section (sequential cataract). Visual acuity is reduced to light perception.
Thus, Still's disease is characterized by the classic ocular triad: uveitis, corneal dystrophy, cataract (Fig. 113). It should be noted that the ocular triad may be the only manifestation of Still's disease, i.e., it can occur without symptoms of polyarthritis.
Eye symptoms in the absence of polyarthritis develop relatively slowly and more favorably. Exacerbations and rapid progression of the ocular triad occur with exacerbations of polyarthritis and the addition of common childhood infections, influenza, etc. The diagnosis of this type of collagenosis is established on the basis of the clinical and ophthalmological picture, the results of laboratory immunological studies and determination of the content of acid glycosaminoglycans.
Differential diagnosis must be made with rheumatism and osteoarticular tuberculosis. Ocular manifestations of Still's disease are detected in almost every 5th sick child. With this disease, pediatricians must be especially attentive to the condition of the eyes, since the process in the eyes is very sluggish, but, as a rule, without timely local treatment it ends in blindness.
Eye treatment is carried out against the background of general therapy of the disease. Installations of mydriatics (atropine + scopolamine + adrenaline + heat) are indicated to prevent the formation or rupture of the posterior adhesions of the iris, forced instillation of dimexide, vitamins B, C, PP, E with glucose, dibazol, amidopyrine, novocaine, etc. In the remission stage to improve trophism and resorption of opacities in the cornea, lens and vitreous body are carried out by installing dionin, lidase, protease, papain (lecozyme).
Corticosteroids, oxygen, etc. are prescribed. During the torpid process, drugs are administered parabulbarly - under the conjunctiva, into the episcleral (Tenon's) space, and also suprachoroidally (dexazone). Under the influence of long-term treatment, significant clearing of the cornea occurs, thinning and rupture of many posterior adhesions of the iris, noticeable resorption of opacities in the lens and vitreous body, and as a result, an improvement in central vision occurs.
However, surgical treatment is more often indicated: partial non-penetrating keratectomy, cataract extraction. The outcomes of operations are not always favorable, as the inflammatory process may worsen. Anti-relapse treatment is indicated in an inpatient setting, which is carried out annually.
Rheumatic uveitis
. Rheumatic uveitis is a symptom of the complex syndrome of rheumatism, which is a common infectious-allergic disease. The incidence of uveitis in patients with rheumatism ranges from 3 to 8%.
The development of rheumatic uveitis is promoted by hypothermia, which reduces the body's resistance. The disease can occur outside the acute phase of the rheumatic process, but more often develops against the background of a chronic process, joining the disease of the joints. Uveitis occurs predominantly in children over 3 years of age. It usually begins acutely and flows rapidly.
The disease is characterized by a sharp mixed injection of the eyeball, hemorrhages in the anterior chamber (hyphema), as well as under the conjunctiva. Exudate in the anterior chamber may be gelatinous in nature. Multiple pigmented posterior adhesions of the iris quickly appear, which, unlike those in Still's disease, are relatively easily ruptured under the influence of mydriatics.
Many predominantly small gray precipitates are formed on the corneal endothelium. The iris becomes full-blooded. The lens and vitreous body are rarely involved in the pathological process. The duration of the disease is 17 years - 2 months. Most often both eyes are affected. Relapses of the disease usually coincide with a rheumatic attack.
Treatment of rheumatic uveitis is aimed at relieving the manifestations of the general disease (antibiotics, salicylates, corticosteroids, antihistamines, etc.). Antibiotics and sulfa drugs, corticosteroids, salicylates, mydriatics (preferably scopolamine), as well as agents that accelerate the resorption of precipitates and possible opacities in the vitreous (electrophoresis of potassium iodide, dionine, lidase, aloe, subconjunctival injections of oxygen) are used locally. The outcome of the disease is often favorable.
Toxoplasmosis uveitis.
The disease can be congenital or acquired. The process is localized mainly in the choroid itself and occurs in the form of chorioretinitis. The course of uveitis in young children is almost invisible. The disease is detected during preventive examinations and more often in connection with the development of secondary strabismus.
A characteristic ophthalmoscopic sign of choroiditis in congenital toxoplasmosis is damage to the central part of the choroid proper, combined with changes in the retina. In this case, in the area of the macula there is a light lesion measuring - 72 times the diameter of the optic nerve head, and sometimes more. In the acute stage, the color of this lesion is yellowish-white or whitish-brown. The center of the lesion protrudes into the vitreous body, its contours are vague.
The optic disc is hyperemic, its tissue is cloudy and slightly swollen. Gradually, an atrophic process develops in the lesion and the affected area acquires a white color, its boundaries are clear, it is surrounded by pigment, and individual vessels and clumps of pigment are visible in the center (Fig. 114).
In the acute course of toxoplasmosis uveitis, opacities and exudate in the vitreous body may be observed, resulting in the formation of proliferating strands and minor hemorrhages.
Recurrences of hemorrhages indicate the activity of the process.
Chorioretinitis can occur in an exudative form with retinal detachment, and therefore it must be differentiated from Coats' retinitis. It should be noted that along with changes in the fundus of the eye during toxoplasmosis, congenital pathologies such as mental retardation, hydrocephalus, calcifications in the brain, malignant myopia, ptosis, microphthalmos, cataracts and lenticonus are often observed.
Due to decreased visual acuity, nystagmus and strabismus occur early.
Acquired toxoplasmosis occurs in children of any age, but more often in preschoolers through infection from sick pets (cats, dogs), as well as pigeons, etc. Infection can occur through nutrition (the meat of sick animals), and can also be transmitted by a sick person. The clinical picture of acquired toxoplasmosis uveitis, in contrast to congenital uveitis, is often characterized by a picture of panuveitis, sometimes even with symptoms of conjunctivitis and keratitis.
The process is usually acute, one-sided, and there is an increase in body temperature. In some cases, a relapse of congenital toxoplasmosis uveitis may occur according to the acquired type.
For the diagnosis of congenital and acquired toxoplasmosis, a correctly collected anamnesis is of great importance, while paying attention to the nature of the course of pregnancy and childbirth, the presence of extra-ocular diseases. For the same purpose, the following laboratory and laboratory-clinical research methods are used: complement fixation reaction (FFR), fluorescent antibodies (RFA), passive hemagglutination (RPHA), microprecipitation in agar, blast transformation (RBT) of peripheral blood lymphocytes under the influence of toxoplasmin.
Clinical and immunological diagnostic reactions are a skin allergy test with toxoplasmin, as well as focal tests with intradermal and subconjunctival administration of toxoplasmin.
It is advisable to carry out treatment in three stages.
First, the acute process caused by Toxoplasma invasion is eliminated (chloridine, sulfadimezin, folic acid, corticosteroids), then specific hyposensitization is carried out (toxoplasmin therapy), after which stimulating and absorbing therapy is carried out (oxygen, lidase, dionin, vitamins, papain, lekozyme, microdoses dexazone). As a rule, repeated courses are required under the control of the body's immunological reactions.
Prevention of congenital toxoplasmosis involves treating a pregnant woman who has positive immunological reactions to toxoplasmosis.
Classification
The classification of this congenital type implies division into two - according to the nature of its occurrence and according to the characteristics of the course of the clinical picture.
Thus, according to the tiological factor, two forms of development of this disease are distinguished:
congenital. acquired or traumatic.
Based on the nature of the development of the onic picture, the following forms of development of this ophthalmology are distinguished:
- full; partial; associated with Gillespie syndrome or WRAG.
The clinical picture of the pathological process, in addition to symptoms, will be supplemented by specific signs, the nature of which depends on the form of development of the disease.
Symptoms
The clinical manifestations of the disease depend on the degree of damage to the iris. The frequent combination of aniridia with glaucoma and cataracts worsens the overall prognosis of the disease, which greatly reduces the patient’s quality of life and leads to disability due to progressive blindness.
Additional signs of the disease:
- decreased visual acuity;
- involuntary oscillatory movements of the eyeballs (nystagmus);
- strabismus;
- increased photosensitivity.
Aniridia can be partial, complete, or combined with Gillespie syndrome and WARG syndrome. In the full form of the disease, remnants of the iris root are preserved, but due to underdevelopment of the eyeball, the quality of vision decreases. The partial form of the pathology has less pronounced manifestations of the disease and can proceed for a long time with minor manifestations.
WARG syndrome in combination with aniridia is manifested by the formation of nephroblastoma, genitourinary disorders and obvious mental retardation.
Some patients additionally develop pancreatic diseases and serious abnormalities in kidney function.
Gillespie syndrome occurs in combination with the main symptoms of aniridia and manifestations of mental retardation with cerebellar ataxia.
In some patients, not only vision but also hearing decreases. In severe forms of the disease, children are born with serious developmental defects, brain damage, underdevelopment of the bones of the body and skull, and absence of eyes. In most patients, against the background of photophobia, characteristic changes in appearance occur: the habit of looking from under the brows appears, the palpebral fissure narrows, and pronounced wrinkles appear around the eyes.
Symptomatic
It should be noted that in the associated form with Gillespie syndrome, in addition to ophthalmological signs, other general symptoms are present.
As for disturbances in the functioning of the visual apparatus, here the disturbances should be clinically
severe photophobia. a decrease in quality to the point that a person sees even close-up objects in a blurred manner. Ambyopia – refers to decreased visual acuity in the left eye. nystagmus, that is, involuntary rotation of the eyes like a pendulum. increased intraocular pressure. corneal clouding. pathology of the lens and optic nerve. pathology of the retina.
With the partial development of this ophthalmological disease, the symptoms are almost identical, but the only difference is that the intensity of the manifestation of the disease will not be so pronounced.
If the child has a congenital form that is associated with Gillespie or Wrage syndrome, the general clinical picture will be accompanied by additional symptoms:
- pathological increase in muscles on only one side of the body; Retention of urination, which will lead to acute renal failure and other diseases of the genitourinary system; formation of malignant nephroblastoma; delay in mental and physical development; mental retardation; hearing impairment; drooping of the upper eyelid in relation to the iris by more than 2 mm; pulmonary stenosis; cerebellar ataxia.
In the event that a congenital pathological process occurs in an associated form, the prognosis of a bad case is not due to concomitant serious complications. In addition, diagnostic testing may be required, since the concomitant clinical picture may indicate other diseases, including those of a congenital nature.
“Manifestation of aniridia”
Treatment
The main method of treating aniridia is the implantation of an artificial iris of a suitable shade. The operation is used mainly for congenital forms of the disease. Acquired aniridia is accompanied by a high risk of corneal damage during surgical interventions. Therefore, surgery in this case may be contraindicated.
Due to increased photosensitivity, patients are recommended to use sunglasses when outdoors.
Conservative therapy includes the use of symptomatic remedies that maintain the health of the visual organ and prevent the occurrence of complications. Ophthalmologists prescribe drops based on beta blockers, prostaglandins and other active agents to control intraocular pressure and prevent glaucoma.
Read in a separate article: Coloboma of the iris: what it is, symptoms and treatment
If there are contraindications to surgical treatment, patients are recommended to use contact lenses that hide the absence of the iris. With the help of special moisturizing local products, it is possible to prevent the development of keratopathy, which is accompanied by destruction and clouding of the surface layers of the cornea.
The main task of specialists who treat people with aniridia is to socialize the patient and maintain a decent quality of life. Not so long ago, specialists did not have the opportunity to perform surgical correction of the disease and could only offer the use of contact lenses with light filters. But every year more and more treatment methods appear, including surgery.
Reconstructive surgeries for implantation of the irido-lens diaphragm have become available to patients. Such surgical interventions are still traumatic and can be dangerous for the patient. But in the future, experts plan to improve surgical treatment techniques. Implantation can be carried out through micro-incisions, thereby reducing the degree of trauma and reducing the risk of developing undesirable health consequences.
Diagnostic
In this case (except for the initial examination by a pediatrician) consultation takiltation takiltation narrow-tocypinsnhalasqualification
neonatologist; ophthalmologist; geneticist; surgeon, when it comes to the form used.
The diagnostic program at the initial stage includes a visual examination and determination of family history, as in most cases this is a congenital disease.
In addition, diagnostic measures will include:
- strengthening; gonioscopy; tonometry; refractory; skiascopy; ultrasound biomicroscopy; genetic studies to detect mutations in the PAX6 gene; FISH test for quality education (nephroblastoma).
As for standard laboratory tests, they are carried out only when necessary.
The results of diagnostic measures, as well as the data that were obtained during the initial examination, make it possible to establish an accurate diagnosis, the form of the disease and, therefore, prescribe the correct one.
Chechen
Treatment of aniridia can be carried out using both conservative and radical methods, eumestvegamermegamama.
It should be noted that by surgical intervention in this case it is meant to be carried out to repair a cosmetic defect . However, if a patient is diagnosed with a congenital form with cataracts, then the congenital form with cataracts is diagnosed, and at the same time the diagnosis is made to swallow.
Conservative methods mean the use of medications.
If a patient is diagnosed with high eye pressure, the doctor prescribes special drops.
prostaglandin; beta blockers; carbonic anhydrase inhibitors.
Drops or gel are also prescribed to reduce the risk of developing pathological changes in the region itself.
In addition, people with this disease are strictly prohibited from exposing their visual organs to direct influence. It is necessary to wear dark sunglasses that would completely neutralize the impact.
Complications
Unfortunately, it is impossible to completely eliminate the consequences of this disease, since it is (often) contagious. Provided that therapeutic measures are started promptly and fully on an ongoing basis, the risk of complications can be minimized. However, much will depend on the very form of development of the pathological process. In general, the following complications are likely to develop:
- cataract; glaucoma; retardation in mental and physical development; complete blindness.
Only a doctor can predict the likelihood of developing such complications.